Acute Mouse Brain Slicing to Investigate Spontaneous Hippocampal Network Activity
Summary
This protocol describes the preparation of horizontal hippocampal-entorhinal cortex (HEC) slices from mice exhibiting spontaneous sharp-wave ripple activity. Slices are incubated in a simplified interface holding chamber and recordings are performed under submerged conditions with fast-flowing artificial cerebrospinal fluid to promote tissue oxygenation and the spontaneous emergence of network-level activity.
Abstract
Acute rodent brain slicing offers a tractable experimental approach to gain insight into the organization and function of neural circuits with single-cell resolution using electrophysiology, microscopy, and pharmacology. However, a major consideration in the design of in vitro experiments is the extent to which different slice preparations recapitulate naturalistic patterns of neural activity as observed in vivo. In the intact brain, the hippocampal network generates highly synchronized population activity reflective of the behavioral state of the animal, as exemplified by the sharp-wave ripple complexes (SWRs) that occur during waking consummatory states or non-REM sleep. SWRs and other forms of network activity can emerge spontaneously in isolated hippocampal slices under appropriate conditions. In order to apply the powerful brain slice toolkit to the investigation of hippocampal network activity, it is necessary to utilize an approach that optimizes tissue health and the preservation of functional connectivity within the hippocampal network. Mice are transcardially perfused with cold sucrose-based artificial cerebrospinal fluid. Horizontal slices containing the hippocampus are cut at a thickness of 450 μm to preserve synaptic connectivity. Slices recover in an interface-style chamber and are transferred to a submerged chamber for recordings. The recording chamber is designed for dual surface superfusion of artificial cerebrospinal fluid at a high flow rate to improve oxygenation of the slice. This protocol yields healthy tissue suitable for the investigation of complex and spontaneous network activity in vitro.
Introduction
Electrophysiological measurement from living hippocampal slices in vitro is a powerful experimental approach with numerous advantages. The experimenter can use a microscope, micromanipulators, and a recording system to directly visualize and collect measurements from individual neurons in the tissue. Tissue slices are also very accessible to photostimulation or drug delivery for optogenetic, chemogenetic, or pharmacological experiments.
The hippocampal network generates highly synchronous population activity in vivo, visible as oscillations in the extracellular local field potential1,2,3,4,5. Brain slice methods have been leveraged to gain insight into the cellular and circuit mechanisms underlying these neuronal network oscillations. Foundational work from Maier et al. demonstrated that sharp wave-ripple complexes (SWRs) can emerge spontaneously in slices of the ventral hippocampus6,7. Subsequent studies from multiple investigators have gradually elucidated many aspects of SWRs, including the role of neuromodulators in regulating the network state of the hippocampus8,9,10 and the synaptic mechanisms that drive the in vitro reactivation of neuronal ensembles previously active during behavior in vivo11. Brain slice experiments have also provided insight into the gamma range oscillation (30–100 Hz), a distinct hippocampal network state believed to support memory encoding and recall12,13. Finally, recognizing the central role of the hippocampus and associated structures in the pathophysiology of temporal lobe epilepsy14,15, researchers have used hippocampal slice preparations to investigate the generation and propagation of epileptiform activity. Carter et al. demonstrated that combined hippocampal-entorhinal cortex slices prepared from chronically epileptic animals can spontaneously generate epileptiform discharges in vitro16. Subsequently, Karlócai et al. explored the mechanisms underlying epileptiform discharges in hippocampal slices by using modified artificial cerebrospinal fluid (ACSF) with altered ion concentrations (reduced Mg2+ or elevated K+) or added drugs (4AP or gabazine)17.
Investigators have developed numerous hippocampal slice approaches that differ in key ways: (1) the region of the hippocampus contained in the slice (dorsal, intermediate, or ventral); (2) the presence or absence of extrahippocampal tissues such as the entorhinal cortex; (3) the orientation used to cut slices (coronal, sagittal, horizontal, or oblique); and (4) the conditions under which the tissue is maintained after slicing (submerged fully in ACSF or held at the interface of ACSF and humidified, carbogen-rich air).
The choice of which slicing approach to use should be determined by the experimental objective. For example, transverse or coronal slices of the dorsal hippocampus maintained under submerged conditions have been used very effectively for the investigation of intrahippocampal circuitry and synaptic plasticity18,19,20. However, such preparations do not spontaneously generate network oscillations as readily as slices from the ventral hippocampus21,22,23. Although a state of persistent SWR activity can be induced by tetanic stimulation in transverse slices from the dorsal and ventral hippocampus24, spontaneous SWRs are more readily observed in ventral slices7,25.
An inherent physiological and anatomical distinction between the dorsal and ventral hippocampus is supported by studies performed both in vivo and in vitro26. Recordings in rats revealed strongly coherent theta rhythms throughout the dorsal and intermediate hippocampus, yet poor coherence between the ventral region and the rest of the hippocampus27. SWRs in vivo propagate readily between the dorsal and intermediate hippocampus, while SWRs that originate in the ventral hippocampus often remain local28. The associational projections originating from CA3 pyramidal neurons that reside in the dorsal and intermediate hippocampus project long distances along the longitudinal axis of the hippocampus. CA3 projections originating from ventral regions remain relatively local, and thus are less likely to be severed during the slicing process29,30. Ventral slices may, therefore, better preserve the recurrent network necessary to generate population synchrony. The propensity of ventral slices to generate spontaneous network activities in vitro may also reflect higher intrinsic excitability of pyramidal neurons or weaker GABAergic inhibition in the ventral hippocampus as compared to more dorsal regions31. Indeed, ventral hippocampal slices are more susceptible to epileptiform activity32,33. Thus, many studies of spontaneous physiological8,9,11,24 or pathological16,34,35,36 network oscillations have traditionally used a horizontal slicing approach, sometimes with a slight angle in the fronto-occipital direction, which yields tissue slices parallel to the transverse plane of the ventral hippocampus.
Network connectivity is unavoidably impacted by the slicing procedure as many cells in the slice will be severed. The angle and thickness of the slice and the tissue retained in the preparation should be considered to optimize connectivity in the circuits of interest. Many studies have utilized horizontal combined hippocampal-entorhinal cortex slices (HEC) to explore interactions between the two structures in the context of physiological or pathological network oscillations. Roth et al. performed dual recordings from the CA1 subfield of the hippocampus and layer V of the medial entorhinal cortex to demonstrate propagation of SWR activity through the HEC slice37. Many studies of epileptiform activity have used the HEC slice preparation to investigate how epileptiform discharges propagate through the corticohippocampal network16,35,36,38. It is important to note that preservation of the intact corticohippocampal loop is not a prerequisite for spontaneous SWRs, epileptiform discharges, or gamma oscillations; network oscillations can be generated in transverse slices of the dorsal or ventral hippocampus with no attached parahippocampal tissues21,22,23, 25,39,40,41. A more important factor for the spontaneous generation of network oscillations in hippocampal slices may be the thickness of each slice, as a thicker slice (400–550 μm) will preserve more connectivity in the CA2/CA3 recurrent network21,22,25.
Although angled horizontal HEC slices (cut with an approximately 12° angle in the fronto-occipital direction) have been used to study the functional connectivity of the corticohippocampal loop11,16,34,35,42, such angled preparations are not required for spontaneous network activity43,44,45. However, the use of an angled slicing plane does allow the investigator to selectively make slices that best preserve the transversely-oriented lamellae of either the ventral or intermediate hippocampus, depending on whether a downward or an upward angle is applied (Figure 1). This approach is conceptually similar to that used by Papatheodoropoulos et al., 2002, who dissected each hippocampus free and then used a tissue chopper to create transverse slices along the entire dorsal-ventral axis21. In the light of the aforementioned functional distinctions between the ventral and dorsal-intermediate hippocampus, investigators should consider the anatomical origin of slices when designing experiments or interpreting results. Using an agar ramp during the slicing procedure is a simple way to preferentially produce slices from either the intermediate or ventral hippocampus.
Hippocampal slices can be maintained in either a submerged chamber (with the tissue fully immersed in ACSF), or an interface-style chamber (e.g., Oslo or Haas chamber, with slices covered only by a thin film of flowing media). Interface maintenance enhances oxygenation of the tissue, which promotes neuronal survival and allows for sustained high levels of interneuronal activity. Traditionally, submerged recording conditions use a slower ACSF flow rate that does not provide adequate tissue oxygenation for stable expression of network-level oscillations. In submerged hippocampal slices carbachol-induced gamma oscillations are only observed transiently46,47, while they can be stably maintained in interface recording chambers10,48,49. As such, many studies of complex spontaneous activity in vitro have relied on interface recording chambers to investigate sharp-wave ripple complexes6,7,8,9,10,25,37, gamma oscillations10,13, and epileptiform activity16,38,45,47.
In a submerged-style recording chamber, an immersion microscope objective can be used to visualize individual cells and selectively target healthy-looking cells for recordings. The submerged preparation also allows fine control over the cellular milieu, as submersion facilitates rapid diffusion of drugs or other compounds to the tissue. Thus, a modified methodology in which stable network oscillations are maintained under submerged conditions represents a powerful experimental approach. This approach is exemplified by the work of Hájos et al., in which hippocampal slices recover in a simplified interface-style holding chamber for several hours before transfer to a modified submerged recording chamber with a high flow rate of ACSF (~6 mL/min) to enhance oxygen supply to the tissue12,48,49. Under these conditions, high levels of interneuron activity and stable spontaneous network oscillations can be maintained in a submerged recording chamber. This modified approach allows the investigators to perform visually guided whole-cell patch clamp recordings and characterize the contribution of morphologically identified cell types to carbachol-induced gamma oscillations12. SWRs can also occur spontaneously in submerged hippocampal slices with a fast flow rate of ACSF11,48,49. Maier et al. demonstrated that hippocampal slices that recovered in an interface chamber before transfer to a submerged recording chamber reliably exhibited spontaneous SWRs, whereas slices that recovered submerged in a beaker before transfer to a submerged recording chamber showed smaller evoked field responses, lower levels of spontaneous synaptic currents, and only very rarely exhibited spontaneous SWRs43. Schlingloff et al. used this improved methodology to demonstrate the role of parvalbumin-expressing basket cells in the generation of spontaneous SWRs44.
The following protocol presents a slicing method through which spontaneously active neurons in horizontal hippocampal slices can be recovered under interface conditions and subsequently maintained in a submerged recording chamber suitable for pharmacological or optogenetic manipulations and visually guided recordings.
Protocol
All methods described here have been approved by the Institutional Animal Care and Use Committee at Columbia University (AC-AAAU9451).
1. Prepare solutions
- Prepare sucrose cutting solution for slicing as described in Table 1.
NOTE: After preparing 1 L of sucrose solution, freeze a small amount (approximately 100–200 mL) in an ice tray. These frozen sucrose ice cubes will be blended into an icy slurry (see step 4.3). - Prepare artificial cerebrospinal fluid (ACSF) for recording as described in Table 2.
- Prepare 1 M of NaCl for stimulation pipettes by dissolving 0.05844 g of NaCl in 1 mL of purified water that has been filtered to remove trace metals and other impurities.
NOTE: Sucrose cutting solution and ACSF should be prepared fresh for each experiment.
2. Prepare agar ramp
- Prepare 4% agar (e.g., 2 g of agar in 50 mL of water) by dissolving agar powder into purified water that has been filtered to remove trace metals and other impurities. Heat the mixture in a microwave until it just begins to boil (approximately 30–60 s). Pour the molten agar into a mold and allow it to cool and solidify at 4 °C in a fridge at an approximately 12° incline.
NOTE: For a mold, one can use any glass or plastic container set at an angle, with enough molten agar poured in to form a ramp of 4 cm in length and approximately 0.8 cm in height.
3. Stage the slicing area
- Fill a 400 mL beaker containing a slice recovery chamber with approximately 250 mL of ACSF; place it in a water bath warmed to 32 °C and begin bubbling with carbogen (95% oxygen gas/5% carbon dioxide gas).
NOTE: Fill the recovery beaker with just enough fluid to place the nylon mesh of the holding chamber at the very surface of the solution, so that slices will be held at the interface of the warm solution mixture and the air (Figure 1). Place small pieces of lens paper on the nylon mesh. The slices will lay on top of the lens paper, which can later be used to transfer slices individually to the recording chamber (see step 6.6). - Place a flask with the sucrose solution into an ice bucket to chill and begin bubbling with carbogen.
NOTE: The recovery beaker and sucrose solution should be warmed and chilled, respectively, with carbogen bubbling for at least 30 mins before the mouse is placed in the isoflurane chamber. - Pull out the tray of premade, frozen sucrose solution ice cubes from the freezer and place on the bench to partially thaw.
- Place one half of a clean double-edged razor blade into the microtome and calibrate if necessary. Set aside the other half of the razor blade for use during the dissection.
- Run a carbogen line and temperature probe into the slicing chamber and surround with ice to chill the chamber.
- Prepare a clean bench or table covered with two disposable absorbent pads. Lay out all dissection tools and three pieces of lab tape on the left pad, where the transcardial perfusion will be performed.
NOTE: Dissection tools include small Bonn scissors, dissector scissors, large spatula/spoon, microspatula, scalpel with new blade, spatula, sharp/blunt surgical scissors, large tissue forceps, and small tissue forceps (see Table of Materials). - On the other absorbent pad to the right of the perfusion area, place a circular piece of filter paper into the lid of a 100 mm diameter glass Petri dish. Place the bottom of the Petri dish next to the lid and place a carbogen line into both pieces of the dish.
- Use a razor blade or scalpel to cut a small ramp of agar (approximately 4 cm along the angled surface, 0.8 cm in height, 2 cm in width). Cut off a piece of the ramp from the tall end and reverse it to create a backing block of agar. Use cyanoacrylate adhesive to affix the agar ramp and backing block to the slicing platform and set aside.
NOTE: The backing block of agar helps stabilize the brain during slicing and provides a surface on which to dissect away unnecessary tissues from each slice (Figure 1).
4. Transcardial perfusion
- Suspend a 60 mL capacity syringe as a reservoir for sucrose cutting solution approximately 18 inches above the benchtop (e.g., using a three-pronged swivel clamp on a vertical post). Attach tubing to the bottom of the reservoir, run the tubing through a roller clamp, and connect the other end of the tube to a clean 20 G needle.
- Fill the 60 mL reservoir with approximately 30 mL of chilled sucrose solution and direct a carbogen line into the sucrose reservoir to continually bubble the perfusate.
NOTE: Ensure that the sucrose is flowing through the tubing and needle without any trapped bubbles. The flow rate should be just fast enough to have a steady, continual stream of dripping sucrose from the needle. - Using a blender, crush and blend the frozen sucrose into an icy slurry and use the large spatula/spoon to distribute the slurry.
- Place a small amount of sucrose slurry around the edges of the glass Petri dish lid. Add a small amount of sucrose slurry to the Petri dish bottom.
- Add roughly 20–30 mL of sucrose slurry to the perfusion fluid reservoir, mixing it well with the 30 mL of chilled liquid sucrose until the reservoir contains a mixture of very cold, predominantly liquid sucrose with some remnant frozen solution.
- Place the mouse into a chamber connected to an isoflurane vaporizer. With oxygen flowing at approximately 2 L/min, turn the dial of the vaporizer to deliver isoflurane at 5% concentration and start a timer.
NOTE: Keep this timer going throughout the course of slicing to gauge how quickly the slices are obtained. The procedure should be done as quickly as possible, such that slicing is complete, and tissue is recovering in the interface chamber within 15–20 min of the animal entering the isoflurane chamber. Watch the mouse to ensure a state of deep anesthesia is achieved. After a minimum of 5 min, the mouse should be deeply anesthetized and unresponsive to toe pinches. - Immediately before removing the mouse from the isoflurane chamber, fill the Petri dish lid with chilled sucrose solution to a depth of approximately 3–5 mm and fill the Petri dish bottom with chilled sucrose solution to a depth of approximately 1.0 cm.
- Quickly transfer the mouse to the left absorbent pad and use the 3 pieces of tape to secure the forelimbs and tail. Perform a hindlimb toe pinch to ensure that the mouse is unresponsive before any incision is performed. Using the large tissue forceps and surgical scissors, tent the skin and make a lengthwise incision from the bottom of the sternum to the top of the chest. Using the forceps pull up on the sternum and use the scissors to cut through the diaphragm.
NOTE: The initial positioning of the mouse and first several incisions to sever the diaphragm should be performed as quickly as possible to ensure the mouse does not regain consciousness. To ensure an adequate depth of anesthesia throughout the procedure, a nose cone can be placed on the mouse to deliver isoflurane during the perfusion. - Use the scissors to cut through the rib cage on each side, cutting in one large motion towards the point where the forelimb meets the body. With the forceps, swing the front of the rib cage away and up toward the head, and then fully remove it with a horizontal cut using the large scissors. Hold the heart in place using the large forceps and insert the 20 G perfusion needle into the left ventricle. Once the needle is positioned correctly, the left side of the heart should quickly pale as chilled sucrose solution fills the ventricle.
- Use the small dissector scissors to cut into the right atrium and allow the blood to flow out of the circulatory system. If the incisions are performed correctly, there should be minimal damage to the heart, and it should continue pumping throughout the perfusion.
NOTE: Rolled-up pieces of tissue paper can be used to wick away blood and sucrose solution from the heart and maintain visibility of the perfusion needle during the procedure. - Ensure that the perfusion needle stays in place and does not fall out of the left ventricle. With a proper flow rate and placement, the liver will start to pale to a light tan/beige color with 20–30 s.
- After 30–45 s, use the large scissors to decapitate the mouse. Holding the head in the left hand, push or peel the skin away from the skull. In a well-perfused animal, the skull should be very pale, and the brain should appear a very light pink color (approaching white) through the skull without clearly visible blood vessels.
5. Extract the brain and cut slices
- Using the small Bonn scissors, make two lateral cuts through the skull towards the midline at the front of the skull, near the eyes. Make two additional cuts on either side of the base of the skull.
- Transfer the head to the bottom of the glass Petri dish where it should be mostly immersed in chilled sucrose solution. Use the small Bonn scissors to cut down the midline along the length of the skull, pulling up with the scissors to minimize damage to the underlying brain tissue. Using the small tissue forceps, firmly grasp each side of the skull and swing it up and away from the brain, like opening a book.
- Use the fingers of the left hand to hold the flaps of skull open and insert the microspatula under the brain near the olfactory bulbs. Flip the brain out of the skull into the sucrose and use the microspatula to sever the brain stem. Wash the brain to remove any residual blood, fur, or other tissues.
- Use the large spatula/spoon to transfer the brain to the lid of the glass Petri dish. With the other half of the double-edged razor blade previously set aside, make two coronal cuts to first remove the cerebellum and then the most anterior portion of the brain, including the olfactory bulbs (Figure 1).
- Apply cyanoacrylate adhesive to the agar ramp. Very briefly place the brain onto a piece of dry filter paper using the large tissue forceps and then immediately transfer it to the agar ramp, placing the ventral surface of the brain onto the adhesive.
NOTE: For slices of the intermediate hippocampus, the brain should be oriented with the anterior facing up the slope of the ramp, and the posterior closer to the blade. For slices of the ventral hippocampus, orient the brain with the anterior end pointed down the slope of the ramp, with the posterior end at the top of the ramp, further away from the blade. In either case, the brain should be positioned at the top of the ramp, such that the coronally-cut surface of the brain contacts the agar backing block (Figure 1). - Place the slicing platform with the agar and brain into the slicing chamber of the microtome and completely immerse with chilled sucrose solution. Use the large spatula/spoon to transfer some sucrose slurry to the chamber, stirring to melt any frozen sucrose and rapidly bring down the temperature of the mixture to ~1–2 °C.
NOTE: Watch the temperature gauge throughout the slicing. If the sucrose solution warms above 3 °C, add more slurry and mix to bring the temperature back down. - Cut slices at a thickness of 450 μm with the microtome speed set to 0.07 mm/s. As each slice is freed, use the small tissue forceps and a sharp scalpel to first separate the two hemispheres, and then to cut away tissue until the slice consists primarily of the hippocampus and parahippocampal regions (Figure 1).
- Use a plastic transfer pipette to transfer the slices individually to the interface recovery chamber, ensuring that they are positioned at the interface of the ACSF and the air with only a thin meniscus of ACSF covering the slices. Tightly close the lid of the chamber and allow slices to recover at 32 °C for 30 min.
- After the initial recovery at 32 °C, bring the interface recovery chamber out of the water bath and place on a stirrer set to a slow speed such that the magnetic stir bar promotes circulation of ACSF within the chamber. Allow it to gradually cool to room temperature as the slices recover for an additional 90 min. Ensure that the recovery chamber is continually bubbled with carbogen and do not allow large bubbles to become trapped underneath the slices.
6. Perform local field potential (LFP) recordings of spontaneous activity
- Prepare for LFP recordings by turning on all necessary equipment, including the computer running the acquisition software, the monitor connected to the computer, the stimulators, the micromanipulator, the temperature controller, the microscope light source, the microscope-attached camera, the microelectrode amplifier, the digitizer, and the peristaltic pump. If using a central vacuum system, open the wall valve to prepare the vacuum line that will remove ACSF from the recording chamber.
- Fill the heated reservoir with ACSF, then place one end of the tubing into the 400 mL beaker containing the bubbling ACSF. Turn on the peristaltic pump to direct ACSF from the 400 mL beaker to the heated reservoir, and from the reservoir onward to the recording chamber. Tap or pinch the tubing to release any trapped bubbles.
- Adjust the peristaltic pump to ensure that the ACSF flow rate through the recording chamber is fast (~ 8–10 mL/min). Use a temperature probe to ensure that the ACSF is 32 °C in the center of the recording chamber.
NOTE: If ACSF is delivered to the recording chamber using a peristaltic pump, a high flow rate can result in a significant fluctuation in flow rate. Consistent flow rates can be achieved using a simple pulsation dampener consisting of a series of empty syringes integrated into the tubing (Figure 2). - Prepare stimulation and recording pipettes from borosilicate glass capillaries using a heated filament puller. The puller protocol should be configured to yield pipettes with a resistance of 2–3 MOhm for stimulation or local field potential recording electrodes.
- Fill stimulation pipettes with 1 M NaCl and LFP pipettes with ACSF.
- Briefly clamp the tubing and turn off the pump to pause flow of ACSF. Transfer a slice to the recording chamber using fine forceps to grasp a corner of the lens paper the slice is resting on-the slice will stick to the lens paper. Place the lens paper and slice into the recording chamber with the slice facing down, then “peel” away the lens paper leaving the slice submerged in the recording chamber. Secure the slice using a harp.
NOTE: Harps can be purchased pre-made or made in-lab using a U-shaped piece of stainless steel or platinum and fine nylon filament. - Place a NaCl-filled stimulation pipette in the manual micromanipulator and slowly advance the tip of the pipette into the surface of the slice (e.g., in the stratum radiatum layer) at an angle of approximately 30–45°. Once the tip of the pipette enters the tissue, advance the pipette forward slowly and refrain from large movements in the lateral or vertical direction that could unnecessarily damage axons within the slice. Place the tip of the pipette at least 50–100 μm deep into the slice to avoid cells near the surface that were damaged during slicing.
- Place an ACSF-filled LFP pipette into the pipette holder attached to the motorized micromanipulator. Apply a very light positive pressure using either mouth pressure or a 1 mL syringe connected via a stopcock valve and a short length of tubing to the pipette holder.
NOTE: Position LFP pipettes within the slice in order to record the signals of interest: in the case of sharp wave ripples, one LFP pipette should be placed in the stratum pyramidale (SP) and a second pipette in the stratum radiatum (SR). This configuration allows for simultaneous recordings of the negative sharp-wave in the SR and the high-frequency ripple oscillation in the SP (Figure 3). - Using the micromanipulator slowly advance the tip of the LFP pipette into the region of interest (e.g., the CA1 pyramidal cell layer) at an angle of approximately 30–45°. Place the tip of the pipette at least 50–100 μm deep into the slice to avoid cells near the surface that were damaged during slicing. While advancing the LFP pipette, continually deliver a small voltage test pulse using the acquisition software and watch for a sudden increase in electrode resistance. This may indicate that the pipette has been clogged or pressed up against a cell.
- Once the LFP pipette is positioned in the region of interest, carefully release the positive pressure by opening the valve on the tubing attached to the pipette holder.
- To record the LFP in a second location simultaneously, repeat steps 6.8–6.10 with a second pipette and micromanipulator.
- Use the microelectrode amplifier in the current clamp configuration to record spontaneous activity in the local field potential after using the bridge balance function in the acquisition software to correct for series resistance of the pipette. Spontaneous SWRs will appear as positive deflections in the extracellular potential of the SP layer (Figure 3).
- In order to record evoked field potentials, use the stimulators connected to the digitizer to deliver a short (200 us) square voltage pulse through the NaCl-filled stimulation pipette. Adjust the stimulation voltage dial to evoke a range of response amplitudes.
Representative Results
Presented here are representative recordings from HEC slices prepared as described in this protocol. Following recovery in an interface holding chamber (Figure 1C), slices are transferred individually to a submerged recording chamber (Figure 2B). The recording chamber is supplied with carbogen-saturated ACSF using a peristaltic pump (Figure 2A). The pump first draws ACSF from a holding beaker into a heated reservoir. Carbogen lines are placed into both the holding beaker and the heated reservoir to provide continuous oxygenation of the media. A pulsation dampener, consisting of a series of air-filled syringes, is positioned in between the peristaltic pump and the recording chamber to minimize the fluctuations in flow rate produced by rapid peristalsis. The air pocket in each syringe absorbs the changes in pressure caused by each cycle of the pump, so that the recording chamber receives a smooth and consistent flow of ACSF52,53. An inline heater positioned after the pulsation dampener ensures that the temperature of the ACSF is held at 32 °C as it enters the recording chamber.
In this example, the dual-surface superfusion recording chamber consists of three 3D-printed layers (Figure 2B). The bottom layer has a rectangular cutout to fit a coverslip, secured with vacuum grease. The middle layer contains the bottom half of an elongated oval chamber, with two horizontal supports. Nylon filament is strung across these supports (roughly every 0.5 mm) and secured with cyanoacrylate adhesive. The slice will rest on top of this strung filament. The top layer contains the upper half of the oval chamber along with small wells into which the silver chloride ground pellets can be placed. The elongated oval shape of the chamber is designed to promote fast laminar flow of ACSF.
Figure 3 presents representative recordings from HEC slices prepared according to this protocol. To initially assess slice health, field postsynaptic potentials (fPSPs) are evoked in the stratum radiatum (SR) using a pipette filled with 1 M of NaCl. In healthy slices, electrical stimulation should produce a fPSP with a small presynaptic fiber volley and a large postsynaptic potential with a rapid initial descent (Figure 3B, upper left). In healthy slices, spontaneous sharp-wave ripples (SWRs) are visible as positive deflections in the LFP in the stratum pyramidale (Figure 3B, lower left). In suboptimal slices evoked fPSPs show a large fiber volley and a relatively small postsynaptic potential, and such slices do not show spontaneous SWRs (Figure 3B, right). SWRs in vitro show characteristics consistent with published descriptions: a positive field potential in the SP layer with an overlaid high frequency oscillation, paired with a negative field potential in the SR layer (Figure 3C). A single SWR recorded in CA2 is indicated with an asterisk (Figure 3C, right). SWRs in HEC slices originate within CA2/CA3 recurrent circuits and propagate to CA1. A single SWR observed in the CA2 and CA1 SP layer is indicated with an asterisk (Figure 3D, right). In this representative example, the CA2 SWR (green) leads that in CA1 (blue) by several milliseconds, as shown in the overlay of the SWR envelope (filtered at 2–30 Hz) recorded in each region.
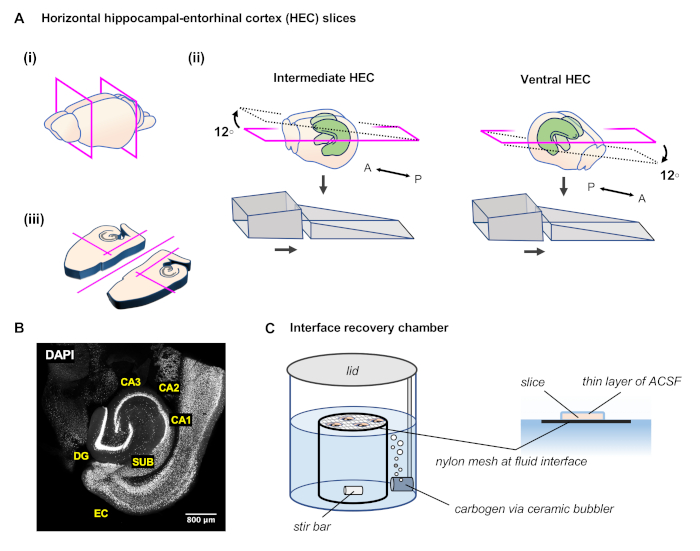
Figure 1: Preparation of horizontal angled hippocampal-entorhinal cortex (HEC) slices. (A)(i) After extracting the brain, perform two coronal cuts with a razor blade to remove the posterior and anterior portions of the brain. (ii) The agar ramp is formed of two angled portions glued to the microtome slicing platform. To prepare slices of the intermediate hippocampus, place the brain block onto the agar ramp with the anterior surface facing up the slope and making contact with the tall backing portion of the ramp. To prepare slices of more ventral hippocampus, place the brain block onto the agar ramp with the anterior surface facing down the slope, so that the posterior cut surface makes contact with the tall backing portion of the ramp. (iii) As each slice is freed, perform several more cuts with the scalpel to separate the hemispheres and remove unnecessary tissue. (B) Representative image of the resulting slice with cell nuclei labeled by DAPI. (C) In an interface recovery chamber, slices are placed on pieces of lens paper on top of a stainless steel or nylon mesh, level with the surface of the ACSF. A ceramic bubbler conveys carbogen into the chamber and a magnetic stir bar continually mixes the fluid in the chamber. A thin film of ACSF covers the top surface of the slice, enhancing diffusion of oxygen from the humid carbogen-rich air of the chamber. Please click here to view a larger version of this figure.
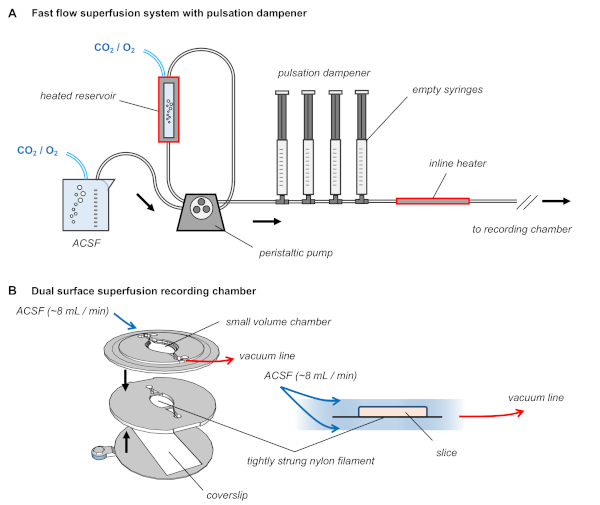
Figure 2: Dual surface superfusion recording chamber with pulsation dampener in the ACSF delivery tubing. (A) Diagram of the superfusion system. ACSF is warmed to 32 ˚C, constantly bubbled with carbogen gas, and delivered at approximately 8–10 mL/min using a peristaltic pump with a pulsation dampener consisting of a series of air-filled syringes. (B) The recording chamber consists of three 3D-printed layers, the middle of which is strung with nylon filament. The slice rests upon this strung filament and ACSF flows above and below the tissue. Please click here to view a larger version of this figure.
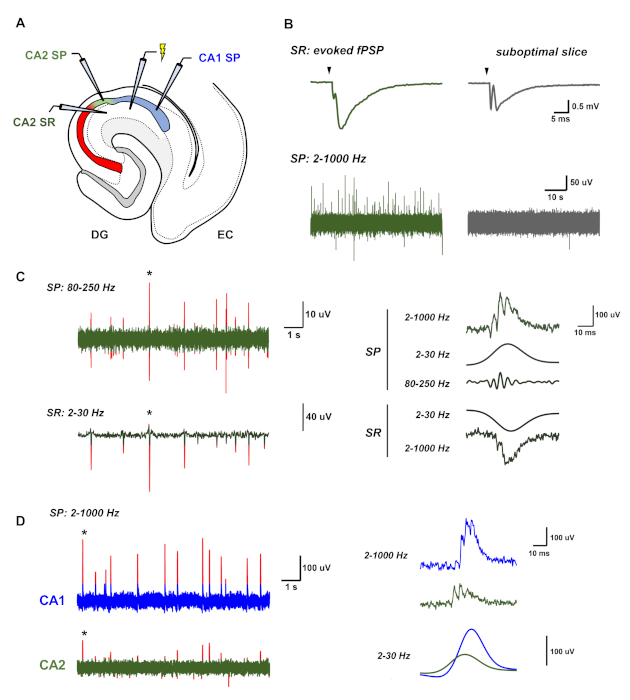
Figure 3: Representative recordings of spontaneous sharp-wave ripples from HEC slices. (A) A simplified diagram of the HEC slice showing the positions of the recording and stimulation electrodes. (B) Representative recordings of LFP activity from both an active, healthy slice and a suboptimal slice. The healthy slice (left, in green) shows large evoked field responses and spontaneous sharp-wave ripples (SWRs), visible as irregularly occurring positive deflections in the local field potential of the SP layer. In contrast, an unhealthy slice shows small evoked field responses and no spontaneous activity (right, in gray). (C) Representative recordings of SWRs in the CA2 region, consisting of a negative deflection in the LFP in the SR layer and a high frequency oscillation with an underlying positive deflection in the LFP in the SP layer. Peaks in each channel greater than three standard deviations of the signal amplitude are highlighted in red. A bandpass filter of 2–30 Hz isolates the underlying positive and negative envelope of the sharp wave in the SP and SR layer, respectively, while a bandpass filter of 80–250 Hz is used to isolate the high-frequency oscillation of the ripple in the SP layer. (D) SWRs in vitro propagate from CA2/CA3 to CA1. In these representative recordings, SWRs in CA2 (green, bottom) precede that in CA1 (blue, top) by several milliseconds. Peaks in each channel greater than three standard deviations of the signal amplitude are highlighted in red. Please click here to view a larger version of this figure.
| molecular weight (grams / mol) | final concentration (mM) | grams / 1 L sucrose cutting solution | ||
| sucrose | C12H22O11 | 342.3 | 195 | 66.749 |
| sodium chloride | NaCl | 58.44 | 10 | 0.584 |
| glucose | C6H12O6 | 180.08 | 10 | 1.801 |
| sodium bicarbonate | NaHCO3 | 84.01 | 25 | 2.1 |
| potassium chloride | KCl | 74.55 | 2.5 | 0.186 |
| sodium phosphate monobasic anhydrous | NaH2PO4 | 137.99 | 1.25 | 0.173 |
| sodium pyruvate | C3H3NaO3 | 110.04 | 2 | 0.22 |
| stock concentration (M) | final concentration (mM) | milliliters / 1L sucrose cutting solution | ||
| calcium chloride | CaCl2 | 1 | 0.5 | 0.5 |
| magnesium chloride | MgCl2 | 1 | 7 | 7 |
Table 1: Composition of sucrose cutting solution. Begin with approximately 0.75 L of purified water that has been filtered to remove trace metals and other impurities. Dissolve each solid while mixing the solution with a magnetic stir bar. Once all solids are dissolved, bubble carbogen gas through the solution for 10 min. Add the MgCl2 and CaCl2 solutions and add water to bring the total volume to 1 L. Mix with a magnetic stir bar for 10 min to ensure the solution is uniformly mixed. The osmolarity should be between 315 and 325 mOsm, and the pH should be approximately 7.4.
| molecular weight (grams / mol) | final concentration (mM) | grams / 2L ACSF | ||
| sodium chloride | NaCl | 58.44 | 125 | 14.61 |
| glucose | C6H12O6 | 180.08 | 12.5 | 4.502 |
| sodium bicarbonate | NaHCO3 | 84.01 | 25 | 4.201 |
| potassium chloride | KCl | 74.55 | 3.5 | 0.522 |
| sodium phosphate monobasic anhydrous | NaH2PO4 | 137.99 | 1.25 | 0.345 |
| ascorbic acid | C6H8O6 | 176.12 | 1 | 0.352 |
| sodium pyruvate | C3H3NaO3 | 110.04 | 3 | 0.66 |
| stock concentration (M) | final concentration (mM) | milliliters / 2L ACSF | ||
| calcium chloride | CaCl2 | 1 | 1.6 | 3.2 |
| magnesium chloride | MgCl2 | 1 | 1.2 | 2.4 |
Table 2: Composition of artificial cerebrospinal fluid. Begin with approximately 1.5 L of purified water that has been filtered to remove trace metals and other impurities. Dissolve each solid while mixing the solution with a magnetic stir bar. Once all solids are dissolved, bubble carbogen gas through the solution for 10 min. Add the MgCl2 and CaCl2 solutions and add water to bring the total volume to 2 L. Mix with a magnetic stir bar for 10 min to ensure the solution is uniformly mixed. The osmolarity should be between 315 and 325 mOsm, and the pH should be approximately 7.4.
Discussion
There are several steps in this slicing protocol designed to promote tissue health and favor the emergence of spontaneous naturalistic network activity: the mouse is transcardially perfused with chilled sucrose cutting solution; horizontal-entorhinal cortex (HEC) slices are cut at a thickness of 450 μm from the intermediate or ventral hippocampus; slices recover at the interface of warmed ACSF and humidified, carbogen-rich air; during recordings slices are superfused with ACSF warmed to 32 °C and delivered at a fast flow rate with dual-surface superfusion in a submerged recording chamber.
Slice health is of paramount importance for the generation of network oscillations in vitro. Young animals will yield more healthy slices, and generally with juvenile or adolescent mice the transcardial perfusion step can be skipped. As animals age, it becomes increasingly difficult to make healthy slices, yet some investigations (such as disease models or longitudinal studies) necessitate the use of adult or aging animals. Dengler et al., for example, used transcardial perfusions in their preparation of HEC slices from pilocarpine-treated chronically epileptic adult mice50. With adult mice, it is beneficial to perform a transcardial perfusion with chilled sucrose cutting solution to cool the tissue, clear blood from the brain, and reduce metabolic activity before removing the brain from the skull51. It is important to note, however, that transcardial perfusions require training to be performed correctly and care must be taken to ensure that the procedure is carried out quickly and in a way that does not pose a risk to animal welfare. When possible, experiments should be designed to use young animals so as to preclude the use of transcardial perfusions. In a suboptimal slice preparation, there will not be enough healthy cells, particularly interneurons, to support ongoing network oscillations. To assess slice health during the experiment, it is useful to first record evoked field potentials (for example, with a stimulation pipette and a recording pipette in the stratum radiatum, SR). In a healthy slice, stimulation in the SR layer will evoke a large field postsynaptic potential (fPSP) with a relatively small presynaptic fiber volley (Figure 3).
The slices produced by this protocol are angled horizontal hippocampal-entorhinal cortex (HEC) slices. Importantly, neither the inclusion of parahippocampal tissue nor the angled cut are necessary for hippocampal slices to spontaneously generate network activities such as SWRs. Indeed, many studies have utilized horizontal or transverse hippocampal slices to interrogate aspects of physiological25,40,41,44 or pathological network oscillations33,38. In this protocol the placement of the brain onto an agar ramp allows the experimenter to selectively produce more slices from either the ventral or intermediate hippocampus (Figure 1), which may be beneficial for experimental objectives that take into account the functional heterogeneity that exists along the longitudinal axis of the hippocampus26,31. If the anatomical origin of the slices is not a factor, then the agar ramp can be excluded and a true horizontal cutting plane will yield slices of the intermediate-to-ventral hippocampus. As each horizontal tissue slice is freed, most extraneous parts of the slice can be removed with three simple cuts, leaving a roughly rectangular slice that contains the hippocampus and some surrounding tissue, including the parahippocampal region (Figure 1). Further dissection can be performed to remove all extrahippocampal tissues, but the inclusion of surrounding tissue is beneficial, in that the slice harp can be easily placed such that the nylon filaments do not rest across the hippocampus proper. As discussed above, the combined HEC slice is also a useful preparation with which to investigate a larger corticohippocampal network in the context of physiological37 or pathological16,35,36,38 network oscillations.
The key factor in this protocol is to optimize oxygen supply to the tissue, both during the recovery phase and during the recordings. Many studies of network oscillations are performed in slices that are transferred directly from the microtome to an interface recording chamber and allowed to recover with continual perfusion of fresh ACSF. After several hours of recovery, recordings can then be performed in the same interface chamber. Thus, slices are held at the interface of ACSF and humid carbogen-rich air for the full duration of the experiment. In the alternative methodology presented in this protocol, slices recover in an interface-style holding chamber for at least two hours before individual slices are transferred to a submerged-style recording chamber with sufficiently fast ACSF flow rates. Slices prepared under these conditions can exhibit stable gamma oscillations12 or spontaneous SWR activity43. Slice recovery in an interface-style holding chamber is a critical step: Maier et al. demonstrated that slices which recover in a beaker completely submerged in ACSF exhibit smaller evoked field potentials, less frequent spontaneous postsynaptic currents, and only rarely produce spontaneous network activity43. Similarly, Hájos et al. demonstrated that fast ACSF flow rates result in a higher frequency of spontaneous inhibitory postsynaptic currents, suggesting improved interneuronal activity49. During the recording period, dual-surface superfusion is not strictly necessary, provided the recording chamber holds a relatively small volume of ACSF delivered at a fast flow rate (at least 6 mL/min)43. The 3D printed recording chamber presented in this protocol (Figure 2B) is a relatively cost effective and a simple option, but there are also commercially available submerged recording chambers designed to hold smaller volumes, promote laminar flow of the media, or provide dual-surface superfusion (in contrast to circular recording chambers, for example, which allow excess dead volume of ACSF).
While this protocol allows one to record network oscillations without the requirement of a traditional interface recording chamber, there are several limitations. Although slices are held in the ACSF-air interface during the recovery period, they do not receive continual perfusion of fresh media as occurs in traditional Haas-style interface recording chambers. Slices must be transferred individually (using fine forceps) from the recovery chamber to the submerged recording chamber. Furthermore, fast flow rates can cause instability and motion artifacts problematic for some recordings, particularly if ACSF is delivered with a peristaltic pump. In order to maintain fast flow rates and minimize mechanical disturbances, a simple pulsation dampener can be integrated into the perfusion system (Figure 2). This pulsation dampener operates using the Windkessel effect52, in which empty syringes contain air pockets that act as elastic reservoirs, absorbing the fluctuating pressure generated by the rollers of the peristaltic pump53. However, incorporation of a pulse dampener can add length to the tubing that delivers ACSF to the recording chamber and impact oxygen supply to the slice. Flow rates should only be as fast as is necessary to yield stable network oscillations, and if a peristaltic pump is used it should ideally be a pump that uses a large number of rollers (> 12) to minimize the pulsation caused by peristalsis, preclude the use of a pulsation dampener, and ensure that the tubing that delivers ACSF to the recording chamber is as short as possible. Recordings performed with fast flow rates also necessitate large volumes of ACSF, which may be problematic if experiments require the addition of valuable or expensive drugs or compounds to the media. Although a dual-surface superfusion chamber requires a specially constructed recording chamber with two fluid inlets to deliver oxygenated media to both sides of the slice, spontaneous network oscillations can be observed with moderate ACSF flow rates48. This protocol utilizes both a fast flow rate (stabilized with a pulsation dampener) and a dual-surface superfusion chamber to improve the likelihood of observing spontaneous activity.
Finally, this protocol has a low yield with regards to the number of slices produced per animal. Horizontal slicing with a thickness of 450 μm yields a small number of HEC slices at the preferred orientation (in which the slice is effectively parallel to the transverse axis of the hippocampus). Of these slices, typically, only one or two per hippocampi exhibits spontaneous SWR activity, fewer than has been reported elsewhere43. Though thicker slices presumably contain a greater degree of recurrent connectivity, cutting slightly thinner slices (400 μm) may yield a greater number per mouse of transversely-oriented slices with SWR activity. In addition, the likelihood that multiple slices reliably exhibit spontaneous SWR activity may be higher in experiments that utilize true horizontal or downward angled slices of the ventral hippocampus. The current protocol incorporates the use of upward angled horizontal slices of the intermediate hippocampus, which may be less likely to exhibit spontaneous network activity in comparison to slices from the ventral hippocampus25,26,31. Finally, this protocol used slices from adolescent and adult mice. While transcardial perfusions can improve the quality of slices from older animals, the likelihood of observing spontaneous network activities may be improved by the use of slices from younger animals12,41,44.
In summary, this protocol presents a mouse brain slicing approach that yields angled horizontal hippocampal-entorhinal cortex slices from the intermediate or ventral hippocampal formation that can exhibit complex spontaneous network activity in the form of sharp wave-ripple complexes.
Declarações
The authors have nothing to disclose.
Acknowledgements
The author would like to thank Steve Siegelbaum for support. Funding is provided by 5R01NS106983-02 as well as 1 F31 NS113466-01.
Materials
| 3D printer | Lulzbot | LulzBot TAZ 6 | |
| Acute brain slice incubation holder | NIH 3D Print Exchange | 3DPX-001623 | Designed by ChiaMing Lee, available at https://3dprint.nih.gov/discover/3dpx-001623 |
| Adenosine 5′-triphosphate magnesium salt | Sigma Aldrich | A9187-500MG | |
| Ag-Cl ground pellets | Warner | 64-1309, (E205) | |
| agar | Becton, Dickinson | 214530-500g | |
| ascorbic acid | Alfa Aesar | 36237 | |
| beaker (250 mL) | Kimax | 14000-250 | |
| beaker (400 mL) | Kimax | 14000-400 | |
| biocytin | Sigma Aldrich | B4261 | |
| blender | Oster | BRLY07-B00-NP0 | |
| Bonn scissors, small | becton, Dickinson | 14184-09 | |
| borosilicate glass capillaries with filament (O.D. 1.5 mm, I.D. 0.86 mm, length 10 cm) | Sutter Instruments | BF150-86-10HP | Fire polished capillaries are preferable. |
| calcium chloride solution (1 M) | G-Biosciences | R040 | |
| camera | Olympus | OLY-150 | |
| compressed carbogen gas (95% oxygen / 5% carbon dioxide) | Airgas | X02OX95C2003102 | |
| compressed oxygen | Airgas | OX 200 | |
| constant voltage isolated stimulator | Digitimer Ltd. | DS2A-Mk.II | |
| coverslips (22×50 mm) | VWR | 16004-314 | |
| cyanoacrylate adhesive | Krazy Glue | KG925 | Ideally use the brush-on form for precision |
| data acquisition software | Axograph | N/A | Any equivalent software (e.g. pClamp) would work. |
| Dell Precision T1500 Tower Workstation Desktop | Dell | N/A | Catalog number will depend on specific computer – any computer will work as long as it can run electrophysiology acquisition software. |
| Digidata 1440A | Molecular Devices | 1-2950-0367 | |
| digital timer | VWR | 62344-641 | 4-channel Traceable timer |
| disposable absorbant pads | VWR | 56616-018 | |
| dissector scissors | Fine Science Tools | 14082-09 | |
| double-edge razor blades | Personna | BP9020 | |
| dual automatic temperature controller | Warner Instrument Corporation | TC-344B | |
| dual-surface or laminar-flow optimized recording chamber | N/A | N/A | The chamber presented in this protocol is custom made. A commercial equivalent would be the RC-27L from Warner Instruments. |
| equipment rack | Automate Scientific | FR-EQ70" | A rack is not strictly necessary but useful for organizing electrophysiology |
| Ethylene glycol-bis(2-aminoethyiether)- N,N,N',N'-teetraacetic acid (EGTA) | Sigma Aldrich | 324626-25GM | |
| filter paper | Whatman | 1004 070 | |
| fine scale | Mettler Toledo | XS204DR | |
| Flaming/Brown micropipette puller | Sutter Instruments | P-97 | |
| glass petri dish (100 x 15 mm) | Corning | 3160-101 | |
| glucose | Fisher Scientific | D16-1 | |
| Guanosine 5′-triphosphate sodium salt hydrate | Sigma Aldrich | G8877-250MG | |
| ice buckets | Sigma Aldrich | BAM168072002-1EA | |
| isoflurane vaporizer | General Anesthetic Services | Tec 3 | |
| lab tape | Fisher Scientific | 15-901-10R | |
| lens paper | Fisher Scientific | 11-996 | |
| light source | Olympus | TH4-100 | |
| magnesium chloride solution (1 M) | Quality Biological | 351-033-721EA | |
| magnetic stir bars | Fisher Scientific | 14-513-56 | Catalog number will be dependent on the size of the stir bar. |
| micromanipulator | Luigs & Neumann | SM-5 | |
| micromanipulator (manual) | Scientifica | LBM-2000-00 | |
| microscope | Olympus | BX51WI | |
| microspatula | Fine Science Tools | 10089-11 | |
| monitor | Dell | 2007FPb | |
| MultiClamp 700B Microelectrode Amplifier | Molecular Devices | MULTICLAMP 700B | The MultiClamp 700B should include headstages, pipette holders, and a model cell. |
| N-(2-Hydroxyethyl)piperazine-N′-(2-ethanesulfonic acid), (HEPES) | Sigma Aldrich | H3375-25G | |
| needle (20 gauge, 1.5 in length) | Becton, Dickinson | 305176 | |
| nylon filament | YLI Wonder Invisible Thread | 212-15-004 | size 0.004. This cat. # is from Amazon.com |
| nylon mesh | Warner Instruments Corporation | 64-0198 | |
| perstaltic pump | Harvard Apparatus | 70-2027 | |
| Phosphocreatine di(tris) salt | Sigma Aldrich | P1937-1G | |
| pipette holders | Molecular Devices | 1-HL-U | |
| platinum wire | World Precision | PT0203 | |
| polylactic acid (PLA) filament | Ultimaker | RAL 9010 | |
| potassium chloride | Sigma Aldrich | P3911-500G | |
| potassium gluconate | Sigma Aldrich | 1550001-200MG | |
| potassium hydroxide | Sigma Aldrich | 60377-1KG | |
| razor blades | VWR | 55411-050 | |
| roller clamp | World Precision Instruments | 14041 | |
| scale | Mettler Toledo | PM2000 | |
| scalpel handle | Fine Science Tools | 10004-13 | |
| slice harp | Warner | SHD-26GH/2 | |
| sodium bicarbonate | Fisher Chemical | S233-500 | |
| sodium chloride | Sigma Aldrich | S9888-1KG | |
| sodium phosphate monobasic anhydrous | Fisher Chemical | S369-500 | |
| sodium pyruvate | Fisher Chemical | BP356-100 | |
| spatula | VWR | 82027-520 | |
| spatula/spoon, large | VWR | 470149-442 | |
| sterile scalpel blades | Feather | 72044-10 | |
| stirrer / hot plate | Corning | 6795-220 | |
| stopcock valves, 1-way | World Precision Instruments | 14054 | |
| stopcock valves, 3-way | World Precision Instruments | 14036 | |
| sucrose | Acros Organics | AC177142500 | |
| support for swivel clamps | Fisher Scientific | 14-679Q | |
| surgical scissors, sharp/blunt | Fine Science Tools | 14001-12 | |
| syringe (1 mL) | Becton, Dickinson | 309659 | |
| syringe (60 mL with Luer-Lok tip) | Becton, Dickinson | 309653 | |
| three-pronged clamp | Fisher Scientific | 05-769-8Q | |
| tissue forceps, large | Fine Science Tools | 11021-15 | |
| tissue forceps, small | Fine Science Tools | 11023-10 | |
| transfer pipettes | Fisher Scientific | 13-711-7M | |
| tubing | Tygon | E-3603 | ID 1/16 inch, OD 3/16 inch |
| tubing | Tygon | R-3603 | ID 1/8 inch, OD 1/4 inch |
| vacuum grease | Dow Corning | 14-635-5D | |
| vibrating blade microtome | Leica | VT 1200S | |
| vibration-dampening table with faraday cage | Micro-G / TMC-ametek | 2536-516-4-30PE | |
| volumetric flask (1 L) | Kimax | KIM-28014-1000 | |
| volumetric flask (2 L) | PYREX | 65640-2000 | |
| warm water bath | VWR | 1209 |
Referências
- Buzsáki, G., Lai-Wo, S., Vanderwolf, C. H. Cellular bases of hippocampal EEG in the behaving rat. Brain Research Reviews. 6, 139-171 (1983).
- Buzsáki, G. Hippocampal sharp waves: Their origin and significance. Brain Research. 398, 242-253 (1986).
- Buzsáki, G., Horváth, Z., Urioste, R., Hetke, J., Wise, K. High-frequency network oscillation in the hippocampus. Science. 256, 1025-1027 (1992).
- Buzsáki, G., Anastassiou, C. A., Koch, C. The origin of extracellular fields and currents — EEG, ECoG, LFP and spikes. Nature Reviews Neuroscience. 13, 407-420 (2012).
- Buzsáki, G. Hippocampal sharp wave-ripple: A cognitive biomarker for episodic memory and planning. Hippocampus. 25, 1073 (2015).
- Maier, N., et al. Reduction of high-frequency network oscillations (ripples) and pathological network discharges in hippocampal slices from connexin 36-deficient mice. Journal of Physiology. 541, 521-528 (2002).
- Maier, N., Nimmrich, V., Draguhn, A. Cellular and network mechanisms underlying spontaneous sharp wave-ripple complexes in mouse hippocampal slices. Journal of Physiology. 550, 873-887 (2003).
- ul Haq, R., et al. Adrenergic modulation of sharp wave-ripple activity in rat hippocampal slices. Hippocampus. 22, 516-533 (2012).
- ul Haq, R., et al. Serotonin dependent masking of hippocampal sharp wave ripples. Neuropharmacology. 101, 188-203 (2016).
- Maier, P., Kaiser, M. E., Grinevich, V., Draguhn, A., Both, M. Differential effects of oxytocin on mouse hippocampal oscillations in vitro. European Journal of Neuroscience. 44, 2885-2898 (2016).
- Mizunuma, M., et al. Unbalanced excitability underlies offline reactivation of behaviorally activated neurons. Nature Neuroscience. 17, 503-505 (2014).
- Hájos, N., et al. Spike timing of distinct types of GABAergic interneuron during hippocampal gamma oscillations in vitro. Journal of Neuroscience. 24, 9127-9137 (2004).
- Geschwill, P., et al. Synchronicity of excitatory inputs drives hippocampal networks to distinct oscillatory patterns. Hippocampus. , (2020).
- Rutecki, P. A., Grossmann, R. G., Armstrong, D., Irish-Loewen, S. Electrophysiological connections between the hippocampus and entorhinal cortex in patients with complex partial seizures. Journal of Neurosurgery. 70, 667-675 (1989).
- Lothman, E. W., Bertram, E. H., Stringer, J. L. Functional anatomy of hippocampal seizures. Progress in Neurobiology. 37, 1-82 (1991).
- Carter, D. S., Deshpande, L. S., Rafiq, A., Sombati, S., Delorenzo, R. J. Characterization of spontaneous recurrent epileptiform discharges in hippocampal – cortical slices prepared from chronic epileptic animals. Seizure: European Journal of Epilepsy. 20, 218-224 (2011).
- Karlócai, M. R., et al. Physiological sharp wave-ripples and interictal events in vitro: What’s the difference. Brain. 137, 463-485 (2014).
- Leroy, F., et al. Input-timing-dependent plasticity in the hippocampal CA2 region and its potential role in social memory. Neuron. 95, 1089-1102 (2017).
- Sun, Q., et al. Proximodistal heterogeneity of hippocampal CA3 pyramidal neuron intrinsic properties, connectivity, and reactivation during memory recall. Neuron. 95, 656-672 (2017).
- Masurkar, A. V., et al. Medial and lateral entorhinal cortex differentially excite deep versus superficial CA1 pyramidal neurons. Cell Reports. 18, 1-13 (2017).
- Papatheodoropoulos, C., Kostopoulos, G. Spontaneous, low frequency (∼2-3 Hz) field activity generated in rat ventral hippocampal slices perfused with normal medium. Brain Research Bulletin. 57, 187-193 (2002).
- Papatheodoropoulos, C., Kostopoulos, G. Spontaneous GABAA-dependent synchronous periodic activity in adult rat ventral hippocampal slices. Neuroscience Letters. 319, 17-20 (2002).
- Kubota, D., Colgin, L. L., Casale, M., Brucher, F. A., Lynch, G. Endogenous waves in hippocampal slices. Journal of Neurophysiology. 89, 81-89 (2003).
- Behrens, C. J., Van Den Boom, L. P., De Hoz, L., Friedman, A., Heinemann, U. Induction of sharp wave – complexes in vitro and reorganization of hippocampal networks. Nature Neuroscience. 8, 1560-1567 (2005).
- Kouvaros, S., Papatheodoropoulos, C. Prominent differences in sharp waves, ripples and complex spike bursts between the dorsal and the ventral rat hippocampus. Neurociência. 352, 131-143 (2017).
- Strange, B. A., Witter, M. P., Lein, E. S., Moser, E. I. Functional organization of the hippocampal longitudinal axis. Nature Reviews Neuroscience. 15, 655-669 (2014).
- Patel, J., Fujisawa, S., Berényi, A., Royer, S., Buzsáki, G. Traveling Theta Waves along the Entire Septotemporal Axis of the Hippocampus. Neuron. 75, 410-417 (2012).
- Patel, J., Schomburg, E. W., Berényi, A., Fujisawa, S., Buzsáki, G. Local generation and propagation of ripples along the septotemporal axis of the hippocampus. Journal of Neuroscience. 33, 17029-17041 (2013).
- Fricke, R., Cowan, W. M. An autoradiographic study of the commissural and ipsilateral hippocampo-dentate projections in the adult rat. Journal of Comparative Neurology. 181, 253-269 (1978).
- Ishizuka, N. O. R., Weber, J., Amaral, D. G. Organization of intrahippocampal projections originating from CA3 pyramidal cells in the rat. The Journal of Comparative Neurology. 623, 580-623 (1990).
- Papatheodoropoulos, C. Electrophysiological evidence for long-axis intrinsic diversification of the hippocampus. Frontiers in Bioscience – Landmark. 23, 109-145 (2018).
- Gilbert, M., Racine, R. J., Smith, G. K. Epileptiform burst responses in ventral vs dorsal hippocampal slices. Brain Research. 361, 389-391 (1985).
- Papatheodoropoulos, C., Moschovos, C., Kostopoulos, G. Greater contribution of N-methyl-D-aspartic acid receptors in ventral compared to dorsal hippocampal slices in the expression and long-term maintenance of epileptiform activity. Neurociência. 135, 765-779 (2005).
- Jones, R. S. G., Heinemann, U. Synaptic and intrinsic responses of medial entorhinal cortical cells in normal and magnesium-free medium in vitro. Journal of Neurophysiology. 59, (1988).
- Rafiq, A., Delorenzo, R. J., Coulter, D. A. Generation and propagation of epileptiform discharges in a combined entorhinal cortex / hippocampal slice. Journal of Neurophysiology. 70, 1962-1974 (1993).
- Stoop, R., Pralong, E. Functional connections and epileptic spread between hippocampus, entorhinal cortex and amygdala in a modified horizontal slice preparation of the rat brain. European Journal of Neuroscience. 12, 3651-3663 (2000).
- Roth, F. C., Beyer, K. M., Both, M., Draguhn, A., Egorov, A. V. Downstream effects of hippocampal sharp wave ripple oscillations on medial entorhinal cortex layer V neurons in vitro. Hippocampus. 26, 1493-1508 (2016).
- Bertsche, A., Bruehl, C., Pietz, J., Draguhn, A. Region- and pattern-specific effects of glutamate uptake blockers on epileptiform activity in rat brain slices. Epilepsy Research. 88, 118-126 (2010).
- Wu, C., Shen, H., Luk, W. P., Zhang, L. A fundamental oscillatory state of isolated rodent hippocampus. Journal of Physiology. 540, 509-527 (2002).
- Colgin, L. L., Jia, Y., Sabatier, J. M., Lynch, G. Blockade of NMDA receptors enhances spontaneous sharp waves in rat hippocampal slices. Neuroscience Letters. 385, 46-51 (2005).
- Ellender, T. J., Nissen, W., Colgin, L. L., Mann, E. O., Paulsen, O. Priming of hippocampal population bursts by individual perisomatic-targeting interneurons. The Journal of Neuroscience. 30, 5979-5991 (2010).
- Xiong, G., Metheny, H., Johnson, B. N., Cohen, A. S. A. Comparison of different slicing planes in preservation of major hippocampal pathway fibers in the mouse. Frontiers in Neuroanatomy. 11, 1-17 (2017).
- Maier, N., Morris, G., Johenning, F. W., Schmitz, D. An approach for reliably investigating hippocampal sharp wave-ripples in vitro. PLoS One. 4, 6925 (2009).
- Schlingloff, D., Kali, S., Freund, T. F., Hajos, N., Gulyas, A. I. Mechanisms of sharp wave initiation and ripple generation. Journal of Neuroscience. 34, 11385-11398 (2014).
- McCloskey, D. P., Scharfman, H. E. Progressive, potassium-sensitive epileptiform activity in hippocampal area CA3 of pilocarpine-treated rats with recurrent seizures. Epilepsy Research. 97, 92-102 (2011).
- McMahon, L. L., Williams, J. H., Kauer, J. A. Functionally distinct groups of interneurons identified during rhythmic carbachol oscillations in hippocampus in vitro. Journal of Neuroscience. 18, 5640-5651 (1998).
- Pöschel, B., Heinemann, U., Draguhn, A. High frequency oscillations in the dentate gyrus of rat hippocampal slices induced by tetanic stimulation. Brain Research. 959, 320-327 (2003).
- Hájos, N., et al. Maintaining network activity in submerged hippocampal slices: importance of oxygen supply. European Journal of Neuroscience. 29, 319-327 (2009).
- Hájos, N., Mody, I. Establishing a physiological environment for visualized in vitro brain slice recordings by increasing oxygen supply and modifying aCSF content. Journal of Neuroscience Methods. 183, 107-113 (2009).
- Dengler, C. G., Yue, C., Takano, H., Coulter, D. A. Massively augmented hippocampal dentate granule cell activation accompanies epilepsy development. Nature Publishing Group. , 1-17 (2017).
- Ting, J. T., et al. Preparation of acute brain slices using an optimized N -methyl-D-glucamine protective recovery method. Journal of Visualized Experiments. 132, 1-13 (2018).
- Westerhof, N., Lankhaar, J. W., Westerhof, B. E. The arterial windkessel. Medical and Biological Engineering and Computing. 47, 131-141 (2009).
- Shi, W. X., Bunney, B. S. A small volume chamber for electrical recording from submerged brain slices and a pulse-free medium supply system using a peristalic pump. Journal of Neuroscience Methods. 35, 235-240 (1990).

