Delivery of In Vivo Acute Intermittent Hypoxia in Neonatal Rodents to Prime Subventricular Zone-derived Neural Progenitor Cell Cultures
Summary
This article describes the methodology for administering short periods of intermittent hypoxia to postnatal day 1-8 mouse or rat pups. This approach effectively elicits a robust tissue level “priming effect” on cultured neural progenitor cells that are harvested within 30 min of hypoxia exposure.
Abstract
Extended culture of neural stem/progenitor cells facilitates in vitro analyses to understand their biology while enabling expansion of cell populations to adequate numbers prior to transplantation. Identifying approaches to refine this process, to augment the production of all CNS cell types (i.e., neurons), and to possibly contribute to therapeutic cell therapy protocols is a high research priority. This report describes an easily applied in vivo “pre-conditioning” stimulus which can be delivered to awake, non-anesthetized animals. Thus, it is a non-invasive and non-stressful procedure. Specifically described are the procedures for exposing mouse or rat pups (aged postnatal day 1-8) to a brief (40-80 min) period of intermittent hypoxia (AIH). The procedures included in this video protocol include calibration of the whole-body plethysmography chamber in which pups are placed during AIH and the technical details of AIH exposure. The efficacy of this approach to elicit tissue-level changes in the awake animal is demonstrated through the enhancement of subsequent in vitro expansion and neuronal differentiation in cells harvested from the subventricular zone (SVZ). These results support the notion that tissue level changes across multiple systems could be observed following AIH, and support the continued optimization and establishment of AIH as a priming or conditioning modality for therapeutic cell populations.
Introduction
The goal of this method is to reproducibly and effectively deliver intermittent bouts of systemic lowered ambient oxygen to neonatal rodents. The rationale for using intermittent hypoxia (IH) to manipulate stem cell biology originates from in vitro cell culture experiments in which O2 content of the growth media is altered. Specifically, when compared to “standard” conditions of 20% O2, extended culture of stem/progenitor cell populations cells in 3% O2 results in increased proliferation, decreased apoptosis and increased neuronal yield1,2.
This group has significant experience with the administration of systemic IH, and has conducted extensive studies on the role of IH in respiratory plasticity3-7. This work, and the recent finding that chronic IH increased neurogenesis in the rodent CNS8-10, forms the basis for the exploration of acute in vivo hypoxia as a preconditioning stimulus (i.e., prior to tissue harvest) on the subsequent culture of neural stem/progenitor cells (NPCs)11. Remarkably, when mouse pups were exposed to a brief (<1 hr) period of acute intermittent hypoxia (AIH), cells that were harvested from the subventricular zone (SVZ) had significantly increased capacity for expansion as neurospheres or adherent monolayer cells. The AIH protocol was also associated with increased expression of a “neuronal fate” transcription factor (Pax6).
Accordingly, in vivo AIH protocols may provide a means to “prime” NPCs prior to culture. For example, applications for this approach could include expanding cell populations prior to transplantation into the injured central nervous system, or simply increasing the neuronal differentiation of cultured cells prior to in vitro experiments. Further, because this is a systemic delivery, any organ, tissue or cell is a candidate for similar study. Therefore, the protocol as written is potentially applicable to a wide range of studies on intermittent oxygen manipulation in small mammals.
There are certain advantages to this approach. In other published work, neonates were treated as a litter with the dam in hypobaric chambers, which allows for chronic dosing, less handling prior to treatment, and maintained maternal contact during treatment9. The current approach bypasses repeated treatments to a breeding female, or the use of a different dam for each experiment. This protocol also allows study of precise litter-matched and age-matched neonates. Representative data demonstrate another key strength of this protocol, namely the rapidity with which AIH, as delivered, elicits a powerful and consistent biological response in neural stem cell biology. This establishes a precedent for this protocol to elicit tissue- and cellular-level biological changes that alter cell biology.
This report will outline the detailed procedures used for exposing rodent pups to AIH as well as the population analysis of SVZ cells grown as neurospheres.
Protocol
NOTE: All animal procedures in this protocol are conducted with the approval of University of Florida Institutional Animal Care and Use Committee (IACUC) and are in compliance with the 'Guide for the Care and Use of Laboratory Animals'.
1. Basic Experimental Set up Before Intermittent Hypoxia Administration
- Expose pups12 to the different gas mixes using a whole-body mouse plethysmograph chambers in much the same manner as adult rodents for other experimental purposes5,13,14. The chambers have a 4 inch diameter (volume = 450 ml), which is of ample size to accommodate 3-4 mouse pups or 1-2 rat pups. Here, AIH protocols are delivered to neonates aged postnatal day 1-8 (P1-P8).
- Use compressed air gas tanks to deliver the 21% “baseline” gas, which maintains chamber oxygenation at 21%. To achieve “relative hypoxia”, use a 10% oxygen/90% nitrogen gas tank.
NOTE: Plastic tubing (3/16” diameter) connects the gas tanks to a flow meter. Thus, the input to the flow meter consists of one tube each for baseline and hypoxia airflow. - Configure the gas tubing as follows.
- Run plastic tubing (1/8” diameter) from the flow meter to a bias flow regulator, which enables flows of 1 L/min to each chamber (i.e., 4 L/min if 4 chambers are used).
- Run plastic tubing (1/8” diameter) from the bias flow regulator to the plethysmography chambers. Airflow at 1 L/min to each chamber is a predetermined flow rate at which gas exchange is deemed to be non-stress-inducing to the animals based on physiological and behavioral observations.
- Seal all unused connections to and from the bias flow unit and all unused openings to the chambers with caps so that no gas flow escapes to other chambers not in use, or out of the plethysmography chambers during the protocol.
- Place the chamber(s) into an incubator prior to putting animals in the chamber to allow equilibration to 37 °C, or body temperature.
2. Calibration of Cycle Times for Intermittent Hypoxia
- Inspect all tubing, between air tanks and flow meter, flow meter and bias flow unit, and bias flow unit and plethysmography chamber(s) for proper connections. The connections are set up as described in Step 1. Verify the connection by a step-wise check of all described lines and closures: e.g., checking unused lines out of the bias flow unit and any chamber openings not in use.
- Connect an ambient O2 sensor with a hand-held O2 meter and then attach the sensor to the plethysmography chamber lid.
- Open both gas tanks and attach one pair of surgical, long handled hemostats insulated with plastic tubing to clamp the off-cycle flow of gas. In this way, only one gas tank at a time is delivering the 1 L/min gas flow per chamber. Clamp the “baseline” gas mix while the “hypoxic” gas mix is delivered to the chamber, and vice versa.
- Record the time required for the chamber O2 to reach the target levels of 10% and return to 21%. Utilize the recorded times for subsequent protocol delivery.
3. Administration of Acute Intermittent Hypoxia
- Inspect all tubing and connections as described in Step 2.1.
- Place neonates in the plethysmography chamber(s) and house the plethysmography chamber lids into the chamber base. Confirm a proper seal to the O-ring seal is as well as closure of any unused chamber connections. These steps are critical to ensuring the appropriate delivery of gas mixes.
- Place the chambers holding the pups to be treated into the 37 °C incubator and close the door. Allow chamber to equilibrate to 37 °C prior to starting the protocol. Maintain control animals at 37 °C in the incubator at room air oxygenation.
- Open both gas tanks and use one pair of surgical, long handled hemostats insulated with plastic tubing to clamp the off-cycle flow of gas. In this way, only one gas tank at a time is delivering the 1 L/min gas flow per chamber.
- Use a hand-held timer to precisely time cycles and to indicate the time to switch the hemostats between tubes, thus resulting in the alternation of gas flow to the chambers.
- Record the completion of each cycle using a treatment log such as the one provided in Figure 1 to mark off all steps in the 2-step, 20 cycle protocol.
- Monitor the incubator temperature at every cycle change to ensure animals are maintained at the designated range (33-35 °C, which is the setting on the incubator that results in 37 °C).
- Closely monitor pup activity throughout the protocol to ensure that animals tolerate cycles without visible distress such as vocalizations, altered level of limb activity or rolling.
4. Isolation and Culture of Stem/Progenitor Cells from the Subventricular Zone
NOTE: The change in neurosphere formation following AIH compared to controls is an example of an endpoint that demonstrates the efficacy of this protocol to elicit tissue- and cellular-level changes.
- To isolate neurospheres forming cells, remove mouse or rat pups from the chamber immediately after AIH is completed. Sacrifice the animals according to IACUC protocols within 30 min of protocol termination.
- Harvest the SVZ tissue, place into neurosphere culture and conduct standard passage and expansion of derivative neurospheres, as previously published in methods chapters15,16 and a separate video protocol8.
Representative Results
The initial experiments, based on historical data, were conducted using 1 min cycle lengths. Based on the subsequent calibrations performed in Step 2 above, it was determined that the O2 level in the chamber was 13% at 1 min post-hypoxia flushing and, that it took a similar time to return to the 21% baseline. However, a 2 min cycle was sufficient to both achieve 10% oxygen and a return to 21% during the “baseline” cycle. Subsequently, 2 min cycle lengths have been used. The protocol duration consisted of 20 cycles alternating between baseline and hypoxia (80 min overall treatment time). A 20 cycle duration was chosen due to previous work showing that such cycle duration is sufficient to elicit changes in respiratory outcome measures11. Using the described set up (Figure 2), neonates subjected to AIH had no apparent adverse events and did not exhibit behaviors suggestive of pain and discomfort during the 80 min protocol. Specifically, no visible apnea was observed, excessive limb or head movements, or vocalizations. Following AIH, subventricular zone-derived neural stem/progenitor cell populations cultured as neurospheres for 14 days (and also as adherent monolayer populations, data not shown) exhibit a nearly two-fold increase in diameter, demonstrating increased expansion within each forming sphere (Figure 3). Cells that are next plated in permissive conditions (i.e., absence of mitogenic factors) yield significantly more beta-3-positive cells (an increase from <10% to >45%) which indicates more extensive neuronal differentiation as compared to cells harvested from normoxic treated (control) pups (Figure 4).
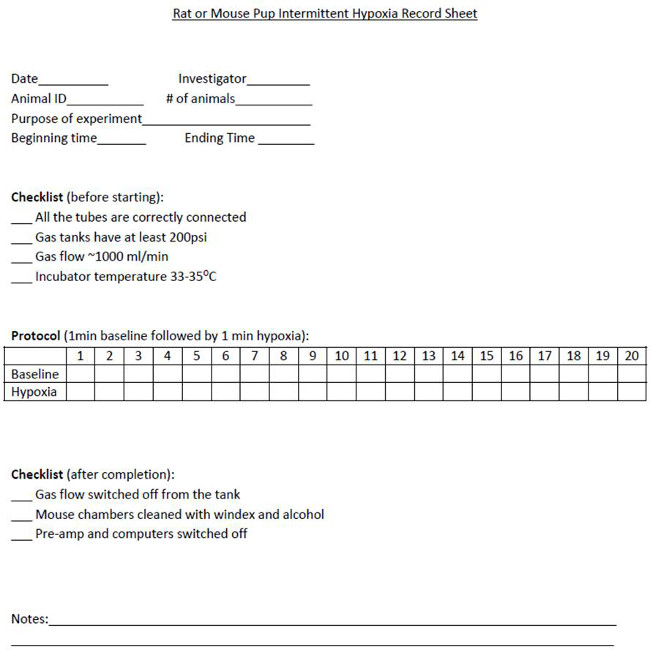
Figure 1. This acute IH record sheet is used to document animal and experimental details, provide a check list for before starting and following completion of the IH protocol, and serve as a tracking document for accurate tally of all completed cycles.
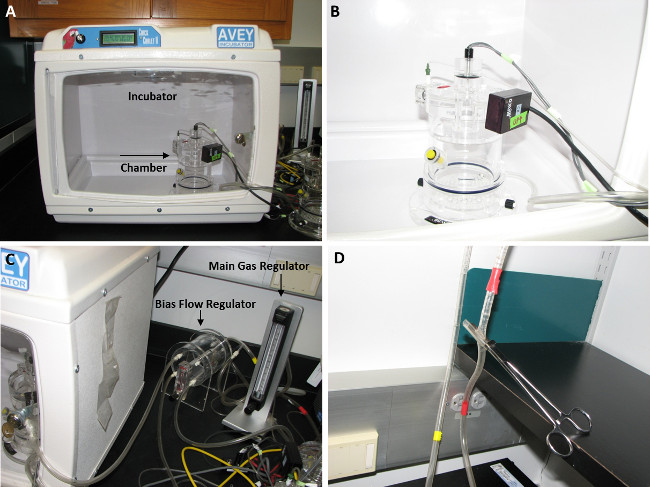
Figure 2. Intermittent hypoxia set up for neonatal rodents. (A) Incubator to maintain environment at 37 °C. Plethysmography chamber is shown within the incubator, and again with the chamber door ajar (B). (C) Right, flow meter adjusted to 1 L/min for each chamber. Gas flow is directed via the bias flow unit splitter unit (center) to any connected chamber (left, within incubator). (D) Hemostat control of baseline (red tape) and hypoxia (yellow tape) input lines. Please click here to view a larger version of this figure.
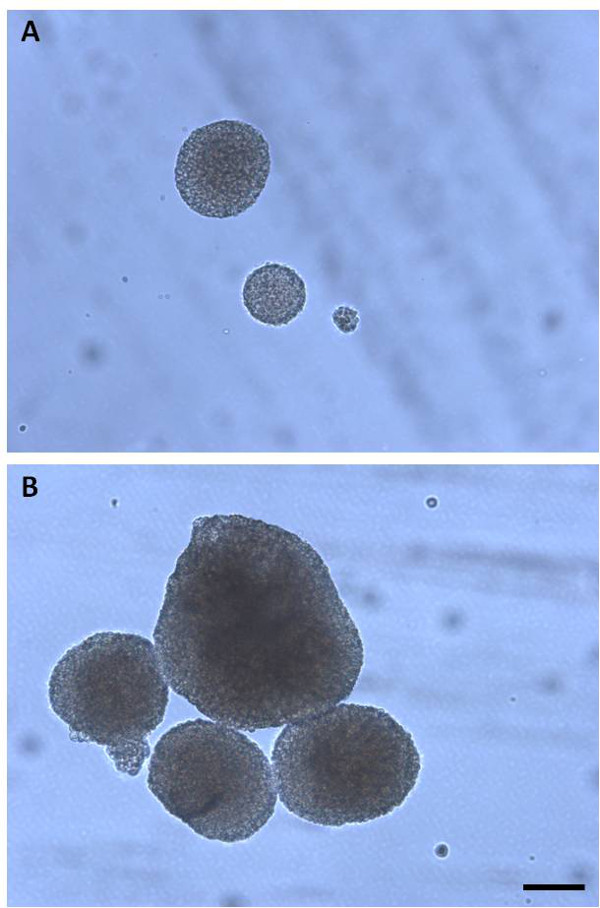
Figure 3. Control neurospheres (A) demonstrate a smaller diameter than AIH neurospheres (B). Images taken at 10X objective, scale bar = 100 µm. Please click here to view a larger version of this figure.
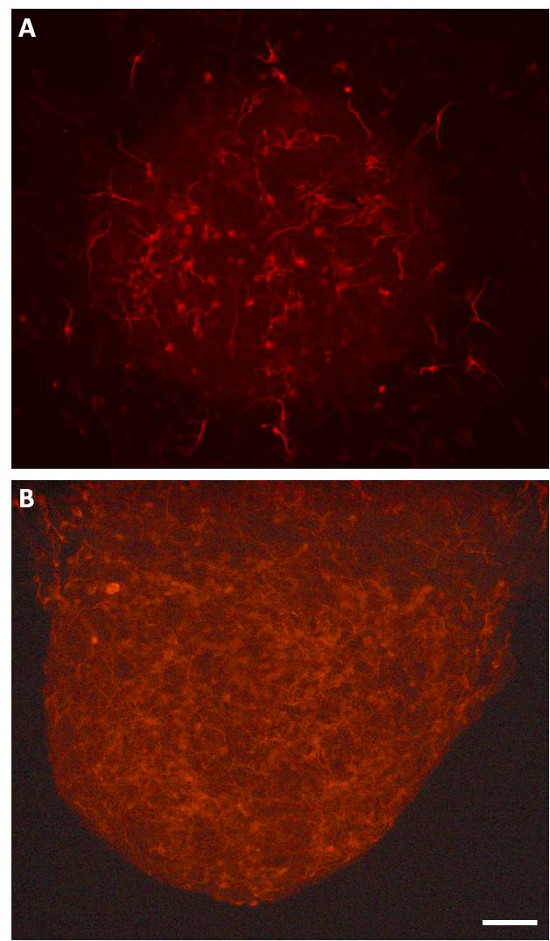
Figure 4. Control neurospheres (A) demonstrate fewer beta-3-tubulin-positive neuroblasts than AIH neurospheres (B). Images taken at 20X objective, scale bar = 50 µm. Please click here to view a larger version of this figure.
Discussion
This work reports the development of a protocol to expose neonatal rodents to AIH. The parameters described here effectively alter in situ neural stem cell biology, which is observable over several rounds of cell passage. Specifically, AIH increases the number of non-adherent neurospheres, the expansion of cells within each neurosphere (refected by sphere diameter), the expansion of adherent NPC populations, and the presence of neuroblasts in both non-adherent and adherent populations. It should be emphasized that the method described herein has been used in multiple trials, and the impact of AIH on in vitro cell biology is robust and reproducible. Over the last several years, more than 60 mouse and rat pups have been exposed to AIH, with increased growth and differentiation observed in each experiment. This is particularly interesting proof of concept, methodological data when considering the development of AIH protocols as a therapeutic modality, for example following neural injury and in conjunction with cell therapies.
During the calibration and delivery of this protocol, precision in several steps is critical to achieve the consistent delivery and cycling of O2 conditions. Therefore, a rigorous pre-treatment protocol is performed to ensure ample gas in both air tanks, proper connections in the entire system—from air tank to plethysmography chamber, precise gas flow into each chamber via air flow regulator checks, and a proper seal on all chambers. Finally, maintaining treatment chambers at a constant temperature ensures that animals are kept as a comfortable body temperature.
One limitation to this method is the lack of a vacuum-based removal of cycling gas, which would decrease the time for each cycle to achieve the limits of the exposure range, thus providing a more rapid method of cycling parameters. Another limitation is that the detailed mechanisms by which this protocol elicit the observed changes is not completely understood, something which this group continues to explore. Prior work demonstrated that HIF1-alpha target genes, EPO and VEGF, appear to be involved in both expansion and morphological changes in these cells11. Further, this report outlined that changes in expansion, in particular, become more pronounced with increased time in culture. This highlights the critical need to carefully document the post-treatment cell culture time course in order to standardize experimental results.
Taken together, these technical results describe a novel application of acute intermittent hypoxia delivered via whole body plethysmography chambers. A significant future application is the continued development of AIH as a non-invasive and powerful tool to encourage the health of both injured CNS tissue and regenerative therapeutic tools such as stem cells destined for transplant.
Declarações
The authors have nothing to disclose.
Acknowledgements
The authors acknowledge funding sources responsible for this work: 5K12HD055929 (HHR), 5R01NS080180-02 (DDF).
Materials
| Name of Material/ Equipment | Company | Catalog Number | Comments/Description |
| Mouse plethysmography chambers | Buxco | PLY4211 | |
| Flow meter | Porter | F150 | |
| Bias flow unit | AFPS | ||
| Baseline Gas Mix | Airgas | AIZ300 | Compressed Air |
| Hypoxic Gas Mix | Airgas | X03NI72C2000189 | 10% Oxygen, balance nitrogen |
| Oxygen Meter | Teledyne | AX-300 |
Referências
- Studer, L., et al. Enhanced proliferation, survival, and dopaminergic differentiation of CNS precursors in lowered oxygen. J Neurosci. 20 (19), 7377-7383 (2000).
- Chen, H. L., et al. Oxygen tension regulates survival and fate of mouse central nervous system precursors at multiple levels. Stem Cells. 25 (9), 2291-2301 (2007).
- Ling, L., et al. Chronic intermittent hypoxia elicits serotonin-dependent plasticity in the central neural control of breathing. J Neurosci. 21 (14), 5381-5388 (2001).
- Mitchell, G. S., et al. Invited review: Intermittent hypoxia and respiratory plasticity. J Appl Physiol. 90 (6), 2466-2475 (2001).
- Fuller, D. D., Zabka, A. G., Baker, T. L., Mitchell, G. S. Phrenic long-term facilitation requires 5-HT receptor activation during but not following episodic hypoxia. J Appl Physiol. 90 (5), 2001-2006 (2001).
- Fuller, D. D., Johnson, S. M., Olson, E. B., Mitchell, G. S. Synaptic pathways to phrenic motoneurons are enhanced by chronic intermittent hypoxia after cervical spinal cord injury. J Neurosci. 23 (7), 2993-3000 (2003).
- Baker-Herman, T. L., et al. BDNF is necessary and sufficient for spinal respiratory plasticity following intermittent hypoxia. Nat Neurosci. 7 (1), 48-55 (2004).
- Zhu, L. L., et al. Neurogenesis in the adult rat brain after intermittent hypoxia. Brain Res. 1055, 1-6 (2005).
- Zhang, J. X., Chen, X. Q., Du, J. Z., Chen, Q. M., Zhu, C. Y. Neonatal exposure to intermittent hypoxia enhances mice performance in water maze and 8-arm radial maze tasks. Journal of neurobiology. 65 (1), 72-84 (2005).
- Zhu, L. L., Wu, L. Y., Yew, D. T., Fan, M. Effects of hypoxia on the proliferation and differentiation of NSCs. Mol Neurobiol. 31 (1-3), 231-242 (2005).
- Ross, H. H., et al. In vivo intermittent hypoxia elicits enhanced expansion and neuronal differentiation in cultured neural progenitors. Exp Neurol. 235 (1), 238-245 (2012).
- Fuller, D. D., et al. Induced recovery of hypoxic phrenic responses in adult rats exposed to hyperoxia for the first month of life. J Physiol. 536 (Pt 3), 917-926 (2001).
- Fuller, D. D., Fregosi, R. F. Fatiguing contractions of tongue protrudor and retractor muscles: influence of systemic hypoxia. J Appl Physiol. 88 (6), 2123-2130 (2000).
- Baker, T. L., Fuller, D. D., Zabka, A. G., Mitchell, G. S. Respiratory plasticity: differential actions of continuous and episodic hypoxia and hypercapnia. Respir Physiol. 129 (1-2), 25-35 (2001).
- Marshall, G. P., et al. Production of neurospheres from CNS tissue. Methods Mol Biol. 438, 135-150 (2008).
- Azari, H., Rahman, M., Sharififar, S., Reynolds, B. A. Isolation and expansion of the adult mouse neural stem cells using the neurosphere assay. J Vis Exp. (45), (2010).

