Establishment of Acute Pontine Infarction in Rats by Electrical Stimulation
Summary
Presented here is a protocol for establishing acute pontine infarction in a rat model via electrical stimulation with a single pulse.
Abstract
Pontine infarction is the most common stroke subtype in the posterior circulation, while there lacks a rodent model mimicking pontine infarction. Provided here is a protocol for successfully establishing a rat model of acute pontine infarction. Rats weighing about 250 g are used, and a probe with an insulated sheath is injected into the pons using a stereotaxic apparatus. A lesion is produced by the electrical stimulation with a single pulse. The Longa score, Berderson score, and beam balance test are used to assess neurological deficits. Additionally, the adhesive-removal somatosensory test is used to determine sensorimotor function, and the limb placement test is used to evaluate proprioception. MRI scans are then used to assess the infarction in vivo, and TTC staining is used to confirm the infarction in vitro. Here, a successful infarction is identified that is located in the anterolateral basis of the rostral pons. In conclusion, a new method is described to establish an acute pontine infarction rat model.
Introduction
Since the 1980s, the middle cerebral artery occlusion (MCAO) model induced by silicone filaments has been widely used in basic stroke research1. Other methods (i.e., suturing of one branch of the MCA2 and photochemically induced focal infarction) have also been used. These models have been termed MCA-based stroke models and have greatly contributed to investigations of the pathophysiological mechanisms underlying stroke and potential therapeutics. Although there are limitations of these experimental models3,4, these methods have been used many labs5,6. MCA-based stroke models represent a stroke in the anterior circulation; however, few reports have investigated models mimicking stroke in the posterior circulation7.
There are significant differences among the etiology, mechanisms, clinical manifestation, and prognosis between anterior and posterior circulation strokes8. Therefore, the results derived from anterior circulation stroke models cannot be applied to posterior circulation stroke. For example, the reperfusion time window for anterior circulation has been extended to 6 h, with a small portion of studies extending to 24 h based on imaging findings9. However, the time window for posterior circulation may be longer than 24 h, according to previous reports10 and our own clinical experiences. This elongated reperfusion time window must be further studied and confirmed in experimental models.
Regarding posterior circulation strokes, pontine infarction is the most common subtype, accounting for 7% of all ischemic stroke cases11,12. According to infarction topography, pontine infarctions are divided into isolated and non-isolated pontine infarctions13. Isolated pontine infarctions are categorized into three types based on the underlying mechanisms: large artery disease (LAD), basilar artery branch disease (BABD), and small artery disease (SAD). Knowledge of the mechanisms, manifestation, and prognosis of pontine infarction has been derived from clinical investigations of cases14. However, a rodent model mimicking pontine infarction has been less investigated.
In previous studies, diffuse brainstem tegmentum injury involving the pons has been explored7. One group attempted to create a pontine infarction model via ligation of the basilar artery (BA)15. Another group used a 10-0 nylon monofilament suture to selectively ligate four points of the proximal BA selectively16. This model mimics LAD, but most pontine infarctions result from BABD and SAD. In addition, selective ligation of the BA is a complicated surgery and has a high death rate.
Provided here is a detailed protocol for an easy-to-perform, easily reproduced, and successful rat model of acute pontine infarction by electrical stimulation.
Protocol
The protocol was reviewed and approved by the Institution Animal Care and Use Committee of The Second Affiliated Hospital of Guangzhou Medical University, an institution accredited by AAALACi. The rats were provided by the Animal Center of Southern Medical University.
1. Animal
- Use adult male Sprague-Dawley rats weighing 250 ± 10 g.
- Upon transport, house the rats for at least 1 week before surgery under controlled environmental conditions with an ambient temperature of 25 °C, relative humidity of 65%, and 12 h/12 h light/dark cycle.
- Provide food and water ad libitum.
2. Establishment of infarction in the pons
- Weigh the rats prior to surgery and assess neurological performance according to the behavioral tests described below (section 3).
- Preheat the heating pad immediately before anesthesia.
- Attach the skull drill to the holder on the stereotaxic frame.
- Intraperitoneally inject the rats with 50 mg/kg ketamine and 5 mg/kg xylazine. Check for the lack of toe-pinch response.
- Mount the rat onto the stereotaxic frame in prone position. Position the ear bars above the ear canal to secure the head. Ensure that the skull is kept horizontal to avoid any skewing of the injection.
- Maintain anesthesia by isoflurane (100% oxygen, 2.5% isoflurane) via a stereotaxic nose cone attachment for rats with inlet and outlet ports. Maintain the temperature at 37 °C using a heating pad and monitor the temperature throughout the procedure.
- Use eye ointment to prevent corneal drying. Use forceps to slightly pinch the paws to ensure that there is no pain response.
- Shave the hair of the skull with a micro-shaver. Apply chlorhexidine surgical scrub in a circular fashion starting at the surgical incision site and rotating outward.
- Make a 3 cm midline incision with a scalpel from the line of the bilateral lateral canthus to 0.5 cm behind the posterior fontanelle, which should be marked by a surgical marker pen.
- Use a cotton swab to remove an blood.
- Place a piece of surgical tape placed on each side of the skin flap to expose the scalp (Figure 1).
- Gently remove the connective tissues from the skull bone with a cotton swab dipped in 0.9% NaCl. If not removed, the connective tissues will get caught in the drill.
- Identify the bregma. Chose the central point of the bregma as the origin point and mark it using a fine-tip black surgical marker pen.
- Place a drill at 6.0 mm AP, 2.0 mm ML (range from 0.5–3.0 mm, Figure 2A).
- Perform craniotomy (1 mm diameter) using an automatic drill. Proceed carefully, because this point is close to the venous sinus.
- Remove the drill from the stereotaxic frame.
- Place a 22 G probe with an insulated sheath in the stereotaxic frame (Figure 3A). The tip of the probe should be placed 2 mm above the proximal end of the sheath (Figure 3A,B; Figure 2B).
- Ensure that the sheath enters the brain 7 mm (7 mm DV, Figure 2B; Figure 1C).
- Advance the probe along the sheath (Figure 1D) until the tip of the probe is 9 mm below the surface of the brain (Figure 2D).
- Connect the electrodes to an electrical stimulator (Figure 3C). Connect the anode to the probe as shown in Figure 1D. Connect the cathode to the rats (usually to the ear of the rats).
- Turn the electrical stimulator on and set up the following parameters: single pulse width = 4,050 ms; voltage = 50 V; and current = 4 mA (Figure 3C). During electrical stimulation, the rat will exhibit trembling. In this study, the device was not turned on for control group rats used for the behavioral tests, MRI, and TTC.
- Leave the probe in position for 5 min after stimulation.
- Remove the probe from the brain (Figure 1F).
- Use bone cement to cover the craniotomy. Allow the cement to dry before wound suturing.
- Suture the wound with 4-0 polyamide suture filaments. After three or four stiches, tie 2-1-1 standard surgical knots.
- Inject the rats with penicillin (0.25 mL, 80 IU diluted in 4 mL of saline) intraperitoneally to prevent infection.
- Inject the rats subcutaneously with meloxicam at a dose of 2 mg/kg and then repeat it every 24 h.
- Monitor the rats every 15 min until fully awake and return them to the cage with a heating pad. Provide free access to food and water until sacrifice.
NOTE: All procedures should follow the aseptic surgical principles. Before the surgery, put on a scrub top, surgical mask and sterile gloves after a surgical scrub of hands. Maintain sterile suture material within the sterile field at all times.
3. Behavioral tests
- Longa score17
- Place the rats on the surface of the table.
- Record scores as follows: 0 = no neurologic deficit; 1 = failure to fully extend contralateral forepaw, a mild focal neurologic deficit; 2 = circling to the left, a moderate focal neurologic deficit; 3 = falling to the left, a severe focal deficit; 4 = no spontaneous walking and a depressed level of consciousness.
- Berderson score18
- Hold the rat by the tail and let the forelimbs reach out for a table. Record the scores as follows: 0 = both limbs reached the table; 1 = only one limb reaches the table.
- Place the animal on a rough surface. Record the scores as follows: 0 = a strong grasp on the rough surface with good resistance when pushed; 1 = a slight resistance only seen in one paw; 2 = no resistance when pushed in one direction.
- Place the rat in an enclosed area (18 in × 36 in) and allow it to roam freely. Record the scores as follows: 0 = walk the entire length of the enclosure without circling; 1 = walk the entire length of the enclosure with circling; 2 = cannot walk the length of enclosure but can circle; 3 = cannot move much. Use the sum of the assessment scores from each task as the final assessment score.
- Balance beam test19
- Ensure that the apparatus consists of a 3 cm wide and 70 cm long beam and is 20 cm above the floor. Place a darkened box at the far end of the beam with a narrow entryway.
- Place a white noise generator and bright light source at the start of the beam. The noise and light were used to motivate the rat to traverse the beam and enter the goal box.
- Terminate the stimuli when the animals enter the darkened box. Record the latency to reach the goal box (in seconds) and hindlimb performance of the rat when traversing the beam.
- Record the scores for each performance as follows: 0 = balances with steady posture; 1 = grasps side of beam; 2 = hugs beam and 1 limb falls off of beam; 3 = hugs beam and two limbs fall off of beam, or spins on beam after >60 s; 4 = attempts to balance on beam but falls off after >40 s; 5 = attempts to balance on beam but falls off after >20 s; and 6 = falls off, no attempt to balance or hang onto beam after <20 s.
- Adhesive removal somatosensory test20
- Place the rats in a clear plexiglass box and allow them to explore the new environment for 2 or 3 min.
- Place a 10 mm diameter green color adhesive label on the inside surface of each forelimb above the thumb and on the wrist.
- Return the rats to the plexiglass box.
- Record the time for the rat to remove the first label and all other labels, respectively. Allow a maximum of 3 min. The test should be conducted 2x in training.
- Limb placement test
- Hold the rats in a horizontal position and prevent movement.
- Once the rat loses contact with table surface (passive limb movement), apply tactile and proprioceptive stimuli to the paw with the table edge.
- Assess the placement of the paw (success or failing) onto the table edge.
- Record the scores as follows: 0 = no placement; 0.5 = unfinished and/or delayed placement; 1 = immediate and complete placement.
4. Infarct confirmation by MRI
- Perform the MRI scan 24 h after surgery.
- Anesthetize the rat by isoflurane (5% for induction, 1%–1.5% for maintenance).
- Secure the rat head in a rat brain array coil and combined with a transmit-only volume coil.
- Place the coil and the rat in the MRI scanner. Secure the rat within the cradle using the tooth and ear bars.
- Maintain body temperature at 37 °C ± 0.5 °C during the MRI scanning procedure using a closed-circuit thermal jacket.
- Use a pilot sequence to ensure correct geometry.
- Collect T2-weighted scans using a fast-spin echo sequence: echo time (TE) = 33 ms; repetition time (TR) = 8,000 ms; field of view = 30 mm x 30 mm; acquisition matrix = 512 × 512; 50 slices; 0.4 mm thick.
- Collect a four-shot spin-echo planar imaging DWI scans: echo time = 30.5 ms; repetition time = 8000 ms; matrix = 96 × 96; field of view = 25 mm x 25 mm; three directions = x, y, z; B values = 0 1,000 s/mm2 and 1,000 s/mm2; 50 contiguous axial slices; 0.4 mm thick.
- Return the rats to the cage.
5. Infarct confirmation by TTC staining
- Sacrifice the rats at the timepoint according to the experimental design. In this experiment, we sacrificed the rats 24 h after surgery.
- Prepare a 2% TTC solution before the sacrifice. Add 0.2 g TTC powder to the 10 mL 0.01 M PBS (pH 7.4). Transfer the dilution to a 10 cm dish covered with silver paper and prewarmed to 37 °C in a water bath.
- Expose the rat to 5% isoflurane until loss of consciousness. Then, expose the rat to CO2 (20%–30% of the volume of the cage per min) until breathing has stopped, then maintain 2 min of CO2 exposure.
- Use the following signs to confirm death: no rising and falling of chest, no palpable heartbeat, poor mucous membrane color, no response to toe pinch, color change or opacity in eyes.
- Perform cervical dislocation.
- Secure the animals by taping the paws on a sterile platform. Create a midline incision from the clavicle to the hypogastrium and a lateral incision from the xiphoid to the left along the ribcage. Make a cut in the diaphragm also along the ribcage and a thorax midline incision to expose the heart.
- Connect the tip of a needle (27 G) to a perfusion pump containing 0.01 M PBS at 4 °C in the left ventricle.
NOTE: Advance the tip along the left edge of the ventricle to avoid entering the atrium. Turn on the perfusion pump to ensure the tip is in the left ventricle and cut the right atrium. If fluid drains out of the nostril, the tip is in the atrium and needs to be adjusted or reinserted. - Use approximately 100 mL of 0.01 M PBS, maintained at 4 °C for perfusion. Turn off the perfusion pump until the liver turns white.
- Decapitate the rats and dissect the whole brains using the scissors and forceps. Remove any water from the brain surface with blotting paper.
- Store the whole brain at -80 °C for 1 min (cutting brain sections is easier after freezing).
NOTE: This step can be skipped if the brain sections can be cut well without freezing. - Place the brain into the matrix with the dorsal side up.
- Identify the hole in the surface of the brain as shown in Figure 1G and insert a stainless steel 0.21 mm thick blade. Usually, the largest area of infarction is in the plane of the probe; thus, one blade should be inserted in this region.
- Insert the other blades at an interval of 2 mm.
- Simultaneously remove the blades, all at once, from the matrix and place the whole brain with the blades in the TTC solution in the dish. Remove the blades carefully.
NOTE: Here, the brain sections were not easily removed from the liquid because some residual pia mater in the basis cranii interfered with sectioning. If any sections remain in the matrix, use a small spatula to transfer them to the dish. - Place the dish with TTC solution and brain sections in a water bath at 37 °C.
- Check the dish every 5 min and ensure no overlap of sections.
- Add 10 mL of 4% paraformaldehyde solution to the dish to terminate the TTC reaction.
- Orient the sections from the rostral to caudal and take pictures.
6. Statistics
- Use statistical analysis software (e.g., GraphPad Prism) to perform a Student’s t-test.
NOTE: All data are expressed as mean ± SE. Differences between groups are determined with two-tailed Student’s t-tests (p < 0.05 defined as statistical significance).
Representative Results
Six animals were subjected to the surgery protocol described above. The control group as shown in the Figure 4 consisted of six rats. The brain slices shown in the Figure 4 were derived from one rat per group.
The MRI scanning showed that the infarction was located in the basis of the pons (Figure 4A). Since the probe was injected 2 mm to the left of the midline, the infarction was located laterally. This infarction mimics anterolateral pontine infarctions in patients (Figure 4A). Because an insulated sheath was used, there was no infarction beyond the tip of the probe including the cortex, cerebellum, and midbrain (Figure 4A). DWI images also revealed the acute pontine infarction (Figure 4A).
TTC staining was used to confirm the infarction 24 h post-surgery (Figure 4A). Compared to the control group, the infarction volume was significantly higher (Figure 4B).
Behavioral scores were measured before and after surgery. The scores for the control and infract model groups before and after surgery are presented in Table 1. Due to the lack of a specific behavioral test designed for pontine infarction, the Longa score, Berderson score, and balance beam test were used to assess the neurological deficits. Additionally, the adhesive removal somatosensory test to assess the sensorimotor function as well as limb-placement test to assess the proprioception.
Compared to the control group, the rats with pontine infarction circled to the left (Figure 4A). There were significant differences in Longa score (2.67 ± 0.52 vs. 0, p < 0.05, Figure 4C), Berderson score (2.67 ± 0.52 vs. 0, p < 0.05, Figure 4D), limb placement test (4.67 ± 0.52 vs. 0, p < 0.05, Figure 4E), beam balance test score (118.33 ± 2.66 vs. 10.17 ± 1.47, p < 0.05, Figure 4F), and adhesive removal somatosensory test score (2.33 ± 0.52 vs. 12.0 ± 0, p < 0.05, Figure 4G) between rats with pontine infarction and control group rats.
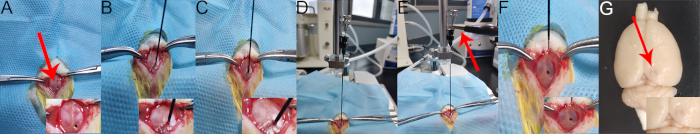
Figure 1: Infarction establishment. (A) A hole made in the skull. (B) The sheath is moved to the hole. (C) Injection of the sheath. (D) Injection of the probe. (E) The anode (red arrow) is connected. (F) The probe is removed. (G) Hole (red arrow) left in the brain surface. Please click here to view this video. (Right-click to download.)
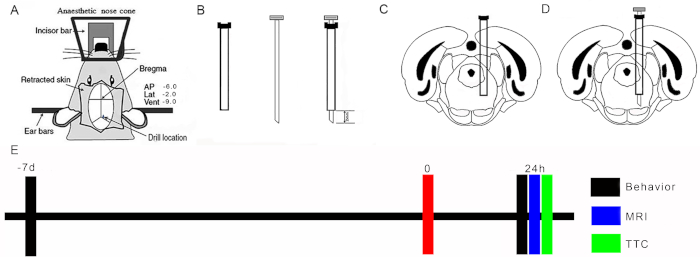
Figure 2: Location of probe. (A) Schematic diagram of stereotaxic locations: arrows point to retraction of skin flaps, site of Bregma, and positioning of drill. (B) Schematic diagram of the sheath and probe. (C) Location of tip of sheath placed in the pons. (D) Location of tip of the probe placed in the pons. (E) Experimental design. Please click here to view this video. (Right-click to download.)
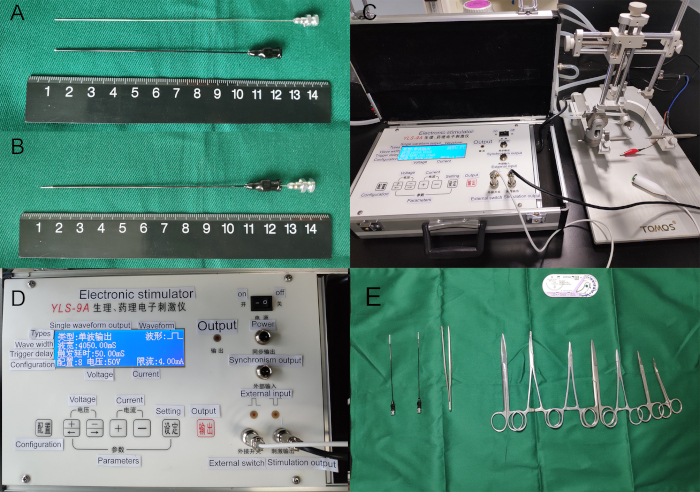
Figure 3: Lesion-producing device. (A) Separate of sheath and probe. (B) The probe in the sheath. (C) The blue electrode was anode which was connected to the caudal probe; the red electrode was cathode. (D) Electrical stimulator. (E) Surgical instruments. Please click here to view this video. (Right-click to download.)
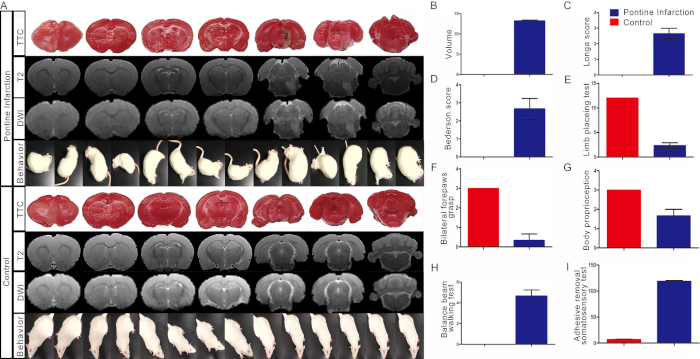
Figure 4: Representative results. (A) The infarction was assessed by MRI scanning with T2 and DWI sequence in vivo and was confirmed by TTC staining in vitro 24 h after surgery. Acute pontine infarction located in the right anterolateral pons (dotted line). Behavioral test showed that the rat circled to the contralateral side of lesion. (B) The volume of infarction. (C) Long score. (D) Bederson score. (E) Limb placing test. (F) Balance beam walking test. (G) Adhesive removal somatosensory test. Bars represent mean ± SD (p < 0.05 vs. control group). Please click here to view this video. (Right-click to download.)
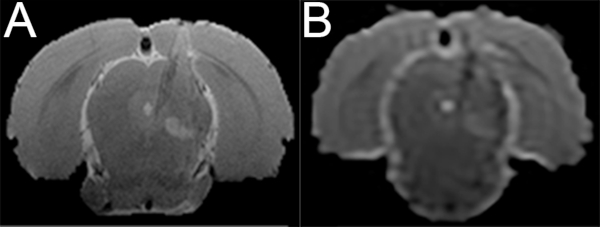
Figure S1: Lacunar infarction in the pons. The length of the probe tip is shortening. MRI scanning shows a lacunar infarction in the right pons. (A) T2 image. (B) DWI image. Please click here to view this video. (Right-click to download.)
| Rat NO | Longa score | Berderson score | Balance beam test | Adhesive-removal somatosensory test | Limb-placement test | |||||
| Pre | Post-surgery | Pre | Post-surgery | Pre | Post-surgery | Pre | Post-surgery | Pre | Post-surgery | |
| Pontine infarction 1 | 0 | 3 | 0 | 2 | 0 | 5 | 6 | 120 | 12 | 2 |
| Pontine infarction 2 | 0 | 2 | 0 | 3 | 0 | 4 | 8 | 120 | 12 | 3 |
| Pontine infarction 3 | 0 | 3 | 0 | 3 | 0 | 5 | 8 | 116 | 12 | 2 |
| Pontine infarction 4 | 0 | 3 | 0 | 3 | 0 | 4 | 6 | 120 | 12 | 2 |
| Pontine infarction 5 | 0 | 3 | 0 | 2 | 0 | 5 | 7 | 114 | 12 | 2 |
| Pontine infarction 6 | 0 | 2 | 0 | 3 | 0 | 5 | 7 | 120 | 12 | 3 |
| Control 1 | 0 | 0 | 0 | 0 | 0 | 0 | 9 | 11 | 12 | 12 |
| Control 2 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 10 | 12 | 12 |
| Control 3 | 0 | 0 | 0 | 0 | 0 | 0 | 10 | 8 | 12 | 12 |
| Control 4 | 0 | 0 | 0 | 0 | 0 | 0 | 7 | 11 | 12 | 12 |
| Control 5 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 9 | 12 | 12 |
| Control 6 | 0 | 0 | 0 | 0 | 0 | 0 | 9 | 12 | 12 | 12 |
Table 1: Behavioral scores.
Discussion
The present study provides a protocol for generating an acute pontine infarction rat model. This model can be used for research on prognosis and rehabilitation (including post-stroke chronic pain) in pontine stroke patients.
There are several strengths of this method. First, it provides a rat model of acute pontine infarction for future studies. As mentioned above, pontine infarction is a common stroke subtype that has received less attention. A major shortcoming of stroke research has been the lack of a specific pontine infarction model. Second, in comparison to the existing pontine infarction rat model by ligation of the BA15,16, this model can be adjusted to alter the location and volume of the infarction according to the experimental design. For example, the length of the tip can be changed so that the infarction extends from the surface of the pons, as done here.
Alternatively, a lacunar infarction in the pons may be established by shortening the length of the probe tip (Supplemental Figure 1). Infarctions in different locations of the pons (i.e., anteromedial pontine infarction) and in different planes of the pons (i.e., upper, middle and lower planes) may also be created according to the topographic design. In this model, the upper pontine plane was chosen. Third, this model is easy to establish and possesses a high success rate. Ligation of the BA may not produce infarction due to the potential collateral circulation15, but this model establishes the infarction at a high success rate, which is essential for reliable research models.
There are some limitations of this method. First, the infarction in this model is not a real stroke. Stroke is a result of vascular vessel lesions, disturbance of blood contents, or dysfunction of regulation of cerebral blood flow. The infarction is created by a lesion in the pons that does not spontaneously occur. In other words, this model cannot be used to address why the stroke occurs in the pons. Second, this model requires special equipment, such as the lesion-producing device and stereotaxic apparatus.
In conclusion, the findings prove this model’s success in establishing an experimental acute pons stroke model. Based on this novel model, the resulting cell loss and prognosis of acute pontine infarction can be further investigated and allow for future therapeutic developments.
Declarações
The authors have nothing to disclose.
Acknowledgements
This study was financially supported by the National Science Foundation of China (81471181 and 81870933) to Y. Jiang and the National Science Foundation of China (No. 81601011), Natural Science Foundation of Jiangsu Province (No. BK20160345) to J. Zhu and by the Scientific Program of Guangzhou Municipal Health Commission (20191A011083) to Z. Qiu.
Materials
| 4-0 sucture | Shanghai Jinzhong | Surgical instruments | |
| Adhesive tape | Shanghai Jinzhong | Surgical instruments | |
| Animal anesthesia system | RWD | Wear mask when using the system | |
| Bone cement | Shanghai Jinzhong | Surgical instrument | |
| Cured clamp | Shanghai Jinzhong | Surgical instrument | |
| General tissue scissors | Shanghai Jinzhong | Surgical instrument | |
| IndoPhors | Guoyao of China | Sterilization | |
| Isoflurane | RWD | 217181101 | |
| Lesion Making Device | Shanghai Yuyan | Making a lesion | |
| MRI system | Bruker Biospin | Confirmation of infarction in vivo | |
| Needle holder | Shanghai Jinzhong | Surgical instrument | |
| Penicilin | Guoyao of China | Infection Prevention | |
| Probe | Anke | Need some modification | |
| Q-tips | Shanghai Jinzhong | Surgical instrument | |
| Shearing scissors | Shanghai Jinzhong | Surgical instrument | |
| Stereotaxic apparatus | RWD | ||
| Suture needle | Shanghai Jinzhong | Surgical instrument | |
| Tissue holding forcepts | Shanghai Jinzhong | Surgical instrument | |
| TTC | Sigma-Aldrich | BCBW5177 | For infarction confirmation in vitro |
Referências
- Zhu, J., et al. Suppression of local inflammation contributes to the neuroprotective effect of ginsenoside Rb1 in rats with cerebral ischemia. Neurociência. 202, 342-351 (2012).
- Xu, X., et al. MicroRNA-1906, a Novel Regulator of Toll-Like Receptor 4, Ameliorates Ischemic Injury after Experimental Stroke in Mice. Journal of Neuroscience. 37, 10498-10515 (2017).
- McBride, D. W., Zhang, J. H. Precision Stroke Animal Models: the Permanent MCAO Model Should Be the Primary Model, Not Transient MCAO. Translational Stroke Research. , (2017).
- Liu, F., McCullough, L. D. Middle cerebral artery occlusion model in rodents: methods and potential pitfalls. Journal of Biomedicine & Biotechnology. 2011, 464701 (2011).
- Jiang, Y., et al. A new approach with less damage: intranasal delivery of tetracycline-inducible replication-defective herpes simplex virus type-1 vector to brain. Neurociência. 201, 96-104 (2012).
- Lopez, M. S., Vemuganti, R. Modeling Transient Focal Ischemic Stroke in Rodents by Intraluminal Filament Method of Middle Cerebral Artery Occlusion. Methods in Molecular Biology. 1717, 101-113 (2018).
- Pais-Roldan, P., et al. Multimodal assessment of recovery from coma in a rat model of diffuse brainstem tegmentum injury. NeuroImage. 189, 615-630 (2019).
- Merwick, A., Werring, D. Posterior circulation ischaemic stroke. The British Medical Journal. 348, 3175 (2014).
- Nogueira, R. G., et al. Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct. The New England Journal of Medicine. 378, 11-21 (2018).
- Wilkinson, D. A., et al. Late recanalization of basilar artery occlusion in a previously healthy 17-month-old child. Journal of Neurointerventional Surgery. 10, 17 (2018).
- Huang, R., et al. Stroke Subtypes and Topographic Locations Associated with Neurological Deterioration in Acute Isolated Pontine Infarction. Journal of Stroke and Cerebrovascular Diseases: The Official Journal of National Stroke Association. 25, 206-213 (2016).
- Jiang, Y., et al. In-stent restenosis after vertebral artery stenting. International Journal of Cardiology. 187, 430-433 (2015).
- Huang, J., et al. Topographic location of unisolated pontine infarction. BMC Neurology. 19, 186 (2019).
- Banerjee, G., Stone, S. P., Werring, D. J. Posterior circulation ischaemic stroke. The British Medical Journal. 361, 1185 (2018).
- Wojak, J. C., DeCrescito, V., Young, W. Basilar artery occlusion in rats. Stroke: A Journal of Cerebral Circulation. 22, 247-252 (1991).
- Namioka, A., et al. Intravenous infusion of mesenchymal stem cells for protection against brainstem infarction in a persistent basilar artery occlusion model in the adult rat. Journal of Neurosurgery. , 1-9 (2018).
- Jiang, Y., et al. Intranasal brain-derived neurotrophic factor protects brain from ischemic insult via modulating local inflammation in rats. Neurociência. 172, 398-405 (2011).
- Schaar, K. L., Brenneman, M. M., Savitz, S. I. Functional assessments in the rodent stroke model. Experiments in Translational and Stroke. 2, 13 (2010).
- Wu, L., et al. Keep warm and get success: The role of postischemic temperature in the mouse middle cerebral artery occlusion model. Brain Research Bulletin. 101, 12-17 (2014).
- Wen, Z., et al. Optimization of behavioural tests for the prediction of outcomes in mouse models of focal middle cerebral artery occlusion. Brain Research. 1665, 88-94 (2017).

