In Vivo Investigation of Antimicrobial Blue Light Therapy for Multidrug-resistant Acinetobacter baumannii Burn Infections Using Bioluminescence Imaging
Summary
Infections caused by multidrug-resistant (MDR) bacterial strains have emerged as a serious threat to public health, necessitating the development of alternative therapeutics. We present a protocol to evaluate the effectiveness of antimicrobial blue light (aBL) therapy for MDR Acinetobacter baumannii infections in mouse burns by using bioluminescence imaging.
Abstract
Burn infections continue to be an important cause of morbidity and mortality. The increasing emergence of multidrug-resistant (MDR) bacteria has led to the frequent failure of traditional antibiotic treatments. Alternative therapeutics are urgently needed to tackle MDR bacteria.
An innovative non-antibiotic approach, antimicrobial blue light (aBL), has shown promising effectiveness against MDR infections. The mechanism of action of aBL is not yet well understood. It is commonly hypothesized that naturally occurring endogenous photosensitizing chromophores in bacteria (e.g., iron-free porphyrins, flavins, etc.) are excited by aBL, which in turn produces cytotoxic reactive oxygen species (ROS) through a photochemical process.
Unlike another light-based antimicrobial approach, antimicrobial photodynamic therapy (aPDT), aBL therapy does not require the involvement of an exogenous photosensitizer. All it needs to take effect is the irradiation of blue light; therefore, it is simple and inexpensive. The aBL receptors are the endogenous cellular photosensitizers in bacteria, rather than the DNA. Thus, aBL is believed to be much less genotoxic to host cells than ultraviolet-C (UVC) irradiation, which directly causes DNA damage in host cells.
In this paper, we present a protocol to assess the effectiveness of aBL therapy for MDR Acinetobacter baumannii infections in a mouse model of burn injury. By using an engineered bioluminescent strain, we were able to noninvasively monitor the extent of infection in real time in living animals. This technique is also an effective tool for monitoring the spatial distribution of infections in animals.
Introduction
Burn infections, which are frequently reported because of cutaneous thermal injuries, continue to be an important cause of morbidity and mortality1. The management of burn infections has been further compromised by the increasing emergence of multidrug-resistant (MDR) bacterial strains2 due to the massive use of antibiotics. One important MDR Gram-negative bacteria is Acinetobacter baumannii, which is known to be associated with recent battle wounds and is resistant to almost all available antibiotics3. The presence of biofilms at the injured foci has been reported4,5 and is believed to exacerbate the tolerance to antibiotics and host defense6,7, causing persistent infections8,9. Therefore, there is a pressing need for the development of alternative treatments. In the recently announced National Strategy for Combating Antibiotic-Resistant Bacteria, the development of alternative therapeutics to antibiotics has been noted as an action by the government of the United States10.
Light-based antimicrobial approaches, as indicated by the name, require light irradiation with or without other agents. These approaches include antimicrobial photodynamic therapy (aPDT), ultraviolet-C (UVC) irradiation, and antimicrobial blue light (aBL). In previous studies, they have shown promising effectiveness in killing MDR bacterial strains11,12,13. Among the three light-based approaches, aBL has attracted increasing attention in recent years due to its intrinsic antibacterial properties without the use of photosensitizers14. In comparison to aPDT, aBL only involves the use of light, while aPDT requires a combination of light and a photosensitizer. Therefore, aBL is simple and inexpensive14. In comparison to UVC, aBL is believed to be much less cytotoxic and genotoxic to host cells15.
The goal of this protocol is to investigate the effectiveness of aBL for the treatment of burn infections caused by MDR A. baumannii in a mouse model. We use bioluminescent pathogenic bacteria to develop new mouse models of burn infections that allow the non-invasive monitoring of the bacterial burden in real time. Compared to the traditional method of body fluid/tissue sampling and subsequent plating and colony counting16, this technique provides accurate results. The process of tissue sampling could introduce another source of experimental error. Since the bacterial luminescence intensity is linearly proportional to the corresponding bacterial CFU17, we can directly measure the survival of bacteria after a certain dose of light irradiation. By monitoring the bacterial burden in living animals receiving the light treatment in real time, the kinetics of bacterial killing can be characterized using a significantly reduced number of mice.
Protocol
1. Preparation of Bacterial Culture
- Add 7.5 mL of Brain Heart Infusion (BHI) medium to a 50 mL centrifuge tube. Seed A. baumannii cells in the BHI medium and then incubate the A. baumannii culture in an orbital incubator (37 °C) for 18 h.
- Centrifuge the culture of cells at 3,500 × g for 5 min, remove the supernatant, and wash the pellets in phosphate-buffered saline (PBS).
- Re-suspend the bacteria pellets in fresh PBS and thoroughly pipette the suspension.
- Collect 100 µL of the bacterial suspension and make a 1:10 dilution using fresh PBS.
- Transfer the dilution to a 1.5 mL semi-micro cuvette and measure the optical density (OD) at a wavelength of 600 nm (OD600-nm).
- Calculate the OD600-nm of the original (undiluted) suspension in PBS according to the measured OD600 nm value of the dilution and the dilution factor (10).
- Adjust the original suspension in PBS to OD600-nm = 0.6 (corresponding to a cell density of 108 CFU/mL).
2. Mouse Model of Burn Infection Caused by Bioluminescent A. baumannii
- Use adult female BALB/c mice aged 7-8 weeks and weighing 17-19 g. Allow the mice to acclimatize to laboratory conditions for at least 3 days before the start of experiment. Maintain the mice in a 12 h light/dark cycle under a room temperature of 21 ℃ and give them food and water ad libitum.
- Anesthetize the mice with an intraperitoneal injection of a ketamine-xylazine cocktail (100 mg/kg – 20 mg/kg). Lightly touch the palpebra of each mouse with a cotton swab; an absence of the palpebral reflex suggests an appropriate anesthetic depth. Cover the mouse eyes with vet ointment to prevent the eyes from dryness during anesthesia.
- Shave the mice on the back to expose as much skin as possible by using a 50-blade hair clipper.
- Place the lid of a 35 mm Petri dish underneath the abdomens of the mice to keep their backs in a relatively horizontal position.
- Boil water in a 250 mL beaker (80% full) using a 10" x 10", 220 VAC hotplate. Immerse a brass block (1 cm x 1 cm cross section) into the beaker until thermal equilibration with the water is reached. Thermal equilibration usually takes <5 min and is indicated by the re-boiling of the water in the beaker.
- Prior to creating the burn injury, administer pre-emptive analgesics (a subcutaneous injection of 0.1mg/kg buprenorphine) for pain relief.
- Ten minutes after the pre-emptive analgesics, gently press the heated brass block to the shaved area on the back of the mice for 7 s to induce burn wounds.
NOTE: To avoid thermal injury to the working personnel, wear thermal-resistant gloves when performing the burning procedure. - Administer 0.5 mL of sterile saline through subcutaneous injection to prevent dehydration.
- Five minutes following the induction of the thermal injury, inoculate 50 µL of bacterial suspension containing 5 x 106 CFU in PBS onto the mouse burns using a pipette. By moving a sterile cotton swab in a zigzag motion on the skin, smear the aliquots on the burns to distribute the bacterial cells in the burned area as evenly as possible.
- Immediately after bacterial inoculation, perform bioluminescence imaging for the infected burns, as described in Section 4.
- Place the mice on a water-heated surgical bed (37 °C, recovery area) until the mice have completely recovered from anesthesia. House the mice with a maximum number of 5 per cage in a Biosafety Level-2 animal room.
- Administer analgesics (subcutaneous injection of 0.1 mg/kg buprenorphine) twice daily for the first three days after the burn injury.
3. Antimicrobial Blue Light Therapy for A. baumannii Infection in Mice
- Start aBL therapy at 24 h after bacterial inoculation.
- Use a light-emitting diode (LED) with a peak emission at 415 nm for aBL irradiation. Mount the LED on a heat sink to prevent thermal effects on the irradiated area in mice18. Fix the LED to an optical support rod with clip connectors to allow the LED to move up and down.
- Turn on the power/energy meter and press the wavelength button to select 415 nm. Reset the power/energy meter to subtract the background (ambient light).
- Place the power/energy meter right under the LED. Wear blue-light-protective goggles. Turn on the LED light and adjust the distance between the LED aperture (a lens that converges the light from the LED) and the light sensor (2 cm in diameter) of the power/energy meter so that the light spot covers the whole area of the light sensor.
- Carefully tune the LED driver and record the reading of the power/energy meter. Calculate the irradiance according to the reading: Irradiance = Reading (W)/Area (cm2). Adjust the irradiance of the LED to 100 mW/cm2 by tuning the LED driver.
- Turn off the LED. Measure the distance between the LED aperture and the light sensor of the power/energy meter.
- Anesthetize the mice with an intraperitoneal injection of a ketamine-xylazine cocktail (100 mg/kg – 20 mg/kg). An absence of the palpebral reflex suggests an appropriate anesthetic depth.
- Randomly divide the mice into an aBL-treated group (n = 10) and an untreated control group (n = 10).
- For the aBL-treated group, cover the eyes of mice with aluminum foil to avoid overexposure to light. Place the mouse burns directly under the LED, with the lid of a 35-mm petri dish underneath the mouse abdomen to keep their backs in a horizontal position.
- Replace the power/energy meter mentioned in step 3.5 with a mouse on a square petri dish. Adjust the height of the mouse back to a position where the distance between the LED aperture and the surface of the mouse burn is equal to that between the LED aperture and the level of the light sensor of the power/energy meter (as discussed in step 3.5).
- Irradiate the infected burns at an irradiance of 100 mW/cm2. Deliver aBL in doses of 72 J/cm2 until a total dose of 360 J/cm2 is reached (e.g., 0, 72, 144, 216, 288 and 360 J/cm2). After each light dose, perform bioluminescence imaging for the mice, as discussed in Section 4.
- For the untreated control group, perform bioluminescence imaging of the mouse burns, as discussed in Section 4, using the same time intervals as used for the aBL-treated group.
- Before the recovery of the mice, place the mice on the water-heated surgical bed to prevent heat loss and hypothermia. Observe the activity and the palpebral reflex of the mice until recovery. After the recovery of the mice, house them 2-3 per cage.
- After aBL therapy, perform bioluminescence imaging, as discussed in Section 4, daily for the first 3 days and then on alternate days to monitor the temporal bio-burden of infections in mice.
4. Bioluminescence Imaging of Infections in Mice
- Image the mice using a low-light imaging system that includes an intensified charge-coupled device camera, a camera controller, a specimen chamber, and an image processor19.
- Anesthetize the mice with an intraperitoneal injection of a ketamine-xylazine cocktail (100 mg/kg – 20 mg/kg). Lightly touch the palpebral of the mice with a cotton swab; an absence of the palpebral reflex suggests an appropriate anesthetic depth.
- Start the live imaging software. In the control panel that appears, click Initialize. Wait until the color of the Temperature box turns green, indicating that the temperature of the stage in the specimen chamber has reached 37 °C.
- Place the mice on the stage (37 °C) in the specimen chamber of the imaging system, with the infected burns directly under the camera.
NOTE: The bioluminescence of the bacteria could decrease when the burns become dry. Therefore, it is recommended to moisturize the mouse burns with PBS before imaging. - In the control panel, put a check mark next to "Luminescence." Select "Auto exposure" so that the exposure time for imaging will be optimized by the live imaging software based on the bioluminescence intensity.
- Select "C" from the "Field of View" drop-down list. Select the "Scan mid range" option to let the software determine the focal distance. Put a check mark next to Overlay.
- Click "Acquire" to capture the image. In the "Edit Image Label" box, click "OK;" an "Image Window" and "Toll Palette" will appear.
- Set Auto ROI parameters for auto-selection.
- Quantify the bioluminescence intensity as relative luminescence units (RLUs) and display the bioluminescence in a false-color scale ranging from pink (most intense) to blue (least intense)19,20.
- Calculate the survival fraction of the bacteria in mouse burns at varying time points based upon bioluminescence intensity analysis. The survival fraction of bacteria at a given time point = the bioluminescence intensity measured at that time point / the bioluminescence intensity measured right before aBL exposure17.
5. Euthanasia of the Mice
- The endpoints of the experiment are as follows: (a) resolution of the infection as evidenced by the loss of bioluminescence as determined by imaging; (b) occurrence of systematic infections as indicated by the spread of bioluminescence outside of the burned area; (c) loss of ≥15% body weight in comparison to normal age-matched mice, or the suffering from pain and distress as indicated by the lack of responsiveness to manual stimulation, immobility, an inability to eat or drink. During the study, if we encounter a situation where we are unsure whether a mouse has fully reached the status of moribund, as outlined by our definition, and/or we are unsure if we need to euthanize it, we will contact a CCM veterinary staff for a plan of action; (d) otherwise the mice will be euthanized 30 days after the commencement of study.
- Relocate the mice into closed cages specifically for euthanasia and euthanize the mice by delivering carbon dioxide (CO2) compressed gas into the cages.
- Open the CO2 tank or valve regulator to initiate the flow of gas. Verify that the regulator reads the correct psi (pounds per square inch) based on instructions posted by the unit, and adjust the regulator to the correct psi as needed, typically no higher than 5 psi.
- Fill slowly. The flow rate should displace no more than 30% of the chamber/cage volume per min (for a typical mouse cage, ~2 L/min; for a rat cage, ~7.5 L/min).
- Wait approximately 3-5 min for the animal to stop moving or breathing; the eyes should be fixed and dilated. Turn off CO2 tank or regulator valve to stop the flow of CO2.
- Ensure that the heart is not beating by feeling the chest between the thumb and forefinger. Ensure that there is no blink reflex by touching the eyeball.
- If there is a heartbeat or blink reflex, repeat the euthanasia process or use scissors to open the chest cavity to create a pneumothorax (the animal must be non-responsive to a toe pinch prior to performing this procedure).
Representative Results
The A. baumannii strain that we used is an MDR clinical isolate, as reported previously12,17. The bacterial strain was made bioluminescent by the transfection of luxCDABE opera11. Figure 1A shows the successive bacterial luminescence images from a representative mouse burn infected with 5 x 106A. baumannii and exposed to a single aBL exposure at 24 h after bacterial inoculation. A Gram-stain of the histological section of a representative mouse skin burn specimen (harvested at 24 h post-inoculation) demonstrated the presence of A. baumannii biofilms on the surface of the infected burn (Figure 1B). As shown in Figure 1A, the bacterial luminescence was almost eradicated after an exposure of 360 J/cm2 aBL was delivered (60 min of irradiation at an irradiance of 100 mW/cm2). Figure 1C is the dose-response curve of the mean bacterial luminescence from mouse burns infected with 5 x 106A. baumannii and treated with aBL at 24 h after bacterial inoculation (n = 10). To achieve a 3-log10 inactivation of A. baumannii in mouse burns, approximately 360 J/cm2 aBL was required. The bacterial luminescence of the mouse burns unexposed to aBL remained almost unchanged during an equivalent period of time (data not shown; P <0.001).
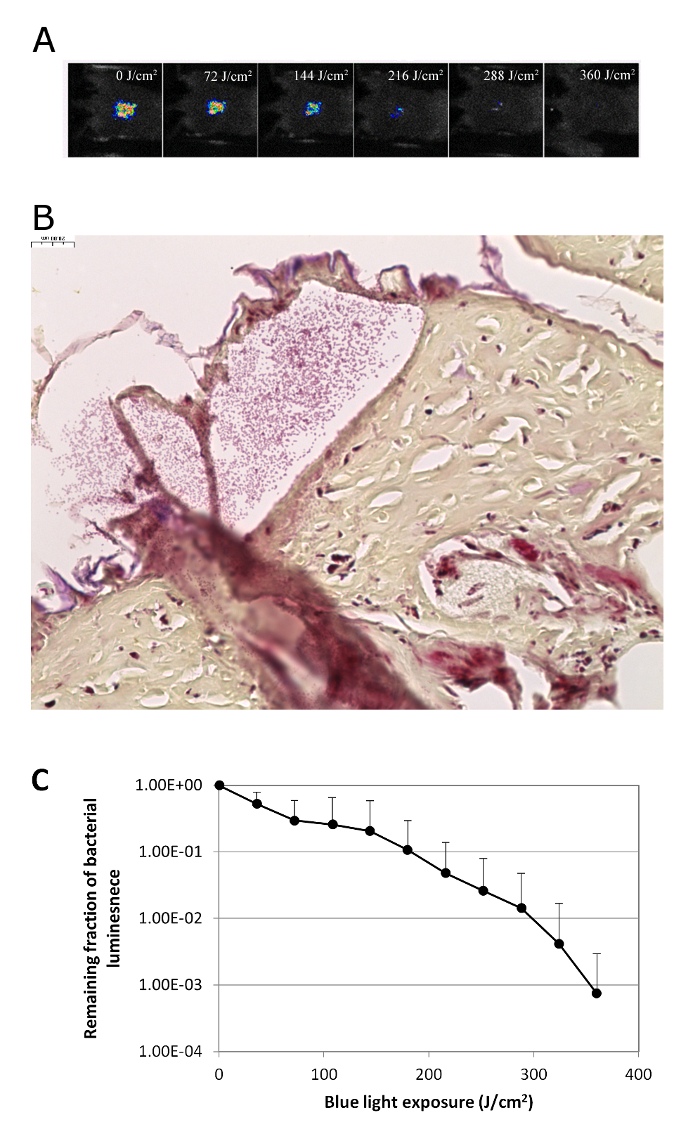
Figure 1: aBL Inactivation of Bacteria in Infected Mouse Burns. (A) Successive bacterial luminescence images from a representative mouse burn infected with 5 x 106 CFU of A. baumannii and exposed to 360 J/cm2 aBL at 24 h after bacterial inoculation. (B) Gram-stained histological section of a representative mouse skin burn showing the presence of A. baumannii biofilms (arrows) in the mouse burn. The skin sample was harvested at 24 h after bacterial inoculation. (C) Dose-response curve of mean bacterial luminescence of mouse burns infected with 5 x 106A. baumannii and treated with an exposure of 360 J/cm2 aBL at 24 h (n = 10) after bacterial inoculation. Bars: standard deviation. Please click here to view a larger version of this figure.
Discussion
aBL is a novel method for treating infections. Since its mechanism of action is completely different from that of chemotherapy, it is more of a physiotherapy. The agent that mediates the antimicrobial effect is blue light irradiation (400-470 nm). With the development of blue LEDs, we gained access to an effective and simple light-based antimicrobial approach for MDR infections.
In this protocol, we have described the development of a mouse model of burn infections caused by a bioluminescent strain of MDR, A. baumannii. With the use of bioluminescent bacteria, the extent of infection can be non-invasively monitored in real time in living animals via bioluminescent imaging. The use of engineered bioluminescent strains of bacteria and the low-light imaging technique creates an efficient technique for monitoring infections in real-time during antimicrobial therapy. This method can also be used in the investigations of infections caused by other microbial species and located at other sites. Besides the efficacy assessment of antimicrobial approaches, this method can also be used to track the progress of infection.
By using this mouse model, we demonstrated that aBL (415 nm) successfully inactivated bacteria in established infections (Figure 1A and C). Prior to aBL therapy, clusters of bacteria were observed in the established infections (Figure 1B), which is a feature of biofilms. Biofilms are more tolerant of traditional antibiotics and host defense compared to their planktonic counterparts6,7 and are frequently associated with persistent infections8,9. The representative results are promising in that 415-nm aBL is biofilm-penetrating. In addition, together with previous reports29,30,31,32, our results demonstrate that the effectiveness of aBL persists regardless of the drug-resistance profile of bacteria.
The protocol described here involves three main procedures: (1) the development of a mouse model of burn infections, (2) aBL therapy, and (3) bioluminescence imaging. While developing a mouse model of burn infections, we noted that there were several factors that affect the extent of infection and the subsequent effectiveness of aBL: (1) The burning time affects the wound depth and the proliferation of bacteria. When the burning time was increased from 3 to 7 s, the bacterial luminescence was much stronger (indicating a higher extent of infection) at 24 h post-inoculation, and the eradication of infection required much higher aBL exposures (>360 J/cm2). (2) The inoculum of the bacteria is a key parameter for the development of infections. A higher bacterial inoculum usually results in a higher extent of infection, while a sufficiently low inoculum frequently fails to develop stable infections in mice. In the latter condition, bacterial luminescence usually becomes undetectable soon after bacterial inoculation. (3) The interaction between bacteria and hosts is dependent upon the bacterial species. We also used P. aeruginosa to develop an infection model. We found that, under the same conditions (i.e., burning time and bacterial inoculum), the infections caused by P. aeruginosa progressed much more rapidly than A. baumannii infections, and sepsis was always observed in mice within 48 h post-inoculation25.
For the execution of aBL therapy, there are several important points that need to be addressed: (1) Proper light irradiance is required for the maximized efficacy of aBL therapy. (2) The surface of the burn in the mice should be placed as horizontally as possible. A failure to appropriately position the burn surface can compromise the efficacy of aBL therapy. (3) During light exposure, it is suggested that the eyes of mice be protected with aluminum foil, especially when a laser is used as the light source. (4) During light exposure, care should be taken to monitor the mice in case they awaken from anesthesia. In this case, a small additional dose of anesthetics should be administrated to keep the animals anesthetized. (5) Both aBL-treated mice and untreated mice should be placed on a heating bed to maintain the body temperature when under anesthesia. During the process of bioluminescence imaging, the bioluminescence of bacteria could decrease when the burns become dry. Therefore, it is recommended to moisturize the mouse burns with PBS before imaging.
There are also some limitations of the techniques discussed in this protocol: (1) For the purpose of monitoring of the extent of infection in real time, bioluminescent bacterial strains must be used. Therefore, before a clinical strain can be tested in the animal model, it must be genetically modified by the transfection of the lux CDABE operon11. (2) The effectiveness of aBL is related to the wavelengths33 and bacterial species/strains34 used. The blue wavelengths, together with other parameters, should be further optimized for inactivating different bacterial species/strains. (3) We only investigated superficial infections in mice. For deep-seated infections, the topical delivery of aBL may not be able to reach the infections, so interstitial light delivery may be needed35. (4) There is a sensitivity limitation of the imaging system, especially when imaging deep infections19. As a result, even when the pixels of bioluminescence are completely eliminated, there might still be viable bacterial cells remaining, allowing bacterial regrowth to occur. An extended exposure to aBL is recommended after the elimination of bacterial luminescence in order to prevent bacterial regrowth.
Declarações
The authors have nothing to disclose.
Acknowledgements
This work was supported in part by the Center for Integration of Medicine and Innovative Technology (CIMIT) under the U.S. Army Medical Research Acquisition Activity Cooperative Agreement (CIMIT No. 14-1894 to TD) and the National Institutes of Health (1R21AI109172 to TD). YW was supported by an ASLMS Student Research Grant (BS.S02.15). We are grateful to Tayyaba Hasan, PhD at the Wellman Center for her co-mentorship for YW.
Materials
| IVIS | PerkinElmer Inc, Waltham, MA | IVIS Lumina Series III | Pre-clinical in vivo imaging |
| Light-emitting diode LED | VieLight Inc, Toronto, Canada | 415 nm | Light source for illumination |
| Power/energy meter | Thorlabs, Inc., Newton, NJ | PM100D | Light irradiance detector |
| Mouse | Charles River Laboratories, Wilmington, MA | BALB/c | 7-8 weeks age, 17-19 g weight |
| Acinetobacter baumannii | Brooke Army Medical Center, Fort Sam Houston, TX | Clinical isolate | Engineered luminescent strain |
| Insulin Syringes | Fisher Scientific | 14-826-79 | BD Lo-Dose U-100 Insulin Syringes for injection |
| Sodium Chloride | Fisher Scientific | 721016 | 0.9% Sodium Chloride |
| Phosphate Buffered Saline, 1X Solution | Fisher Scientific | BP24384 | A standard phosphate buffer used in many biomolecular procedures |
| Brain Heart Infusion | Fisher Scientific | B11059 | Bacterial culture medium |
| Falcon 15mL Conical Centrifuge Tubes | Fisher Scientific | 14-959-70C | For bacterial suspension centrifuge |
| Benchtop Incubated Orbital Shakers | Laboratory Supply Network, Inc, Atkinson, NH | Incu-Shaker Mini | For culturing of bacteria |
| Inoculating Loops | Fisher Scientific | 22-363-605 | For smearing bacterial inoclum on burn surface of mice |
| Fisher Scientific Redi-Tip Pipet Tips, 1-200µL | Fisher Scientific | 02-707-502 | Pipet Tips |
| Thermo Scientific Sorvall Legend X1 Centrifuge | Fisher Scientific | 75-004-220 | For bacterial suspension seperation |
| Brass Block | Small Parts, Inc., Miami, FL | 10 mm by 10 mm | For creation of burns in mice |
| Extreme Dragon PBI/Kevlar High-Heat Gloves | Superior Glove Works Ltd, Cheektowaga, NY | PBI83514 | Heat Resistant Gloves |
| Greiner dishes | Sigma-Aldrich Co. LLC | P5112-740EA | 35 mm ×10 mm |
| Corning Digital Hot Plate | Cole-Parmer Instrument Company, LLC | UX-84301-65 | 10" x 10", 220 VAC, for boiling water |
| Mouse/Rat Thin Line Water Heated Surgical Bed | E-Z Systems | EZ-211 | Prevents heat loss and hypothermia during surgery |
Referências
- Gibran, N. S. Summary of the 2012 ABA Burn Quality Consensus conference. J Burn Care Res. 34 (4), 361-385 (2013).
- Sommer, R., Joachim, I., Wagner, S., Titz, A. New approaches to control infections: anti-biofilm strategies against gram-negative bacteria. Chimia (Aarau). 67 (4), 286-290 (2013).
- Peleg, A. Y., Seifert, H., Paterson, D. L. Acinetobacter baumannii: emergence of a successful pathogen. Clin Microbiol Rev. 21 (3), 538-582 (2008).
- Uppu, D. S. Amide side chain amphiphilic polymers disrupt surface established bacterial bio-films and protect mice from chronic Acinetobacter baumannii infection. Biomaterials. 74, 131-143 (2016).
- Schaber, J. A. Pseudomonas aeruginosa forms biofilms in acute infection independent of cell-to-cell signaling. Infect Immun. 75 (8), 3715-3721 (2007).
- Hoiby, N., Bjarnsholt, T., Givskov, M., Molin, S., Ciofu, O. Antibiotic resistance of bacterial biofilms. Int J Antimicrob Agents. 35 (4), 322-332 (2010).
- Lebeaux, D., Ghigo, J. M., Beloin, C. Biofilm-related infections: bridging the gap between clinical management and fundamental aspects of recalcitrance toward antibiotics. Microbiol Mol Biol Rev. 78 (3), 510-543 (2014).
- Akers, K. S. Biofilms and persistent wound infections in United States military trauma patients: a case-control analysis. BMC Infect Dis. 14, 190 (2014).
- Burmolle, M., et al. Biofilms in chronic infections – a matter of opportunity – monospecies biofilms in multispecies infections. FEMS Immunol Med Microbiol. 59 (3), 324-336 (2010).
- . National strategy on combating antibiotic-resistant bacteria Available from: https://www.whitehouse.gov/sites/default/files/docs/carb_national_strategy.pdf (2014)
- Dai, T. Photodynamic therapy for Acinetobacter baumannii burn infections in mice. Antimicrob Agents Chemother. 53 (9), 3929-3934 (2009).
- Zhang, Y. Antimicrobial blue light therapy for multidrug-resistant Acinetobacter baumannii infection in a mouse burn model: implications for prophylaxis and treatment of combat-related wound infections. J Infect Dis. 209 (12), 1963-1971 (2014).
- Dai, T., et al. Ultraviolet C light for Acinetobacter baumannii wound infections in mice: potential use for battlefield wound decontamination?. J Trauma Acute Care Surg. 73 (3), 661-667 (2012).
- Dai, T. Blue light for infectious diseases: Propionibacterium acnes, Helicobacter pylori, and beyond?. Drug Resist Updat. 15 (4), 223-236 (2012).
- Yin, R. Light based anti-infectives: ultraviolet C irradiation, photodynamic therapy, blue light, and beyond. Curr Opin Pharmacol. 13 (5), 731-762 (2013).
- Haisma, E. M. Inflammatory and antimicrobial responses to methicillin-resistant Staphylococcus aureus in an in vitro wound infection model. PLoS One. 8 (12), e82800 (2013).
- Wang, Y. Antimicrobial Blue Light Inactivation of Gram-Negative Pathogens in Biofilms: In Vitro and In Vivo Studies. J Infect Dis. 213 (9), 1380-1387 (2016).
- Chen, D., Shen, Y., Huang, Z., Li, B., Xie, S. Light-Emitting Diode-Based Illumination System for In Vitro Photodynamic Therapy. Int J Photoenergy. 2012 (2), (2012).
- Demidova, T. N., Gad, F., Zahra, T., Francis, K. P., Hamblin, M. R. Monitoring photodynamic therapy of localized infections by bioluminescence imaging of genetically engineered bacteria. J Photochem Photobiol B. 81 (1), 15-25 (2005).
- Hamblin, M. R., Zahra, T., Contag, C. H., McManus, A. T., Hasan, T. Optical monitoring and treatment of potentially lethal wound infections in vivo. J Infect Dis. 187 (11), 1717-1725 (2003).
- Rowan, M. P. Burn wound healing and treatment: review and advancements. Critical Care. 19, 243 (2015).
- Marx, D. E., Barillo, D. J. Silver in medicine: The basic science. Burns. 40 (Supplement 1), S9-S18 (2014).
- Heyneman, A., Hoeksema, H., Vandekerckhove, D., Pirayesh, A., Monstrey, S. The role of silver sulphadiazine in the conservative treatment of partial thickness burn wounds: A systematic review. Burns. 42 (7), 1377-1386 (2016).
- Roberts, J. A. Individualised antibiotic dosing for patients who are critically ill: challenges and potential solutions. Lancet Infect Dis. 14 (6), 498-509 (2014).
- Dai, T. Blue light eliminates community-acquired methicillin-resistant Staphylococcus aureus in infected mouse skin abrasions. Photomed Laser Surg. 31 (11), 531-538 (2013).
- Uppu, D. S. Amide side chain amphiphilic polymers disrupt surface established bacterial bio-films and protect mice from chronic Acinetobacter baumannii infection. Biomaterials. 74, 131-143 (2016).
- Donlan, R. M., Costerton, J. W. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev. 15 (2), 167-193 (2002).
- Olsen, I. Biofilm-specific antibiotic tolerance and resistance. Eur J Clin Microbiol Infect Dis. , (2015).
- Song, H. H. Phototoxic effect of blue light on the planktonic and biofilm state of anaerobic periodontal pathogens. J Periodontal Implant Sci. 43 (2), 72-78 (2013).
- Rosa, L. P., da Silva, F. C., Viana, M. S., Meira, G. A. In vitro effectiveness of 455-nm blue LED to reduce the load of Staphylococcus aureus and Candida albicans biofilms in compact bone tissue. Lasers Med Sci. 31 (1), 27-32 (2015).
- Guffey, J. S., Wilborn, J. In vitro bactericidal effects of 405-nm and 470-nm blue light. Photomed Laser Surg. 24 (6), 684-688 (2006).
- Enwemeka, C. S., Williams, D., Enwemeka, S. K., Hollosi, S., Yens, D. Blue 470-nm light kills methicillin-resistant Staphylococcus aureus (MRSA) in vitro. Photomed Laser Surg. 27 (2), 221-226 (2009).
- Bumah, V. V., Masson-Meyers, D. S., Cashin, S. E., Enwemeka, C. S. Wavelength and bacterial density influence the bactericidal effect of blue light on methicillin-resistant Staphylococcus aureus (MRSA). Photomed Laser Surg. 31 (11), 547-553 (2013).
- Maclean, M., MacGregor, S. J., Anderson, J. G., Woolsey, G. Inactivation of bacterial pathogens following exposure to light from a 405-nanometer light-emitting diode array. Appl Environ Microbiol. 75 (7), 1932-1937 (2009).
- Kim, M. Optical lens-microneedle array for percutaneous light delivery. Biomedical Optics Express. 7 (1o), 4220-4227 (2016).

