The Ex vivo Preparation of Spinal Cord Slice for the Whole-Cell Patch-Clamp Recording in Motor Neurons During Spinal Cord Stimulation
Summary
This protocol describes a method using a patch-clamp to study the electrical responses of motor neurons to spinal cord stimulation (SCS) with high spatiotemporal resolution, which can help researchers improve their skills in separating the spinal cord and maintaining cell viability simultaneously.
Abstract
Spinal cord stimulation (SCS) can effectively restore locomotor function after spinal cord injury (SCI). Because the motor neurons are the final unit to execute sensorimotor behaviors, directly studying the electrical responses of motor neurons with SCS can help us understand the underlying logic of spinal motor modulation. To simultaneously record diverse stimulus characteristics and cellular responses, a patch-clamp is a good method to study the electrophysiological characteristics at a single-cell scale. However, there are still some complex difficulties in achieving this goal, including maintaining cell viability, quickly separating the spinal cord from the bony structure, and using the SCS to successfully induce action potentials. Here, we present a detailed protocol using patch-clamp to study the electrical responses of motor neurons to SCS with high spatiotemporal resolution, which can help researcher improve their skills in separating the spinal cord and maintaining the cell viability at the same time to smoothly study the electrical mechanism of SCS on motor neuron and avoid unnecessary trial and mistake.
Introduction
Spinal cord stimulation (SCS) can effectively restore locomotor function after spinal cord injury (SCI). Andreas Rowald et al. reported that SCS enables lower limb locomotor and trunk function within a single day1. Exploring the biological mechanism of SCS for locomotor recovery is a critical and trending research field for developing a more precise SCS strategy. For example, Grégoire Courtine's team demonstrated that excitatory Vsx2 interneuron and Hoxa10 neurons in the spinal cord are the key neurons to response to SCS, and cell-specific neuromodulation is feasible to restore the rat walking ability after SCI2. However, few studies focus on the electrical mechanism of SCS at a single-cell scale. Although it is well-known that the suprathreshold direct current stimulus can elicit the action potentials (APs) in the classic squid experiment3,4,5, how the pulsed alternating electrical stimulation, such as SCS, affects the motor signal generation is still unclear.
Given the complexity of intraspinal neural circuits, appropriate selection for cell population is important for investigating the electrical mechanism of SCS. Although SCS restores motor function by activating the proprioceptive pathway6, the motor neurons are the final unit to execute the motor command, derived from integrating proprioception information afferent input7. Therefore, directly studying the electrical characteristics of motor neurons with SCS can help us understand the underlying logic of spinal motor modulation.
As we know, patch-clamp is the golden-standard method for cellularly electrophysiological recording with extremely high spatiotemporal resolution8. Therefore, this study describes a method using a patch clamp to study the electrical responses of motor neurons to SCS. Compared with the brain patch-clamp9, the spinal cord patch-clamp is more difficult due to the following reasons: (1) The spinal cord is protected by the vertebral canal with tiny volume, which requires very fine micromanipulation and rigorous ice-cold maintenance to obtain better cell viability. (2) Because the spinal cord is too slender to be secured on the cutting tray, it should be immersed in low-melting point agarose and trimmed after solidification.
Hence, this method provides technical details in dissecting the spinal cord and maintaining the cell viability at the same time so as to smoothly study the electrical mechanism of SCS on motor neurons and avoid unnecessary trials and mistakes.
Protocol
The Institutional Animal Care and Use Committee approved all animal experiments and the studies were conducted in accordance with relevant animal welfare regulations.
1. Animals preparation
- Animals
- Housing information: House male Sprague-Dawley rats (Postnatal 10-14 days, P10-P14) in a specific pathogen-free environment.
NOTE: Room conditions were maintained at 20 °C ± 2 °C, humidity: 50%-60%, with a 12-h light/ dark cycle. Animals had free access to food and water. - Label the motor neurons retrogradely: Inject Fluoro-Gold (FG) into the bilateral tibialis anterior and gastrocnemius muscle (2% in sterile saline, 50 µL per muscle) to retrogradely label the motor neurons 2 days before the sacrifice.
- Housing information: House male Sprague-Dawley rats (Postnatal 10-14 days, P10-P14) in a specific pathogen-free environment.
- Solutions
- Prepare cutting solution: Mix 120 mM Choline Chloride, 2.6 mM KCl, 26 mM NaHCO3, 1.25 mM NaH2PO4, 0.5 mM CaCl2, 7 mM MgCl2, 1.3 mM Ascorbic Acid, 15 mM Glucose. Pre-bubble the solution with 95% O2 and 5% CO2 (adjust to pH 7.4 with KOH) for 30 min before the dissection and slicing. Cool the solution with crushed ice.
- Prepare artificial cerebrospinal fluid (ACSF): Mix 126 mM NaCl, 3 mM KCl, 1.2 mM NaH2PO4; 1.3 mM MgCl2, 2.4 mM CaCl2, 26 mM NaHCO3, and 10 mM glucose. Pre-bubble the solution with 95% O2 and 5% CO2 for 30 min before the incubation.
- Prepare intracellular solution: Mix 126 mM K-Gluconate, 2 mM KCl, 2 mM MgCl2, 0.2 mM EGTA, 10 mM HEPES, 4 mM Na2ATP, 0.4 mM Na2GTP, 10 mM K-Phosphocreatine, and 0.5% Neurobiotin (pH 7.25 and 305 mOsm/Kg). Cool the solution with crushed ice.
- Prepare low-melting agarose gel: Dissolve 4 g of agarose in 100 mL of cutting solution, and use a magnetic stirring rotor to fully dissolve it. At 30 min before embedding, heat the low-melting-point agarose in the microwave oven with high power for 1 min, and then transfer it into a 39 °C water bath to maintain the liquid state.
- Instrument preparation
- Place crushed ice on the perfusion tray (Supplementary Figure 1A) at 10 min prior to perfusion. Place the anatomical tray (Supplementary Figure 1B) and cutting tray (Supplementary Figure 1C) with a water band at -80 °C overnight in advance.
- Place the incubation chamber with nylon mesh in the oven at 45 °C overnight in advance.
- Use low-melting point agarose to prefabricate a 35° slope and a 2 mm thick platform (Supplementary Figure 1D). After gel solidification, place them in the center of a 35-mm Petri dish to support the spinal cord in the next coming procedures.
- Intracardial perfusion
- Anesthetize the rats with 2.5% tribromoethanol (160 µL/10 g) via intraperitoneal injection. Ensure the rats are fully anesthetized by verifying the lack of response to external stimuli, such as a gentle pinch of the toe.
- When the proper anesthetization is confirmed, place the rats supine and immobilize them in the Petri dish filled with silica gel.
- Cut a 5-mm longitudinal skin incision caudally to the xiphoid process, then fully expand the subcutaneous space. Cut a 2-cm longitudinal skin incision along the ventral midline to fully expose the outer chest wall, starting with the above-mentioned incision and ending with the top of the chest.
- Use toothed tweezers to lift the xiphoid (Supplementary Figure 2A), and then use fine scissors to cut the diaphragm. Cut the sternum along both sides of the xiphoid process to open the chest and expose the heart (Supplementary Figure 2B).
NOTE: Be careful to preserve the internal thoracic vessels on both sides; otherwise, it may cause massive bleeding. - Use toothless tweezers to lift the left ventricle. Insert a 22 G needle into the left ventricular apex along the longitudinal axis of the left ventricle (Supplementary Figure 2C). Meanwhile, observe the rhythmic blood pulsation in the perfusion tube, or the needle may puncture into the right ventricle, which may lead to a poor perfusion effect.
NOTE: Toothed tweezer should not be used; otherwise it may cause extra blood leakage from the tweezer holding site. - Use fine scissors to cut the right atrium (Supplementary Figure 2C), then manually inject 100 mL of ice-cold perfusing fluid at a rate of about 2 mL/s within 1 min.
NOTE: When rats' liver and paws turn pale, and no blood flows out from the right atrium, good perfusion can be achieved.
- Spinal cord dissection (Figure 1)
- Place the rat in the prone position, and cut the spine at the anterior superior iliac spine (about L4 vertebral level) and the curvature shifting point of the thoracic column (about T6 vertebral level), respectively (Figure 1A). Then, immediately place the isolated spine in the oxygenated ice-cold perfusing solution to wash off the residual blood and fat tissue; this procedure is beneficial for keeping the operative field clean in the subsequent procedures.
NOTE: The paraspinal muscles should be reserved, which is conducive for the subsequent fixation of the spine by using an insect pin. - Immediately transfer the isolated spine to the anatomical tray (Figure 1B) with the dorsal side up and the rostral end close to the operator. Fill the anatomical tray with 50 mL of continuously oxygenated ice-cold cutting solution (Figure 1B).
- Use four insect pins to fix the spine by penetrating the paraspinal muscles (Figure 1B).
- Under the dissection microscope, cut the vertebral pedicles of both sides from the rostral end with the micro-scissor, which can be termed "laminectomy" (Figure 1C). Pay attention not to damage the spinal cord. Meanwhile, use the micro-toothed tweezers to lift the cut vertebral body.
- After the laminectomy, do not separate the spinal cord from the spinal canal immediately. Instead, use a micro-scissor to cut the dura mater along the dorsal midline, which is conducive for nutrient uptake between cells and oxygenated ACSF (Figure 1D).
NOTE: Never tear the dura mater. Only cutting the dura mater by micro-scissor is permitted; otherwise, the nerve root and the spinal parenchyma will be seriously damaged! - Lift the rostral part of the spinal cord, then carefully cut the nerve root with about 1 mm reserved (Figure 1E). After separating the spinal cord from the vertebral canal, use 2 insect pins to fix the spinal cord with the ventral side up (Figure 1F).
- Use a micro-scissor to cut the dura mater along the ventral midline (Figure 1F). Cut off the redundant nerve roots with about 1 mm reserved.
NOTE: The nerve is much more tenacious than the spinal cord. If the reserved nerve root is too long (>1 mm), the vibratome cannot cut off the nerve root, which may lead to a serious tear in the spinal parenchyma. - Use a micro-scissor to separate the lumbar enlargement to a length of 6-7 mm (Figure 1G).
- Place the rat in the prone position, and cut the spine at the anterior superior iliac spine (about L4 vertebral level) and the curvature shifting point of the thoracic column (about T6 vertebral level), respectively (Figure 1A). Then, immediately place the isolated spine in the oxygenated ice-cold perfusing solution to wash off the residual blood and fat tissue; this procedure is beneficial for keeping the operative field clean in the subsequent procedures.
- Embedding in the low-melting agarose
- Place the lumbar enlargement on the 35 °slope (Figure 1H) with the dorsal side up and caudal end down. Use an absorbent filter paper to remove abundant water on the tissue surface (Figure 1H).
- Slowly pour the molten agarose gel into the Petri dish containing the lumbar enlargement (Figure 1I).
NOTE: Do not pour too fast, or bubbles will accumulate in the gel. - Place the above Petri dish in the ice-water mixture to cool the gel as soon as possible, which is conducive to maintaining the activity of cells.
- Trim the gel into a 15 mm x 10 mm x 10 mm cube and mount it on the specimen disc with superglue (Figure 1J).
- Slicing
- Place the specimen disc into the pre-frozen cutting tray, then pour the ice-cold cutting solution (Figure 1K). Continuously bubble with 95% CO2 and 5% O2 into the cutting tray.
- Set the vibratome parameters: thickness: 350 µm; speed: 0.14-0.16 mm/s, amplitude: 1.0 mm, and vibration frequency: 85 Hz.
- Harvest 2-3 suitable slices per animal. Record 1-2 healthy FG+ motor neurons per slice, with a range of 5-6 cells per animal.
- Incubation
- Use cover slide tweezers to clip a slice (Figure 1L) and place it into the incubation chamber filled with continuously oxygenated ACSF. Place the incubation chamber in a water bath at 32 °C for 30 min, and then continue to incubate it at room temperature (RT) for another 30 min prior to recording.
NOTE: The above procedures, from anesthesia to obtaining the first slice, should be completed within 20-30 min to retain the viability of cells as much as possible. The motor neurons in each slice can maintain their viability for approximately 6-7 h.
- Use cover slide tweezers to clip a slice (Figure 1L) and place it into the incubation chamber filled with continuously oxygenated ACSF. Place the incubation chamber in a water bath at 32 °C for 30 min, and then continue to incubate it at room temperature (RT) for another 30 min prior to recording.
2. Patch-clamp recording with SCS (Figure 2)
- Preparations
- Perfuse the recording chamber with continuously bubbled ACSF at a rate of about 1-2 mL/min. Adjust the flow rate individually via the control panel on the peristaltic pump.
- Place a slice into the recording chamber. Use the U-shaped platinum wire with nylon threads to firmly stabilize the slice in place.
- Use an infrared differential interference contrast microscope (IR-DIC) to observe the slice. Under the 4x objective lens, confirm that the length of the dorsal root is about 1 mm. Find the area where the dorsal root enters the parenchyma, then move the central field of vision to this area.
- Connect the pulse generator with custom-made electrodes (Figure 2A).
- SCS configuration
- Place the anode of SCS near the dorsal midline via the micromanipulation system (Figure 2B).
- Place the cathode of SCS near the dorsal root entry zone (DREZ) via the micromanipulation system (Figure 2B).
- Cell targeting and imaging
- Use IR-DIC with a 10x objective lens roughly find the dorsolateral region of the motor column, where most motor neurons are located. Then, move the central field of vision to this area.
- Switch to a 60x objective lens to find a healthy neuron with a smooth and bright surface and invisible nuclei (Figure 2C,F).
- Slightly turn down the IR intensity and turn on the fluorescence light source. Switch the light filter to the wide band ultraviolet excitation filter (Figure 2D,G), to select an appropriate FG-positive (FG+) motor neuron (Figure 2E,H).
- Use suction electrodes to apply 1x motor threshold stimulation to the dorsal root. If an evoked action potential is detected in the motor neurons (Supplementary Figure 3), it confirms that the activity of the dorsal root is intact. If not, this slice should be discarded.
- Patch-clamp recording
- Fill the micropipette with the intracellular solution and insert it into the electrode holder. Use the micromanipulation system to lower the pipette into the ACSF bath. The pipette resistance ranges from 5-8 MΩ.
- Apply a small amount of positive pressure to the pipette to blow away the dust and cell debris.
- Lower the electrode to approach the cell. When the pipette touches the surface of FG+ neuron, a small indentation of the membrane becomes visible at the level of the tip. Release the positive pressure.
- Then, apply a small amount of negative pressure to the pipette using a syringe. This creates a small amount of suction that pulls the cell membrane into contact with the glass pipette. Always pay attention to the total resistance on the software interface until the resistance value increases to gigaohms (>1 GΩ). Then, the gigaseal is formed.
- Clamp the membrane potential at -70 mV, then press the fast capacitance compensation button on the software interface of the amplifier. Gently apply a transiently negative pressure to rupture the cell membrane, then press the slow capacitance compensation button on the software interface of the amplifier. At this point, a good whole-cell configuration is obtained.
- Switch to current-clamp mode by clicking the IC button on the software interface, and record the resting membrane potential (RMP).
- Apply the SCS for 1-2 s with the amplitude of 1-10 mA, while the pulse width and frequency are fixed at 210 µs and 40 Hz, respectively. Determine the motor threshold by slowly increasing the stimulation amplitude until the first AP is observed.
- Distinguish delayed and immediate firing motor neurons using a 5 s depolarizing current injection around rheobase in the current-clamp mode10,11,12. Immediate firing motor neurons: Low rheobase can induce immediate and repetitive firing with stable firing frequency; Delayed firing motor neurons: High rheobase can induce a delayed onset for repetitive firing with an accelerating firing rate (Figure 3).
- When SCS is turned off, continue to record the membrane potential for capturing the spontaneous APs firing.
- Perform voltage-clamp recordings voltage-clamp recordings for excitatory postsynaptic current (EPSC) when SCS is on and off. The stimulation parameter is 1x motor threshold, 210 µs, 2 Hz.
Representative Results
Thanks to the rigorous low-temperature maintenance during the fine operation (Supplementary Figure 1, Supplementary Figure 2, and Figure 1), the cell viability was good enough to perform subsequent electrophysiological recordings. To simulate the clinical scenario as much as possible, we used micromanipulation to place the SCS cathode and anode near the dorsal midline and DREZ, respectively (Figure 2), which could initiate neural signal in the dorsal horn to propagate to the motor neurons in the dorsolateral region of the motor column. In this study, we used FG to locate the motor neurons with a diameter of 20-50 µm. As shown in Figure 2D,G, we confidently confirmed a healthy FG+ neuron as a motor neuron-the terminal of the spinal circuit. This labeling method paved the way to study how SCS affects the firing pattern. The electrophysiological properties of delayed and immediate firing motor neurons are listed in Supplementary Table 1 and Supplementary Table 2. The methods for calculating the active and passive properties are provided in Supplementary File 1.
When SCS delivered a pulsed alternating electric field to the spinal slice, we first used current-clamp mode to record the response of membrane potential (Figure 4). As we gradually increased the stimulation amplitude with a step of 1/3 motor threshold (Figure 4B,C), the membrane potential also rose with it, but only 1x motor threshold could elicit Aps (Figure 4D). Figure 4D shows that about every 10-20 pulses could elicit an AP, which indicates that a definite AP response regularity to SCS amplitude might exist.
After the SCS was turned off, we continued to record membrane potential. Figure 5 showed that the membrane potential slightly increased to -60 mV, and the neuron fired a series of spontaneous APs. These spontaneous APs last for a short period of time (30-40 s), then the membrane potential returned to -65 mV, indicating that the SCS can temporarily increase the cell excitability.
Then, we used voltage-clamp recordings for EPSC when SCS was on and off (Figure 6). After each SCS pulse, an evoked EPSC could be detected. The latency between the stimulus artifact and EPSC was 2.64 ± 0.38 ms (Supplementary Figure 4). The amplitude of evoked EPSCs was 35.14 ± 12.73 pA (Supplementary Figure 4). The frequency of evoked EPSCs is consistent with the SCS frequency. After subtracting the passive charge balancing, the evoked EPSC can be observed in a viable motor neuron following 1x motor threshold stimulation (Supplementary Figure 5A). The stimulation polarity was reversed after stopping the perfusion for 2 h in the same cell. The stimulation did not induce any EPSC, confirming that the evoked EPSC was not an artifact (Supplementary Figure 5B).
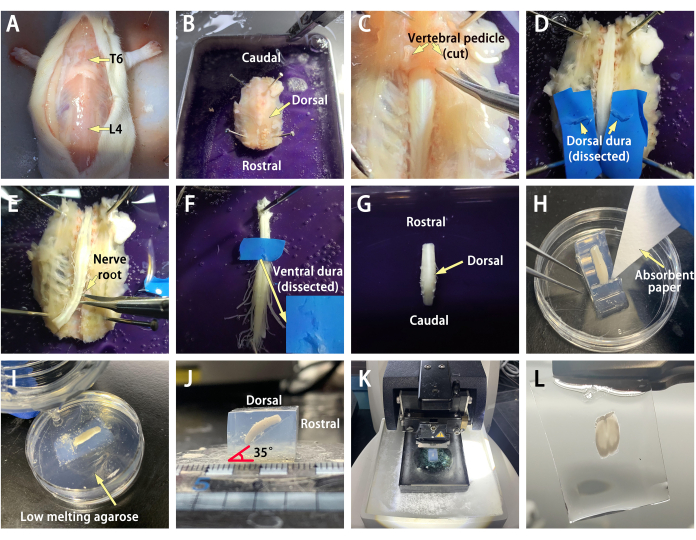
Figure 1: Spinal cord dissection and slicing. (A) Cut the spine at the anterior superior iliac spine (about L4 vertebral level) and the curvature shifting point of the thoracic column (about T6 vertebral level), respectively. (B) Immediately transfer the isolated spine to the anatomical tray with the dorsal side up and the rostral end close to the operator. Fill the anatomical tray with the continuously oxygenated ice-cold cutting solution. (C) Perform laminectomy on both sides from the rostral end. (D) Cut the dorsal dura mater, which is conducive to nutrient uptake between cells and oxygenated artificial cerebrospinal fluid (ACSF). (E) Carefully cut the nerve root. (F) Cut the ventral dura mater.(G)Separate the lumbar enlargement to a length of 6-7 mm. (H) Place the lumbar enlargement on the 35 °slope with the dorsal side up and caudal end down. Use an absorbent filter paper to remove abundant water on the tissue surface. (I) Slowly pour the molten agarose gel into the petri dish. (J) Trim the gel into a cube and mount it on the specimen disc with super glue.(K)Place the specimen disc into the cutting tray, then pour the ice-cold cutting solution.(L)An example of a spinal slice at lumbar enlargement. Please click here to view a larger version of this figure.
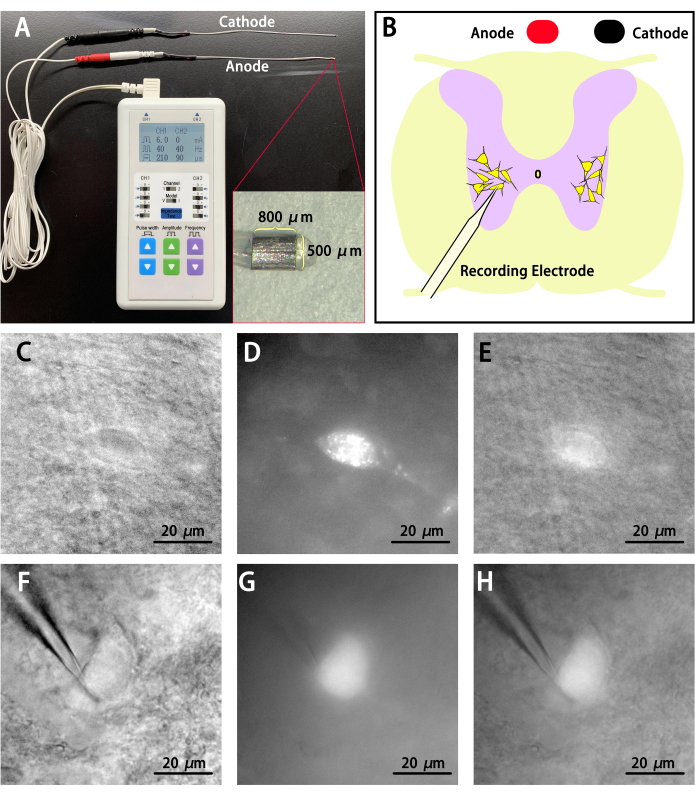
Figure 2: Spinal cord stimulation (SCS) configuration and motor neuron imaging. (A) The pulse generator with custom-made electrodes can separately adjust the amplitude, pulse width, and frequency. Inlet showed that the dimensional specification of an electrode contact is 800 µm x 500 µm x 300 µm. (B) Place the anode and cathode near the dorsal midline and dorsal root entry zone (DREZ) via the micromanipulation system, respectively. Place the recording pipette at the dorsolateral region of the motor column to clamp the Fluoro-Gold positive (FG+) motor neurons. (C) A healthy immediate firing motor neuron with infrared differential interference contrast microscope (IR-DIC) imaging (60x). (D) The same neuron with only fluorescence imaging (60x), shining Fluoro-Gold (FG) particles represent that this neuron is a motor neuron.(E)Merged image of IR-DIC and fluorescence in FG+ motor neuron. (F-H)A healthy delayed firing motor neuron with IR-DIC imaging (60x). Please click here to view a larger version of this figure.
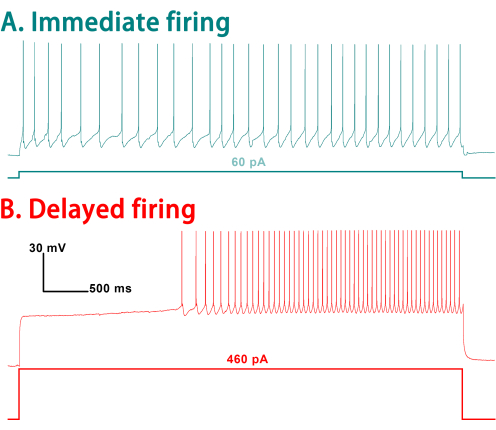
Figure 3: Distinguish delayed and immediate firing motor neurons using a 5 s depolarizing current injection. (A) Immediate firing motor neurons:Low rheobase can induce immediate and repetitive firing with stable firing frequency; (B) Delayed firing motor neurons: High rheobase can induce a delayed onset for repetitive firing with an accelerating firing rate. Please click here to view a larger version of this figure.
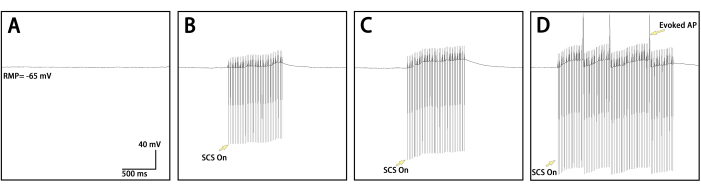
Figure 4: Spinal cord stimulation (SCS) elicited action potentials (APs) firing in motor neurons. (A) When no stimulation was applied, the resting membrane potential (RMP) was -65 mV. (B) 1/3x motor threshold stimulus cannot elicit APs. (C) 2/3x motor threshold stimulus cannot elicit APs.(D) 1x motor threshold stimulus can elicit APs, and every 10-20 pulses can elicit an AP. Please click here to view a larger version of this figure.
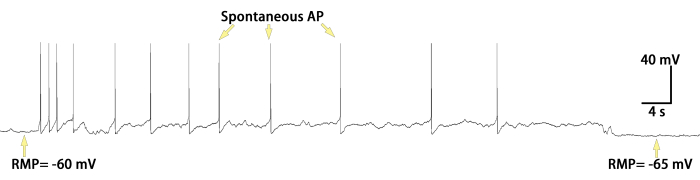
Figure 5: Spontaneous action potentials (APs) firing after spinal cord stimulation (SCS). After the SCS was turned off, the neuron fired a series of spontaneous APs for a short period of time (30-40 s), then the resting membrane potential (RMP) returned to -65 mV. Please click here to view a larger version of this figure.
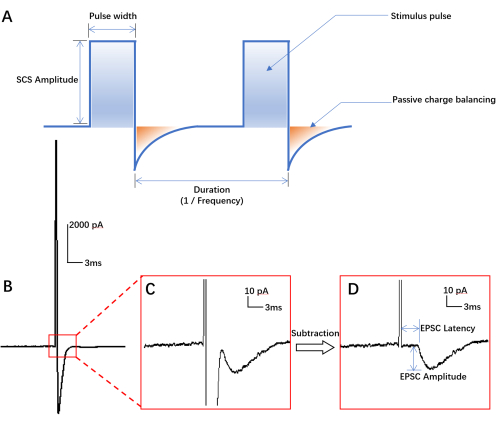
Figure 6: Illustration of spinal cord stimulation (SCS) parameter and evoked excitatory postsynaptic current (EPSC). (A) Illustration of SCS parameter; (B,C) Following a single stimulation pulse (1x motor threshold stimulation), the evoked EPSC can be observed; (D) After subtracting the passive charge balancing, the latency and amplitude of the EPSC can be calculated. Please click here to view a larger version of this figure.
Supplementary Figure 1: Instrument preparation. (A) Perfusion tray: at 10 min before the perfusion, place crushed ice on the 10-cm petri dish filled with silica gel. (B) Anatomical tray: in the night before sacrifice, place the self-made anatomical tray filled with silica gel in the -80 °C refrigerator. (C) Cutting tray: in the night before sacrifice, place the cutting tray with water band in the -80 °C refrigerator. (D) Agarose casting slope: at 30 min before the perfusion, place a 35° agarose slope with base plates in the center of a 35-mm petri dish. Please click here to download this File.
Supplementary Figure 2: Intracardial perfusion. (A) Lift the xiphoid process. (B) Cut the sternum along both sides of the xiphoid process to open the chest and expose the heart. Be careful not to damage the internal thoracic vessels, or massive bleeding will fill the entire operating field and hamper the operator from identifying the ventricle apex or right atrium. (C) Insert a 22 G needle at the left ventricle apex for perfusion and cut the right atrium for fluid exit. Please click here to download this File.
Supplementary Figure 3: Confirming the dorsal root activity. Use suction electrodes to apply 1x motor threshold stimulation to the dorsal root. If an evoked action potential is detected in the motor neurons, we can confirm that the activity of the dorsal root is intact. Please click here to download this File.
Supplementary Figure 4: Latency and amplitude of evoked EPSCs when SCS was on. Please click here to download this File.
Supplementary Figure 5: Demonstration of the validity of the evoked EPSC. (A) Following 1x motor threshold stimulation after subtracting the passive charge balancing, the evoked EPSC can be observed in a viable motor neuron; (B) After stopping the perfusion for 2 h in the same cell, the stimulation polarity was reversed, 1x motor threshold stimulation did not induce any EPSC, which confirmed that the evoked EPSC was not an artifact. Please click here to download this File.
Supplementary File 1: Calculation methods of the active and passive properties. Please click here to download this File.
Supplementary Table 1: Passive properties of motor neurons. Please click here to download this File.
Supplementary Table 2: Active properties of motor neurons Please click here to download this File.
Discussion
The movement information modulated by SCS is finally converged to the motor neurons. Therefore, taking the motor neurons as the research target may simplify the study design and reveal the neuromodulation mechanism of SCS more directly. To simultaneously record diverse stimulus characteristics and cellular responses, a patch-clamp is a good method to study the electrophysiological characteristics at a single-cell scale. However, there are still some difficulties, including how to maintain cell viability, how to quickly separate the spinal cord from the bony structure, and how to use the SCS to induce APs successfully. Therefore, this study aims to help researchers quickly grasp essential operative skills, avoid some possible pitfalls, and focus on the study design rather than methodology as early as possible.
To obtain good cell viability, one should always pay attention to the following details: (1) Keeping the spinal cord at ice-cold temperature is very important because low temperature can inhibit cell death and slow down the metabolic rate, which can protect the neuron from mechanical damage during perfusion, dissection, and slicing13; (2) Delicately removing the dura mater by micro-scissor can enhance the neuronal nutrient uptake from surrounding solutions. Never directly peel off the dura mater; otherwise, the spinal cord will be seriously damaged. In addition, if you forget to clear the dura mater, the subsequent slicing process may be difficult because the blade may not completely cut off the dura mater and then rip out the remaining spinal cord from agarose, which may lead to the failure of slicing. (3) Compared with conventional transverse slice, oblique slices increase the area of gray matter, and you can find more FG+ motor neurons in a single slice9. (4) Because the spinal cord alone cannot be firmly fixed on the specimen disc like the brain, embedding it in agarose gel is effective in solving this problem without decreasing the cell viability. We recommend using low-melting agarose (gel point 26-30 °C) rather than conventional agarose (gel point 38-43 °C), because high temperature may damage the cell viability. (5) We recommend that the distance between two nylon threads of U-shaped platinum wire should be 1 to 1.5 mm because loose threads cannot firmly immobilize the spinal cord, and dense threads may squash the cell.
Compared with the conventional stimulation devices, such as bipolar hook electrodes widely used in basic research, the SCS electrode in this study is derived from our previous clinical work14 and basic research15. SCS deliveries pulsed alternating electrical stimulation, which provides diverse parameter adjusting dimensions. This SCS device also has a charge balance function to avoid tissue electrolysis and does not directly contact the neural tissue; therefore, this SCS has good safety for in vivo applications.
After SCS treatment, the spontaneous APs of motor neurons may be attributed to the following reasons: (1) SCS induces the charge to accumulate in the cell body and axonal colliculus of neurons, leading to the increase of RMP16. This phenomenon indicates that SCS may improve the excitability of neuron, which may be related to the change of conductivity of ion channels after SCS, such as Nav 1.117, Kv 2.118, or Cav 2.319. (2) SCS may activate dorsal GABAergic neurons to facilitate proprioceptive feedback to motor neurons. We suggest that neural transmission may continuously exist between the sensory neurons and motor neurons, leading to spontaneous APs in motor neurons after SCS. Spontaneous APs can maintain an intrinsic state of readiness to execute sensorimotor behaviors20. Therefore, activating or inhibiting spontaneous APs may be beneficial for the treatment of spinal neurological diseases.
As we know, in vivo electrophysiological recording is better for detecting electrophysiological response under the natural distribution of the electric field and the placement of electrodes. Moreover, in vivo motoneuron recordings allow for the identification of motoneuron identity. This can be done through antidromic identification of motor axons coupled with muscle fiber force measurement21. But in vivo spinal cord recordings also have the following drawbacks: (1) Motor neuron lies 2-3 mm away from the dorsal surface of the spinal cord, even using the most advanced two-photon confocal imaging, the observation depth is only 500-800 µm, so it is difficult to optically observe them in vivo using the existing methods. Therefore, if we want to exactly clamp a single motor neuron in vivo, the glass pipette must pass through the dorsal column to reach the invisible motor neuron; the in vivo patch-clamp can only be performed in a “blind” fashion, resulting in significant uncertainty and failure rate. (2) Except for the in vivo patch-clamp, silicon electrode recordings can be the alternative method, such as Utah array or Neuropixels electrode. However, the signals recorded by silicon electrodes are mostly compound action potential rather than single action potential. Although the activity of single neurons has been resolved using spike-sorting algorithms, the accuracy and reliability of sorting algorithms still need to be improved.
Compared to the in vivo recordings, the greatest benefit of in vitro against in vivo is the use of voltage clamp, which allows a unique understanding of the synaptic pathways activated by SCS. In addition, it would also permit the use of live imaging tools. We speculate that SCS induces the release of neurotransmitters such as GABA and glutamate from upper-level neurons onto the motor neurons, resulting in an overall excitatory EPSC response7. Therefore, in our upcoming research, we will incorporate the detection of IPSC, mini EPSC (mEPSC), and evoked EPSC induced by SCS to clarify the patterns of inhibitory and excitatory neurotransmitter release from pre-motor neurons or interneurons. We fully acknowledged that in vitro stimulation also has some limitations: (1) Long-range longitudinal circuitry of the spinal cord is disrupted, resulting in the loss of incoming information from the motor cortex or lower extremity; (2) The distribution of electric fields during in vitro stimulation may differ from that in the in vivo stimulation. In this study, the activation threshold (approximately in milliamperes) for APs was much higher than that of the in vivo experiment (approximately in microamperes)15; this was because the volume capacity of the ACSF solution in the recording chamber was much higher than the cerebrospinal fluid in the natural state, and mathematical theory supports that electric field attenuates faster in high-conductivity materials22. Therefore, most of the current was absorbed by the bath solution, and we speculate that only a small portion of the electric field can diffuse to the nerve roots.
Therefore, considering the advantages and disadvantages of in vivo stimulation and in vitro stimulation, it can be concluded that in vitro patch-clamp is an advantageous method to study the synaptic nature and/or cellular effects of SCS in neonatal rodents.
In clinical practice, the electrode does not directly contract the surface of the spinal cord or the nerve root23. Instead, it relies on the electric field radiation generated by the electrode to indirectly affect the activity of the nerves1. Multiple studies1,23,24 have confirmed that the cathode contact of SCS should be placed as close as possible to the dorsal root or the entry zone (DREZ) to achieve optimal selectivity for stimulating a specific muscle. Increasing the distance between the electrode and the nerve root will weaken the specificity of the stimulation. Therefore, we directly place the cathode near the DREZ rather than directly contacting the nerve root or the spinal cord.
The afferent fibers of the dorsal root first project to the sensory neurons, then to the interneurons and the motor neurons. Besides the transverse projecting circuits, there are also circuits that project towards the rostral and caudal end. For example, motor neurons corresponding to the tibialis anterior muscle can be found at multiple levels25. Therefore, although oblique preparation may sever the transverse projecting circuits, it will still preserve non-transverse projecting fibers, allowing the study of the pre-motor sensory circuitry. In addition to oblique and transverse preparation, longitudinal preparation offers distinct advantages to better preserve the circuits from the dorsal root to the motor neurons and enable the effective retention of spinal cord circuits across multiple segments26, which provides a closer representation of the real physiological conditions.
According to the simulation research6,27,28, SCS mainly activates proprioceptive afferent fibers to restore the lower limb movement, including the Ia, Ib, and II afferent fibers. However, in this study, we cannot confidently confirm which kinds of fiber were specifically activated by SCS. We speculate that a similar pattern may also exist in the in vitro patch clamp. We will address this issue by conducting mathematical modeling and simulation and incorporating it into our ongoing work.
In conclusion, this protocol may help researchers improve their operative skills and grasp the essentials of combining patch-clamp recordings and SCS to investigate the electrical mechanism of SCS at a single-cell scale.
Declarações
The authors have nothing to disclose.
Acknowledgements
This study was funded by the National Natural Science Foundation of China for Young Scholars (52207254 and 82301657) and the China Postdoctoral Science Fund (2022M711833).
Materials
| Adenosine 5’-triphosphate magnesium salt | Sigma | A9187 | |
| Ascorbic Acid | Sigma | A4034 | |
| CaCl2·2H2O | Sigma | C5080 | |
| Choline Chloride | Sigma | C7527 | |
| Cover slide tweezers | VETUS | 36A-SA | Clip a slice |
| D-Glucose | Sigma | G8270 | |
| EGTA | Sigma | E4378 | |
| Fine scissors | RWD Life Science | S12006-10 | Cut the diaphragm |
| Fluorescence Light Source | Olympus | U-HGLGPS | |
| Fluoro-Gold | Fluorochrome | Fluorochrome | Label the motor neuron |
| Guanosine 5′-triphosphate sodium salt hydrate | Sigma | G8877 | |
| HEPES | Sigma | H3375 | |
| infrared CCD camera | Dage-MTI | IR-1000E | |
| KCl | Sigma | P5405 | |
| K-gluconate | Sigma | P1847 | |
| Low melting point agarose | Sigma | A9414 | |
| MgSO4·7H2O | Sigma | M2773 | |
| Micromanipulator | Sutter Instrument | MP-200 | |
| Micropipette puller | Sutter instrument | P1000 | |
| Micro-scissors | Jinzhong | wa1020 | Laminectomy |
| Microscope for anatomy | Olympus | SZX10 | |
| Microscope for ecletrophysiology | Olympus | BX51WI | |
| Micro-toothed tweezers | RWD Life Science | F11008-09 | Lift the cut vertebral body |
| NaCl | Sigma | S5886 | |
| NaH2PO4 | Sigma | S8282 | |
| NaHCO3 | Sigma | V900182 | |
| Na-Phosphocreatine | Sigma | P7936 | |
| Objective lens for ecletrophysiology | Olympus | LUMPLFLN60XW | working distance 2 mm |
| Osmometer | Advanced | FISKE 210 | |
| Patch-clamp amplifier | Axon | Multiclamp 700B | |
| Patch-clamp digitizer | Axon | Digidata 1550B | |
| pH meter | Mettler Toledo | FE28 | |
| Slice Anchor | Multichannel system | SHD-27H | |
| Spinal cord stimulatior | PINS | T901 | |
| Toothed tweezer | RWD Life Science | F13030-10 | Lift the xiphoid |
| Vibratome | Leica | VT1200S | |
| Wide band ultraviolet excitation filter | Olympus | U-MF2 |
Referências
- Rowald, A., et al. Activity-dependent spinal cord neuromodulation rapidly restores trunk and leg motor functions after complete paralysis. Nature Medicine. 28 (2), 260-271 (2022).
- Kathe, C., et al. The neurons that restore walking after paralysis. Nature. 611 (7936), 540-547 (2022).
- Smith, S. J., Buchanan, J., Osses, L. R., Charlton, M. P., Augustine, G. J. The spatial distribution of calcium signals in squid presynaptic terminals. The Journal of Physiology. 472, 573-593 (1993).
- Augustine, G. J. Regulation of transmitter release at the squid giant synapse by presynaptic delayed rectifier potassium current. The Journal of Physiology. 431, 343-364 (1990).
- Llinás, R., McGuinness, T. L., Leonard, C. S., Sugimori, M., Greengard, P. Intraterminal injection of synapsin I or calcium/calmodulin-dependent protein kinase II alters neurotransmitter release at the squid giant synapse. Proceedings of the National Academy of Sciences of the United States of America. 82 (9), 3035-3039 (1985).
- Formento, E., et al. Electrical spinal cord stimulation must preserve proprioception to enable locomotion in humans with spinal cord injury. Nature Neuroscience. 21 (12), 1728-1741 (2018).
- Hari, K., et al. GABA facilitates spike propagation through branch points of sensory axons in the spinal cord. Nature Neuroscience. 25 (10), 1288-1299 (2022).
- Sakmann, B., Neher, E. Patch clamp techniques for studying ionic channels in excitable membranes. Annual Review Of Physiology. 46, 455-472 (1984).
- Leroy, F., Lamotte d’Incamps, B. The preparation of oblique spinal cord slices for ventral root stimulation. Journal of Visualized Experiments:JoVE. (116), e54525 (2016).
- Sharples, S. A., Miles, G. B. Maturation of persistent and hyperpolarization-activated inward currents shapes the differential activation of motoneuron subtypes during postnatal development. Elife. 10, e71385 (2021).
- Bhumbra, G. S., Beato, M. Recurrent excitation between motoneurones propagates across segments and is purely glutamatergic. PLoS Biology. 16 (3), e2003586 (2018).
- Leroy, F., Lamotte d’Incamps, B., Imhoff-Manuel, R. D., Zytnicki, D. Early intrinsic hyperexcitability does not contribute to motoneuron degeneration in amyotrophic lateral sclerosis. Elife. 3, 04046 (2014).
- Tahir, R. A., Pabaney, A. H. Therapeutic hypothermia and ischemic stroke: A literature review. Surgical Neurology International. 7, S381-S386 (2016).
- Lu, Y., et al. Management of intractable pain in patients with implanted spinal cord stimulation devices during the COVID-19 pandemic using a remote and wireless programming system. Frontiers in Neuroscience. 14, 594696 (2020).
- Yao, Q., et al. Wireless epidural electrical stimulation in combination with serotonin agonists improves intraspinal metabolism in spinal cord injury rats. Neuromodulation. 24 (3), 416-426 (2021).
- Arlotti, M., Rahman, A., Minhas, P., Bikson, M. Axon terminal polarization induced by weak uniform dc electric fields: a modeling study. 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society. , 4575-4578 (2012).
- Espino, C. M., et al. Na(V)1.1 is essential for proprioceptive signaling and motor behaviors. Elife. 11, e79917 (2022).
- Romer, S. H., Deardorff, A. S., Fyffe, R. E. W. A molecular rheostat: Kv2.1 currents maintain or suppress repetitive firing in motoneurons. The Journal of Physiology. 597 (14), 3769-3786 (2019).
- Yao, X., et al. Structures of the R-type human Ca(v)2.3 channel reveal conformational crosstalk of the intracellular segments. Nature Communications. 13 (1), 7358 (2022).
- Bandres, M. F., Gomes, J., McPherson, J. G. Spontaneous multimodal neural transmission suggests that adult spinal networks maintain an intrinsic state of readiness to execute sensorimotor behaviors. Journal Of Neuroscience. 41 (38), 7978-7990 (2021).
- Manuel, M., Heckman, C. J. Simultaneous intracellular recording of a lumbar motoneuron and the force produced by its motor unit in the adult mouse in vivo. Journal of Visualized Experiments: JoVE. (70), e4312 (2012).
- Luo, X., Wang, S., Rutkove, S. B., Sanchez, B. Nonhomogeneous volume conduction effects affecting needle electromyography: an analytical and simulation study. Physiological Measurement. 42 (11), (2021).
- Barra, B., et al. Epidural electrical stimulation of the cervical dorsal roots restores voluntary upper limb control in paralyzed monkeys. Nature Neuroscience. 25 (7), 924-934 (2022).
- Powell, M. P., et al. Epidural stimulation of the cervical spinal cord for post-stroke upper-limb paresis. Nature Medicine. 29 (3), 689-699 (2023).
- Wenger, N., et al. Spatiotemporal neuromodulation therapies engaging muscle synergies improve motor control after spinal cord injury. Nature Medicine. 22 (2), 138-145 (2016).
- Özyurt, M. G., Ojeda-Alonso, J., Beato, M., Nascimento, F. In vitro longitudinal lumbar spinal cord preparations to study sensory and recurrent motor microcircuits of juvenile mice. Journal of Neurophysiology. 128 (3), 711-726 (2022).
- Moraud, E. M., et al. Mechanisms underlying the neuromodulation of spinal circuits for correcting gait and balance deficits after spinal cord injury. Neuron. 89 (4), 814-828 (2016).
- Capogrosso, M., et al. A computational model for epidural electrical stimulation of spinal sensorimotor circuits. Journal of Neuroscience. 33 (49), 19326-19340 (2013).

