Modeling Paracrine Noncanonical Wnt Signaling In Vitro
Summary
The present study outlines a highly reproducible and tractable method to study paracrine noncanonical Wnt signaling events in vitro. This protocol was applied to evaluate the impact of paracrine Wnt5a signaling in murine neural crest cells and myoblasts.
Abstract
Noncanonical Wnt signaling regulates intracellular actin filament organization and polarized migration of progenitor cells during embryogenesis. This process requires complex and coordinated paracrine interactions between signal-sending and signal-receiving cells. Given that these interactions can occur between various types of cells from different lineages, in vivo evaluation of cell-specific defects can be challenging. The present study describes a highly reproducible method to evaluate paracrine noncanonical Wnt signaling in vitro. This protocol was designed with the ability to (1) conduct functional and molecular assessments of noncanonical Wnt signaling between any two cell types of interest; (2) dissect the role of signal-sending versus signal-receiving molecules in the noncanonical Wnt signaling pathway; and (3) perform phenotypic rescue experiments with standard molecular or pharmacologic approaches.
This protocol was used to evaluate neural crest cell (NCC)-mediated noncanonical Wnt signaling in myoblasts. The presence of NCCs is associated with an increased number of phalloidin-positive cytoplasmic filopodia and lamellipodia in myoblasts and improved myoblast migration in a wound-healing assay. The Wnt5a-ROR2 axis was identified as a crucial noncanonical Wnt signaling pathway between NCC and second heart field (SHF) cardiomyoblast progenitors. In conclusion, this is a highly tractable protocol to study paracrine noncanonical Wnt signaling mechanisms in vitro.
Introduction
Noncanonical Wnt signaling is an evolutionarily conserved pathway that regulates cellular filament organization and directional migration. This pathway has been implicated in multiple biological processes, including embryonic tissue morphogenesis1,2,3, lymphatic and vascular angiogenesis4,5,6,7, and cancer growth and metastasis8,9,10. At the cellular level, noncanonical Wnt signaling is carried out through coordinated paracrine interactions between signal-sending and signal-receiving cells. These interactions frequently occur between cells of different lineages or types and involve a diverse molecular network that includes up to 19 ligands and multiple receptors, co-receptors, and downstream signal transduction effectors11. Further complicating this signaling process, previous studies have shown that ligand-receptor combinations can vary in a context- and tissue-dependent manner12,13, and that the same source ligands that drive noncanonical Wnt signaling in signal-receiving cells can be produced by multiple signal-sending cell types14,15. Given the cellular and molecular complexity associated with noncanonical Wnt signaling, the ability to study individual and clinically relevant mechanisms in vivo has been limited.
Attempts have been made to study noncanonical Wnt signaling using cell culture techniques in vitro. For example, wound-healing assays performed in cellular monolayers have been used to functionally assess cellular directional migration4,16,17,18,19. Immunostaining techniques have been used to perform spatial analyses of surface protein expression to evaluate noncanonical Wnt-induced changes in cellular morphology7,10, architecture, and asymmetric polarization18,19,20. Although these approaches have provided important tools for characterizing Wnt-related phenotypes in signal-receiving cells, the lack of signal-sending components in these protocols limits their ability to accurately model paracrine signaling mechanisms observed in vivo. As a result, there remains a critical need to develop in vitro systems that allow robust and reproducible evaluation of paracrine signaling interactions between signal-sending and receiving cells of the noncanonical Wnt pathway, particularly those of different cell types.
To this end, the primary objective of this study was to establish a protocol to model paracrine noncanonical Wnt signaling interactions in vitro. We developed a non-contact coculture system that recapitulates signal-sending and signal-receiving components of these interactions and allows the use of standard molecular, genetic, or pharmacologic approaches to independently study specific ligand-receptor mechanisms in the noncanonical Wnt pathway. Mechanisms of NCC-mediated Wnt signaling were examined in myoblasts using established murine cell lines. As proof of principle, this model was used to corroborate findings of prior in vivo studies in mice that implicate the Wnt5a-ROR2 axis as a relevant noncanonical Wnt signaling pathway between NCCs21 and SHF cardiomyoblast progenitors3,22,23.
Protocol
1. Preexperimental expansion and passaging of cells
- C2C12 cell culture:
- Prepare 500 mL of C2C12 culture medium by combining Dulbecco's modified Eagle's medium (DMEM) with 10% fetal bovine serum (FBS) and 1 % penicillin/streptomycin.
- Thaw a vial of C2C12 cells in 37 °C water bath. While the C2C12 cells are thawing, add 5 mL of C2C12 medium to a 15 mL conical tube. Immediately transfer the thawed cells to the 15 mL tube using a P1000 pipette.
NOTE: C2C12 cells are murine myoblast cells that have been previously used and validated as a primary cell line for modeling cardiomyoblast progenitors. - Gently mix C2C12 cells in the conical tube using a serological pipette. Then, add the entire volume of thawed cells in C2C12 medium (6 mL) to a 75 cm2 flask.
- Add 6 mL of fresh C2C12 medium to the flask for a total volume of 12 mL. Gently rotate the flask such that the cell and media solution covers the entire bottom of the flask. Place the flask in a cell culture incubator (37 °C, 5% CO2) to allow the cells to adhere.
- Allow the cells to expand in the incubator until they reach ~60% confluency.
NOTE: This can be determined by periodically removing the cells from the incubator and quickly checking their confluency under a microscope. Be sure to minimize the time that cells are removed from the incubator.
- Passaging C2C12 cells:
- Warm the C2C12 medium, 500 mL of 1x PBS, and 0.25% trypsin-EDTA in a 37 °C water bath. After the reagents have been warmed, transfer all the reagents to the cell culture hood.
- Bring the flask containing the C2C12 cells into the cell culture hood. Gently rinse the flask containing the C2C12 cells with warm 1x PBS twice.
- Tilt the flask at a 45° angle and aspirate the C2C12 medium with a glass pipette connected to vacuum suction. While maintaining a 45° angle, carefully add 10 mL of warm 1x PBS to the corner of the flask using a serological pipette. Lay the flask flat on the surface and gently move the flask in circular motions to ensure that the 1x PBS washes over the entire monolayer of cells.
NOTE: Be careful not to disrupt the C2C12 monolayer while aspirating the medium.
- Tilt the flask at a 45° angle and aspirate the C2C12 medium with a glass pipette connected to vacuum suction. While maintaining a 45° angle, carefully add 10 mL of warm 1x PBS to the corner of the flask using a serological pipette. Lay the flask flat on the surface and gently move the flask in circular motions to ensure that the 1x PBS washes over the entire monolayer of cells.
- Remove the 1x PBS after the second wash. Add 1 mL of 0.25% trypsin-EDTA to the flask, gently move the flask as described above to allow the trypsin-EDTA solution to spread over as much of the monolayer as possible and place the flask in the incubator for 2 min.
- After 2 min incubation, remove the flask from the incubator and gently tap it to detach any remaining cells.
- Add 9 mL of C2C12 medium to the flask with a serological pipette to quench the trypsin. Using the serological pipette, gently rinse the cells with the medium and collect the 10 mL of trypsinized cell suspension. Add 10 mL of the cell suspension to a fresh 15 mL conical tube and centrifuge at 100 × g for 5 min.
- Return the conical tube to the cell culture hood and remove the supernatant with a glass pipette connected to vacuum suction. While aspirating the supernatant, take care not to disrupt the cell pellet at the bottom of the conical tube. To do this, leave ~0.2 mL of the supernatant in the conical tube. Resuspend the cells in 10 mL of fresh C2C12 medium.
- For additional passaging, add 1 mL of the resuspended cells into a 75 cm2 flask. Add 11 mL of C2C12 medium to the flask with a serological pipette and place the flask in the incubator.
- STO cell culture:
- Prepare STO culture medium by making 500 mL of DMEM with 7% FBS, 1% penicillin/streptomycin, and 2 nM L-glutamine.
- Prepare 0.1% gelatin by adding 0.5 g of gelatin powder to a bottle containing 500 mL of tissue-grade or autoclaved water. Add 7 mL of 0.1% gelatin solution to a 75 cm2 flask. Rotate the flask such that the gelatin solution covers the entire bottom of the flask. Let the flask incubate for 30 min at room temperature in the cell culture hood.
- Following 30 min incubation, remove the excess gelatin using a pipette connected to vacuum suction. Let the flasks remain in the incubator for another 30 min prior to use.
- Thaw a vial of STO cells in a 37 °C water bath. Using a P1000 pipette, immediately transfer the thawed cells to a 15 mL conical tube containing 5 mL of freshly prepared STO culture medium.
NOTE: STO cells are murine embryonic fibroblasts routinely used as feeder cells in cell culture protocols. - Gently mix the cells in the conical tube using a serological pipette. Add the entire volume (6 mL) of cells to a gelatin-coated 75 cm2 flask. Rotate the flask to ensure that the cell suspension is well distributed along the bottom of the flask.
- Add 6 mL of fresh STO medium to the flask for a total volume of 12 mL. Rotate the flask as described above to ensure that the cells and medium are well distributed along the bottom of the flask. Place the flask in the 37 °C incubator to allow the cells to adhere. Allow the cells to proliferate in the incubator until they reach ~60-70% confluency.
- Passaging STO cells:
- Warm STO cell medium, 1xPBS, and 0.25% trypsin-EDTA in a 37 °C water bath.
- Gently rinse the flask containing STO cells with warm 1x PBS twice as described in step 1.2.2.1.
- Add 1 mL of 0.25% trypsin-EDTA to the flask using a P1000 pipette. Place the flask in the 37 °C incubator for 5 min.
- After 5 min incubation, remove the flask from the incubator. Gently tap the flask to detach any adherent cells.
- Add 9 mL of STO medium to the flask to quench the trypsin and collect the 10 mL of trypsinized cell suspension as described above. Add 10 mL of the cell suspension to a 15 mL conical tube and centrifuge at 100 × g for 5 min.
- Remove the supernatant and resuspend the cells in 10 mL of STO medium as described above. For additional passaging, add 1 mL of the resuspended cells into a 75 cm2 flask. Add 11 mL of STO medium, rotate the flask to ensure even distribution of the cells and medium along the bottom of the flask, and place the flask in the incubator.
- Inactive STO cell culture and O9-1 cell basal medium preparation:
- Prepare O9-1 cell basal culture medium by mixing 500 mL of DMEM with 15% FBS, 1% penicillin/streptomycin, 2 nM L-glutamine, 0.1 mM minimum nonessential amino acids, 1 nM sodium pyruvate, and 55 µM beta-mercaptoethanol.
- Prepare mitomycin C solution in 1x PBS at a concentration of 0.5 mg/mL by adding 4 mL of 1x PBS directly to a mitomycin C vial. Pipette the solution multiple times with a P1000 pipette. To further dissolve the mitomycin C in 1x PBS, place the vial on a vortex mixer or benchtop rocker for 45 min to 1 h.
- Inactivate the STO cells by treating the STO plates with a final concentration of 0.01 mg/mL mitomycin C added to the standard STO medium. Place the STO plates inside the incubator for 2 h, taking care to protect the flask containing mitomycin C from light by minimizing the time spent outside the incubator. Following mitomycin treatment, wash the cells in 1x PBS twice as described in step 1.2.2.1.
NOTE: Mitomycin C inhibits the proliferation of STO cells so that they can be used to generate conditioned medium over several days without becoming overconfluent in the flask. - After removing the 1x PBS, add 12 mL of O9-1 basal culture medium to the inactivated STO cell cultures and incubate them for 24 h. Collect the conditioned, inactivated STO + O9-1 basal culture medium and place it in 50 mL conical tubes wrapped in foil to protect it from light.
- Add 12 mL of fresh O9-1 basal culture medium to the inactivated STO cell cultures as described above. Repeat this step by adding fresh O9-1 basal culture medium to the same flanks containing the inactivated STO cells every 24 h.
NOTE: Following mitomycin C treatment, the inactivated STO cells cannot proliferate; hence, the flasks containing the inactivated STO cells can be reused to generate conditioned medium. - Store the foil-wrapped 50 mL conical tubes containing conditioned, inactivated STO + O9-1 basal culture medium at 4 °C until a total of 500 mL of the medium has been collected.
- O9-1 cell culture:
- Prepare O9-1 cell growth culture medium using 500 mL of conditioned STO + O9-1 basal medium, and add 103 units of leukemia inhibitory factor (LIF) and 25 ng/mL basic fibroblast growth factor (basic-FGF).
- Prepare 0.1% gelatin-coated flasks as described in steps 1.3.2-1.3.3.
- Thaw a vial of O9-1 cells in a 37 °C water bath. Immediately transfer the thawed cells to a 15 mL conical tube containing 5 mL of freshly prepared O9-1 growth medium.
NOTE: The O9-1 cell line is the only stable, multipotent neural crest cell line that has been generated from the mouse. This cell line is commonly used in neural crest in vitro experiments. - Gently mix the cells using a serological pipette. Add the entire 6 mL of cells to a gelatin-coated 75 cm2 flask.
- Add 6 mL of O9-1 growth medium to the flask for a total volume of 12 mL. Place the flask in the 37 °C incubator to allow the cells to adhere. Allow the cells to proliferate in the incubator until they reach ~60-70% confluency.
- Passaging O9-1 cells:
- Warm O9-1 growth medium, 1x PBS, and 0.25% trypsin-EDTA in a 37 °C water bath.
- Gently rinse the plate containing O9-1 cells with warm 1x PBS twice as described in step 1.2.2.1.
- Add 1 mL of 0.25% trypsin-EDTA to the flask and place it in the 37 °C incubator for 5 min.
- After 5 min incubation, remove the flask from the incubator and tap the flask gently to detach any adherent cells.
- Add 9 mL of O9-1 growth medium to the flask to quench the trypsin. Collect 10 mL of the trypsinized cell suspension and add 10 mL of this cell suspension to a 15 mL conical tube. Centrifuge the tube at 100 × g for 5 min.
- Remove the supernatant and resuspend the cells in 10 mL of O9-1 growth medium. For additional passaging, add 1 mL of the resuspended cells to a 75 cm2 flask. Add 11 mL of O9-1 growth medium and place the flask containing the cells in 12 mL of medium in the 37 °C incubator.
2. Plating cells in a coculture system
- Plating C2C12 cell chambers:
- Following trypsinization (as described in step 1.2), resuspend the C2C12 cell pellet in 10 mL of C2C12 medium. Dilute the cells in a 1:20 ratio in C2C12 medium by removing 0.5 mL of the resuspended C2C12 cells and adding them to a new 15 mL conical tube containing 9.5 mL of fresh C2C12 medium. Gently mix the suspension with a serological pipette.
- Add 1 mL of the 1:20-diluted C2C12 cells to each well of a new 4-chambered well using a P1000 pipette and place the 4-chambered well in the incubator.
- Plating O9-1 cell inserts:
- Following trypsinization, resuspend the O9-1 cell pellet in 10 mL of O9-1 growth medium. Dilute the cells in a 1:20 ratio in O9-1 growth medium by removing 0.5 mL of the resuspended C2C12 cells and adding them to a new 15 mL conical tube containing 9.5 mL of fresh O9-1 growth medium. Gently mix the suspension with a serological pipette.
- Place a single permeable insert (see the Table of Materials) inside each well of a new 4-chambered well filled with 1 mL of O9-1 growth medium.
NOTE: This 4-chambered well should be different from that containing the C2C12 cells from step 2.1.3. - Add 300 µL of the diluted O9-1 cell suspension to each insert using a P1000 pipette. Ensure that the bottom of each insert is submerged within the well filled with 1.3 mL of O9-1 growth medium. Place the well in the 37 °C incubator.
- (Optional). Perform siRNA knockdown in the O9-1 cells or C2C12 cells.
- Perform gene knockdown by siRNA 18-24 h after plating either O9-1 cell inserts or C2C12 cell chamber wells.
- Dilute the siRNA and transfection reagent in reduced-serum medium (see the Table of Materials) according to the manufacturers' recommendations and the desired concentrations for the experiment. Gently mix the diluted siRNA and transfection reagent (1:1) and incubate the mixture at room temperature for 7 min.
NOTE: In this protocol, 50 nM concentrations were used as this siRNA concentration was determined to result in sufficient knockdown of target gene expression. - Add the siRNA-lipid complexes to either the O9-1 cell inserts or the C2C12 cell chamber wells as determined by the experimental design and incubate the cells with the siRNA-lipid complexes for ~36-48 h.
- Dilute the siRNA and transfection reagent in reduced-serum medium (see the Table of Materials) according to the manufacturers' recommendations and the desired concentrations for the experiment. Gently mix the diluted siRNA and transfection reagent (1:1) and incubate the mixture at room temperature for 7 min.
- Perform gene knockdown by siRNA 18-24 h after plating either O9-1 cell inserts or C2C12 cell chamber wells.
3. Performing wound assay and quantitatively assessing myoblast migration
- Wound assay:
- Allow the O9-1 cell inserts and C2C12 cell chamber wells to adhere and proliferate in the incubator until both cells are at ~70-80% confluency before proceeding with this portion of the protocol. If cells grow >90% confluent, do not proceed with the scratch assay, as cells will merely detach from the well.
- Warm 1x PBS and C2C12 medium by placing them in a 37 °C water bath.
- Remove supernatant medium from the C2C12 chamber well and wash the cells once with 1x PBS. Remove the 1x PBS and immediately scratch the cells with a sterile P10 pipette tip.
- Pass the sterile P10 pipette tip firmly in a single direction to span the entire length or width of the cell monolayer (e.g., right to left, top to bottom). Be sure to scratch each well containing cells only once.
NOTE: To optimize scratching results, scratch wells of different experimental conditions at a similar level of confluency. To do this, ensure that each 4-chambered well has cells for each required experimental condition (e.g., well #1 negative control, well #2 positive control). In addition, use a new sterile P10 pipette for each scratch and apply a similar amount of force to the pipette each time. Do not attempt to create more than one scratch in each well. - After scratching, quickly add 1 mL of 1x PBS back into the well using a P1000 pipette tip. Repeat this process for each well that will be scratched.
NOTE: Given the variability associated with each scratch, it is recommended that multiple wells (n = 3) are used for wound creation in each experimental condition. Work expeditiously as it is critical to minimize the duration for which the cells are without 1x PBS during these steps. After removing 1x PBS from each well, one should not take more than 5 s to generate a wound in each well.
- Pass the sterile P10 pipette tip firmly in a single direction to span the entire length or width of the cell monolayer (e.g., right to left, top to bottom). Be sure to scratch each well containing cells only once.
- After generating a wound and adding 1x PBS back into each well, image the scratch using a brightfield inverted microscope and use this image as the baseline wound size (time 0). To take images, perform the following steps:
- Turn on the computer and the microscope (see the Table of Materials) by pressing the power button. Place the chamber slide on the stage and rotate the objective dial to 5x magnification.
- Open the imaging software (see the Table of Materials) by double-clicking the software icon on the computer desktop. Click the Camera tab on the software home screen. Click the Live button to visualize the cells on the AxioCam IC tab.
- Ensure that the light filter is pulled all the way out to allow light to pass to the camera and computer screen. Manually move and/or rotate the chamber slide to position the wound area in the center of the live image on the AxioCam IC tab.
- To take images, click snap to open a new tab next to the AxioCam IC tab that contains the image.
- To save this still image, click file on the top left of the software home page | save as | enter the file name in the file name box. Save the figure in Carl Zeiss image (*.czi) format (the default setting), and select desktop on the bar on the left to save the file to the desktop as a .czi file, which can only be opened in the Zen lite 2012 software program.
- To save the picture as a .tiff, click file | save as | enter file name in the file name box. Save the figure as tagged image file (*.tiff) by clicking the save as type button and selecting *.tiff from the dropdown menu.
NOTE: The .tiff format can be opened in any image processing software. - Manually reposition the chamber slide to take 2-3 more images at other points of the wound in the same well.
NOTE: In total, this will result in 3-4 non-overlapping, high-magnification images of the wound in each well.
- Remove the 1x PBS from each well and add 1 mL of C2C12 medium.
NOTE: Be cautious not to pipette too aggressively when removing or adding solutions to the chamber well following wound generation, as this may cause cells to detach from the chamber well. In addition, tilt the chamber well so that aspiration and reintroduction of solutions can be done at the corners of each well to minimize cell monolayer disruption. - Assemble the well insert coculture system by manually placing the inserts containing the O9-1 cells in each well of the chamber well. Gently push the inserts down into the well such that the bottom of the insert sits just above the underlying C2C12 cells. Return the well insert constructs to the incubator.
NOTE: Do not allow the bottom of the insert to physically touch and mechanically disrupt the underlying C2C12 cells. - Allow the cells to migrate for a total of 9-12 h. To determine the optimal migration time, check the cells at 6 h following wound creation, then every 2-3 h thereafter. End the experiment when the cells in control or positive control conditions begin to completely cover the wound.
NOTE: Given the non-contact nature of the construct, the overlying insert does not need to be removed from the wells when checking interval migration progression. Migratory variability will be observed depending on factors such as the cell types used in this assay, cellular density at the time of wound generation, the width of the wound created, and experimental conditions of manipulated cells (e.g., gene knockdown, recombinant protein addition). Concentrations of these reagents should be determined experimentally with guidance from manufacturer recommendations.
4. Immunofluorescence staining and imaging of migrating myoblasts
- Terminating the migration assay and deconstructing the well insert system:
- Remove the O9-1 cell inserts after a 9-12 h migration period (or alternative time designated by experimental conditions). Carefully aspirate the C2C12 medium using a P1000 pipette. Add 0.5 mL of 1x PBS to the chamber wells, and take final images of cells following migration.
- Carefully aspirate all 0.5 mL of 1x PBS mixed with medium and remove the plastic chambers from the chamber wells using kit instructions, leaving the underlying slide containing the C2C12 cells.
NOTE: Be careful not to disrupt the C2C12 cells adherent to the slide when removing the chamber wells.
- Performing immunostaining:
- Immediately place the slide in a slide holder containing 4% paraformaldehyde (PFA) and incubate for 10 min at room temperature. Pour out the 4% PFA and add 0.1% Triton X-100-containing 1x PBS (1x PBST) to the slide holder to wash the slide for 15 min at room temperature. Pour out the 1x PBST and add 1x PBS to the slide holder to wash the slide for 10 min at room temperature. Repeat this step once more for a total of two 1x PBS washes.
- Remove the slide from the slide holder. Trace the outer edges of the slide with a hydrophobic pen to create a hydrophobic boundary around the slide to prevent solutions from spilling from the slide. Take care not to disrupt the adherent cells.
- Add 1% bovine serum albumin (BSA) blocking solution (diluted in 1x PBS) to the slide (~0.5 mL per slide). Ensure that the solution is contained within the hydrophobic boundary created in step 4.2.4. Incubate the slide for 1 h at room temperature in a humidified slide chamber.
NOTE: Although BSA blocking is not required for phalloidin immunostaining, this step in the protocol allows for coupling with fluorescence antibody staining. - After blocking for 1 h, pour out the blocking solution from the slide, add phalloidin antibody (diluted to 1:200 in 1% BSA blocking solution by adding 5 µL of the antibody to 995 µL of BSA solution) to the slide and incubate at 4 °C overnight. Again, ensure that the solution is contained within the hydrophobic boundary created in step 4.2.4. Given that the phalloidin antibody is conjugated to Alexa Fluor-488 dye, minimize light exposure of the antibody reagent before and after adding to the slide.
- The following day, place the slide in a slide holder protected from light exposure (e.g., wrap the slide holder in foil or use a non-transparent slide holder). Wash the cells in the slide holder with 1x PBS for 10 min at room temperature. Repeat the wash for a total of three 10 min washes.
- Add 4',6-diamidino-2-phenylindole (DAPI)-containing mounting medium and mount the slides with glass coverslips. Image the cells that have migrated using a standard fluorescence microscope.
Representative Results
Effects of NCCs on migratory capacity of murine myoblasts
This assay was first applied to evaluate the impact of NCCs on the migratory capacity of myoblasts. Figure 1 outlines the schematic model of the assay. To test this impact, scratch assays were performed with myoblasts that were grown in isolation (without NCC inserts) compared to those grown in the presence of inserts. As a positive control, 500 ng/mL of recombinant Wnt5a (rWnt5a) was added to chamber wells with NCC inserts. This concentration of rWnt5a was determined by a dose-response analysis performed in C2C12 cells (Supplemental Figure S1). Representative images of NCC inserts are shown in Supplemental Figure S2, demonstrating that the NCCs are healthy at this time point. Immunofluorescence demonstrates robust knockdown of Wnt5a at the protein level following incubation with 50 nM of Wnt5a siRNA (Supplemental Figure S3). Following a 9 h migration period, it was found that the presence of NCCs significantly increased the migratory capacity of myoblasts compared to myoblasts assayed in the absence of NCC inserts (72.6% wound-repopulated area vs 59.1% wound-repopulated area, p = 0.033). The addition of rWnt5a to coculture wells accelerated myoblast migration, with some wound areas demonstrating complete recovery by the 9 h time point, as shown in Figure 2. As expected, migratory myoblasts in all three conditions exhibited normal migratory cellular morphology, including well-formed and protruding filopodia and lamellopodia and asymmetric polarization of actin cytoskeletal projections (Figure 2C).
Importance of NCC-derived Wnt5a for polarized migration of myoblasts
To evaluate the paracrine effect of NCC-derived Wnt5a on myoblast migration, wound-healing assays were performed in myoblasts following the siRNA-mediated knockdown of Wnt5a in NCCs. First, Wnt5a knockdown efficiency was validated in NCCs by real time-quantitative polymerase chain reaction. Treatment with 50 nM siRNA against Wnt5a was found to reduce Wnt5a gene expression by 64% compared to negative control (scrambled) siRNA (Figure 3A). Using this concentration, O9-1 cell inserts were transfected with either control siRNA or Wnt5a siRNA 48 h prior to assembling the coculture. C2C12 cells were grown under normal conditions, and wounds were created at the appropriate confluency. Immediately following wound generation, negative control or Wnt5a knockdown NCC inserts were added to each well. After a 10 h migration period, it was found that knockdown of Wnt5a in NCCs significantly reduced underlying myoblast migratory capacity compared to myoblasts assayed with control NCCs (39.1% wound-repopulated area vs 74.8% wound-repopulated area, p < 0.001). Moreover, myoblasts assayed in the presence of NCCs with knockdown of Wnt5a displayed abnormal cytological morphology by immunostaining, including reduced cytoplasmic areas and fewer actin cytoskeletal projections (Figure 3D). To rescue myoblast migration, exogenous supplementation of 500 ng/mL of rWnt5a was added to coculture wells containing Wnt5a knockdown inserts. The addition of exogenous rWnt5a was found to completely rescue migratory and morphologic defects observed in these myoblasts (Figure 3C,D).
Wnt5a signaling through ROR2 in myoblasts as a driver of polarized migration
To better understand the signal-receiving cell mechanisms in this paracrine model, the assay was repeated following the knockdown of the ROR2 receptor in myoblasts. In this experiment, myoblasts were transfected with 50 nM of ROR2 siRNA ~40 h prior to wound generation, which was shown to be sufficient to knock down ROR2 gene expression by 54% (Figure 4A). During this time, NCC inserts were grown in parallel under normal conditions. After myoblasts reached appropriate confluency, scratch assays were performed, and coculture well inserts were assembled. After a 10 h migration period in the presence of NCC inserts, ROR2 knockdown myoblasts demonstrated reduced migratory capacity compared to myoblasts treated with negative control siRNA (48.1% wound-repopulated area vs 75.7% wound-repopulated area, p = 0.019) (Figure 4B,C). The addition of 500 ng/mL rWnt5a failed to rescue myoblast migratory capacity following ROR2 knockdown, suggesting that ROR2 depletion disrupts the ability of myoblasts to receive Wnt5a signals (Figure 4B,C). Immunostaining for phalloidin corroborated the migratory data and showed that a reduction in phalloidin-positive lamellopodia and filopodia in ROR2 knockdown myoblasts was not restored by supplemental rWnt5a (Figure 4D).
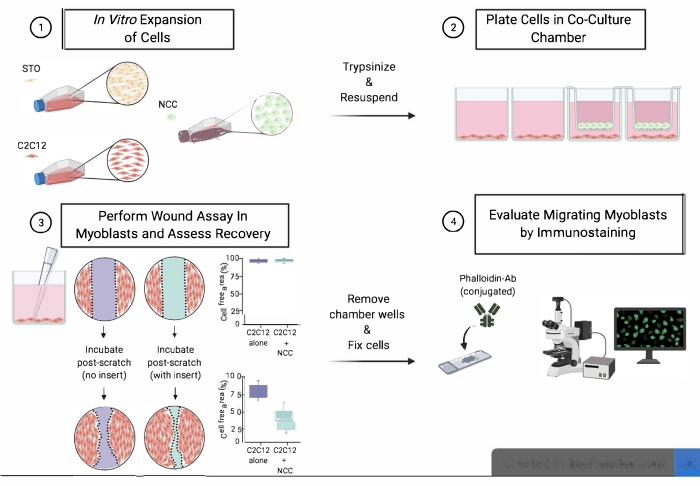
Figure 1: Schematic model of the assay. Step 1 includes the in vitro expansion of C2C12 myoblasts and NCCs using STO feeder cells. Step 2 involves the plating of NCCs and C2C12 cells in the coculture system. Step 3 includes the wound assay performed in underlying C2C12 cells to evaluate cellular migratory capacity. Step 4 involves immunostaining for phalloidin to evaluate cytological architecture and morphology of migrated cells. Abbreviations: NCCs = neural crest cells; Ab = antibody. Please click here to view a larger version of this figure.
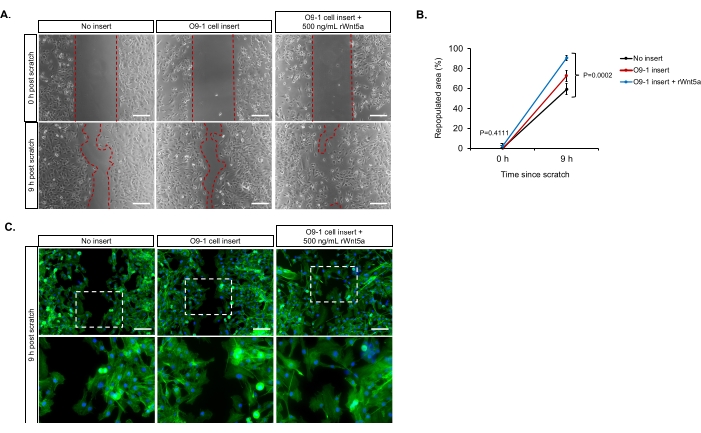
Figure 2: Presence of neural crest cells increases myoblast migratory capacity. (A) The presence of neural crest cell (NCC) inserts at the time of wound generation leads to improved myoblast migration. The addition of exogenous recombinant Wnt5a (rWnt5a) to NCC-C2C12 cocultures has the strongest positive effect on myoblast migration. (B) Quantification of average myoblast repopulated area at 9 h following wound generation (error bars show standard deviation). (C) Phalloidin staining of myoblasts at the wound border 9 h following wound generation. Dashed rectangles show phalloidin-stained myoblasts at the migratory front. A total of n = 3 samples were used for each experimental condition quantified in B. Scale bars = 200 µm (for A and C). Please click here to view a larger version of this figure.
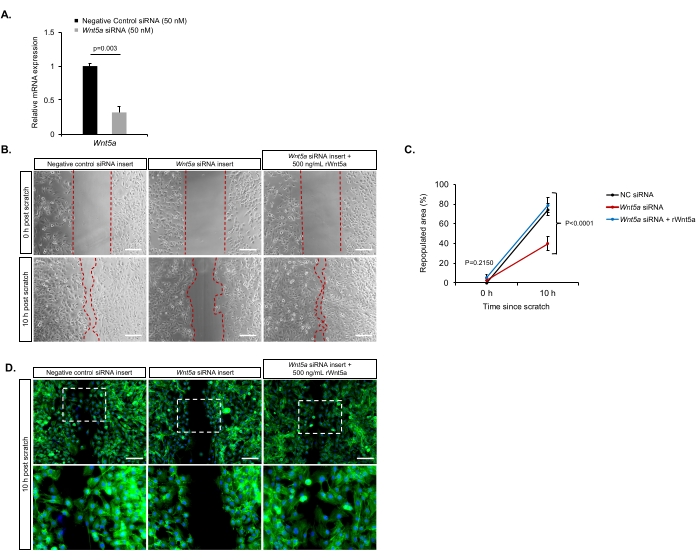
Figure 3: Neural crest cell-derived Wnt5a is necessary for myoblast migration. (A) Relative mRNA expression of Wnt5a to validate siRNA-mediated knockdown in NCCs. (B) Migration of C2C12 myoblasts is significantly reduced following Wnt5a knockdown in NCCs. Addition of exogenous rWnt5a is sufficient to rescue this migratory deficit in myoblasts. (C) Quantification of average myoblast-repopulated area at 10 h following wound generation (error bars show standard deviation). (D) Phalloidin staining of myoblasts at the wound border 10 h following wound generation. Dashed rectangles show phalloidin-stained myoblasts at the migratory front. A total of n = 3 samples were used for each experimental condition quantified in C. Scale bars = 200 µm (for B and D). Abbreviations: NCCs = neural crest cells; siRNA = small interfering RNA. Please click here to view a larger version of this figure.
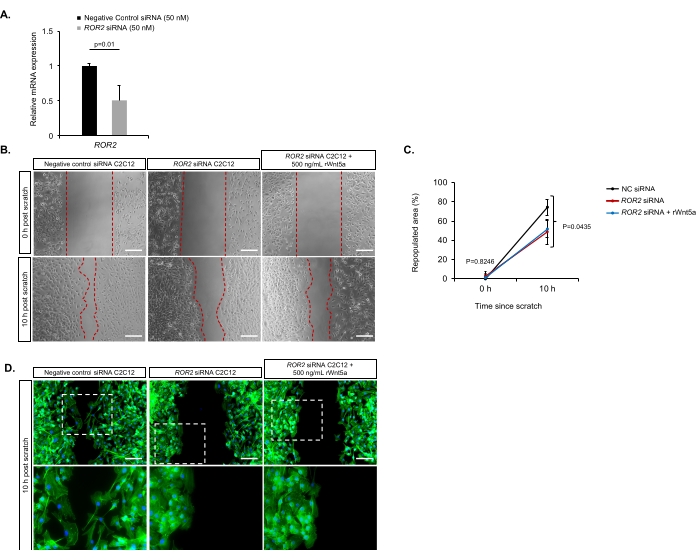
Figure 4: Wnt5a signals through ROR2 receptors in myoblasts to drive migration. (A) Relative mRNA expression of ROR2 to validate siRNA-mediated knockdown in C2C12 cells. (B) Knockdown of ROR2 in myoblasts reduces their migratory capacity despite the presence of NCCs. Exogenous rWnt5a fails to rescue myoblast migration after ROR2 knockdown. (C) Quantification of average myoblast-repopulated area at 10 h following wound generation (error bars show standard deviation). (D) Phalloidin staining of myoblasts at the wound border 10 h following wound generation. Dashed rectangles show phalloidin-stained myoblasts at the migratory front. A total of n = 3 samples were used for each experimental condition quantified in C. Scale bars = 200 µm. Abbreviations: NCCs = neural crest cells; siRNA = small interfering RNA. Please click here to view a larger version of this figure.
Supplemental Figure S1: Dose-dependent analysis for recombinant Wnt5a supplementation. Dose-dependent analysis for recombinant Wnt5a supplementation testing 0 ng/mL, 100 ng/mL, and 500 ng/mL found 500 ng/mL of exogenous rWnt5a to be the optimal concentration to drive myoblast migration and phalloidin cytoarchitectural changes during a 12 h migratory period in vitro. Scale bars = 200 µm. Please click here to download this File.
Supplemental Figure S2: Representative images of well inserts. Brightfield images of well inserts containing O9-1 neural crest cells treated with (A) 50 nM negative control siRNA and (B) 50 nM Wnt5a siRNA. Scale bars = 200 µm. Abbreviation: siRNA = small interfering RNA. Please click here to download this File.
Supplemental Figure S3: Representative images of Wnt5a protein expression in O9-1 cells following siRNA-mediated Wnt5a knockdown. Immunofluorescence staining of Wnt5a protein in cell culture wells containing O9-1 neural crest cells treated with (A) 50 nM negative control siRNA and (B) 50 nM Wnt5a siRNA. Scale bars = 20 µM. Abbreviations: siRNA = small interfering RNA; DAPI = 4',6-diamidino-2-phenylindole. Please click here to download this File.
Discussion
The noncanonical Wnt/planar cell polarity (PCP) signaling pathway is a critically important cellular signaling pathway that has been implicated in multiple developmental24,25 and disease processes24,26. During embryonic development, noncanonical Wnt signaling involves an expansive network of molecular signals from signal-sending cells that ultimately induce changes in morphology, asymmetric organization, and directional migration in signal-receiving cells11. Previous studies have shown that the specific ligand-receptor pathways that drive this signaling are diverse, context-dependent, and often vary between cell types12,13,14,15. Owing to this molecular complexity, the ability to assess paracrine noncanonical Wnt signaling interactions using conventional genetic recombination methods in vivo has been limited. While in vitro systems have increasingly been used as an alternative approach to study noncanonical Wnt cellular phenotypes, available protocols focus exclusively on downstream signal-receiving aspects of the pathway and fail to sufficiently model the intercellular and paracrine nature of these signaling events. Therefore, the objective of the present study was to develop a protocol for a non-contact coculture system that recapitulates paracrine Wnt interactions in vitro. The focus of this protocol was to model two characteristic aspects of functional noncanonical Wnt signaling in vitro, including the organization of intracellular filament proteins and polarized migratory capacity.
As a proof of concept, this protocol was applied to study paracrine mechanisms in the context of heart development. During cardiogenesis, reciprocal signaling events between cardiac NCCs and SHF progenitor cells are crucial for the appropriate maturation of the cardiac outflow tract (OFT)27,28,29. Previous work has shown that during mouse cardiac development, NCC-mediated Wnt/PCP signaling in pharyngeal SHF cells is required for SHF progenitor cell incorporation into the developing OFT and for normal OFT alignment21. Schleiffarth et al. and others have shown that genetic knockout of the gene encoding the Wnt/PCP ligand, Wnt5, has been shown to disrupt SHF progenitor cell organization and migratory capacity, resulting in a foreshortened and misaligned cardiac OFT22,23,30. With established murine NCC (O9-1)31 and myoblast (C2C12) cell lines, this protocol demonstrates that coculture with NCCs is associated with increased phalloidin-positive cytoplasmic filopodia and lamellipodia and improves myoblast migratory capacity in a wound-healing assay. These molecular and functional endpoints in vitro build on previously published protocols for NCC manipulation31 and closely model the in vivo phenotypic changes described in Wnt5a global knockout mice, validating the utility of this model.
To determine the specific molecular pathway driving noncanonical Wnt signaling between NCCs and myoblasts, parallel cell-specific knockdown experiments for the genes encoding the candidate ligand, Wnt5a, in NCCs and its corresponding receptor, ROR2, in myoblasts were performed. As expected, knockdown of molecules in both signal-sending (Wnt5a in NCCs) and signal-receiving (ROR2 in myoblasts) cells independently disrupted Wnt/PCP-related actin cytoarchitectural changes and inhibited myoblast migration. Importantly, phenotypic rescue with recombinant Wnt5a was only observed in the NCC-Wnt5a knockdown condition, which supports a mechanism whereby NCC-derived Wnt5a activates PCP signaling in myoblasts through ROR2 receptors. These results are consistent with data from mouse genetic studies that identify the Wnt5a-ROR2 axis as a crucial Wnt/PCP signaling axis between NCCs and SHF cells during embryonic heart development3,21. Though not experimentally tested in this protocol, it remains unclear if SHF-derived Wnt5a provides reciprocal paracrine signals to the neural crest through ROR2 receptors. This hypothesis could be tested using this protocol by repeating the experiments with C2C12 cells on the top and O9-1 cells on the bottom of the well insert construct. If SHF-derived Wnt5a does provide a reciprocal paracrine signal through NCC-ROR2, then one would expect the knockdown of Wnt5a in C2C12 cells to inhibit migratory capacity and actin polymerization of the underlying O9-1 cells.
There are several unique strengths of this protocol. First, it is a non-contact well insert system that incorporates the sequential use of wound-healing assays and immunostaining techniques to evaluate functional and molecular Wnt/PCP characteristics in the same population of signal-receiving cells. This not only provides a robust approach to phenotyping noncanonical Wnt-induced intracellular filament organization and polarized migratory changes in vitro but also permits more granular assessments of signal transduction mechanisms. While this protocol provides proof of principle regarding Wnt5a-ROR2 molecules, the model also easily lends itself to evaluating the effects of other ligands and receptors in the noncanonical Wnt signaling pathway. One can further adapt the immunostaining protocol to evaluate the expression of multiple potential downstream effector proteins (e.g., RhoA, p-JNK, Daam1, Rac1) that have been shown to transduce noncanonical Wnt signals in vivo. In addition, protein levels of these various effector molecules can be correlated with either migratory or actin cytoarchitecture phenotypes. Second, the non-contact nature of the coculture system allows for the independent manipulation of specific signal-sending versus signal-receiving molecules in the Wnt/PCP pathway. In these representative results, it was elected to perform cell-specific siRNA knockdown. However, this protocol is also amenable to the use of pharmacologic inhibitors or genetically modified cell lines to evaluate candidate ligand-receptor pathways for clinical application. Similarly, one can perform phenotypic rescue experiments by adding molecular or pharmacologic compounds to the coculture medium, as was shown with recombinant Wnt5a. Targeting these compounds to selectively rescue signal-sending versus signal-receiving derangements further validates paracrine mechanistic pathways in ways that are not permitted using current in vivo model systems.
There are many critical steps of this protocol. First, it is important to ensure that primary cells are expanded and maintained at the appropriate confluency throughout the protocol. If C2C12 myoblasts are allowed to proliferate to 100% confluency, they will begin to fuse and differentiate from myoblasts into myotubes. Hence, these cells must be passaged at the appropriate density as described. Second, given that STO feeder cells are needed to generate conditioned medium to grow O9-1 cells, it is imperative that one appropriately inactivates STO cells with mitomycin C and makes sufficient (at least 500 mL) O9-1 growth medium using inactivated STO cells prior to thawing and plating O9-1 cells. Perhaps the most critical step in this protocol is the generation of appropriate scratches with uniform geometry and width in the myoblast monolayer32,33. Step 3.1.4 details several tips for optimizing this part of the protocol. Despite these recommendations, it should be acknowledged that the variability associated with standard 2D scratch assays remains a technical challenge and a limitation of this protocol. Therefore, it is necessary to have multiple technical replicates of each experimental condition.
Finally, although the results presented here were generated using murine NCCs and myoblasts, this protocol can, in principle, be adapted to include any signal-sending and signal-receiving cell of interest. As a result, this system not only has applications for advancing basic mechanisms of paracrine noncanonical Wnt signaling in a variety of developmental contexts, but it can also be used to test therapeutic mechanisms for Wnt/PCP-related disease processes. Examples include pharmacologic screening for drugs that inhibit the Wnt/PCP-induced migratory capacity of malignant cells or restore directional migration of patient-derived terminal cell types with defective PCP signaling capacity at baseline. Beyond the noncanonical Wnt signaling pathway, this protocol can also be adapted to study other paracrine signaling mechanisms and pathways between two cell types. For example, siRNA-mediated knockdown of known secretory molecules in other pathways (e.g., Notch, Bmp/Tgf-β, Fgf) in O9-1 cells can be coupled with immunostaining of proliferative, differentiation, or apoptotic markers in underlying myoblasts.
In conclusion, this protocol establishes a novel and highly tractable experimental protocol to study mechanisms of noncanonical Wnt-related intracellular filament organization and polarized migration in vitro. The methods described here improve upon existing techniques by maintaining the intercellular and paracrine nature of Wnt interactions and allow for the independent assessment of signal-sending versus signal-receiving components of this pathway. This protocol can be broadly applied to investigate basic paracrine Wnt/PCP signaling mechanisms between two cell types and screen for new therapeutic compounds targeting Wnt/PCP-related disease processes.
Declarações
The authors have nothing to disclose.
Acknowledgements
This work was supported in part by NIH awards F30HL154324 to O.T. and K08HL121191 and R03HL154301 to S.R.K. The authors would like to acknowledge that the schematic in Figure 1 in this manuscript was created with biorender.com.
Materials
| 2-Mercaptoethanol | Sigma Aldrich | M-7522 | |
| Antifade mounting medium with DAPI | Vector Laboratories | H-1200-10 | Stored at 4 °C |
| Bovine serum albumin | Santa Cruz Biotechnology | sc-2323 | Stored at 4 °C |
| C2C12 murine myoblast cell line | ATCC | CRL-1772 | |
| Cell culture flasks, 75 cm2 | ThermoFisher Scientific | 156499 | |
| Chamber Slide System, 4-well | ThermoFisher Scientific | 154526 | |
| Dulbecco’s Modified Eagle’s Medium (DMEM), high glucose (4.5 g/L), L-glutamine (2 mM) | Corning | 10-017-CV | Stored at 4 °C |
| Falcon conical centrifuge tubes, 15 mL | Fisher Scientific | 14-959-53A | |
| Falcon permeable support for 24-well plate with 0.4 µM transparent PET membrane | Corning | 353095 | |
| Fetal bovine serum | Fisher Scientific | W3381E | Stored in 50 mL aliquots at -20 °C |
| Gelatin solution, 0.1% | ATCC | PCS-999-027 | Stored at 4 °C |
| Graduated and sterile pipette tips, 10 µL | USA Scientific | 1111-3810 | |
| Leukemia inhibitory factor (LIF), 106 unit/mL | Millipore Sigma | ESG1106 | |
| L-glutamine 200 mM (100x) | Gibco | 25030-081 | |
| Lipofectamine RNAiMAX | Thermo Fisher Scientific | 13778-075 | |
| MEM non-essential amino acids (MEM NEAA) 100x | Gibco | 11140-050 | |
| Minimum essential medium (MEM) | Corning | 10-022-CV | |
| Mitomycin C | Roche | 10107409001 | |
| Non-stick auto-glass coverslips, 24 x 55 mm | Springside Scientific | HRTCG2455 | |
| O9-1 neural crest cell line | Millipore Sigma | SCC049 | |
| Opti-MEM I, 1x | Gibco | 31985-070 | |
| Paraformaldehyde solution in PBS, 4% | Santa Cruz Biotechnology | sc-281692 | Stored at 4 °C |
| Penicillin-streptomycin (10,000 U/mL penicillin and 10,000 μg/mL streptomycin) | Fisher Scientific | W3470H | Stored in 10 mL aliquots at -20 °C |
| Phalloidin-iFluor 488 | Abcam | ab176753 | Stored at -20 °C, Keep out of light |
| Phosphate-buffer saline (PBS), 1x, without calcium and magnesium, pH 7.4 | Corning | 21-040-CV | Stored at 4 °C |
| Recombinant human fibroblast growth factor-basic (rhFGF-basic) | R&D Systems | 233-FB-025 | |
| Recombinant human/mouse Wnt5a protein | R&D Systems | 645-WN-010 | |
| Sodium pyruvate, 100 mM | Gibco | 11360-070 | |
| Square Petri dish with grid | Thomas Scientific | 1219C98 | |
| STO murine fibroblast feeder cells | ATCC | CRL-1503 | |
| Triton X-100 solution | Sigma Aldrich | X100-100ML | |
| Trypsin-EDTA, 0.25% | Fisher Scientific | W3513C | Stored at 4 °C |
| Zeiss Apotome.2 fluoresence microscope | Carl Zeiss AG | ||
| Zeiss inverted Axio Vert.A1 light microscope | Carl Zeiss AG | ||
| Zen lite 2012 microscopy software | Carl Zeiss AG | imaging software |
Referências
- Ho, H. Y. H., et al. Wnt5a-Ror-Dishevelled signaling constitutes a core developmental pathway that controls tissue morphogenesis. Proceedings of the National Academy of Sciences of the United States of America. 109 (11), 4044-4051 (2012).
- Čapek, D., et al. Light-activated Frizzled7 reveals a permissive role of noncanonical wnt signaling in mesendoderm cell migration. Elife. (8), 42093 (2019).
- Li, D., et al. Planar cell polarity signaling regulates polarized second heart field morphogenesis to promote both arterial and venous pole septation. Development. 146 (20), 181719 (2019).
- Lutze, G., et al. Noncanonical WNT-signaling controls differentiation of lymphatics and extension lymphangiogenesis via RAC and JNK signaling. Scientific Reports. 9 (1), 4739 (2019).
- Buttler, K., et al. Maldevelopment of dermal lymphatics in Wnt5a-knockout-mice. Biologia do Desenvolvimento. 381 (2), 365-376 (2013).
- Betterman, K. L., et al. Atypical cadherin FAT4 orchestrates lymphatic endothelial cell polarity in response to flow. Journal of Clinical Investigation. 130 (6), 3315-3328 (2020).
- Descamps, B., et al. Frizzled 4 regulates arterial network organization through noncanonical Wnt/planar cell polarity signaling. Circulation Research. 110 (1), 47-58 (2012).
- Weeraratna, A. T., et al. Wnt5a signaling directly affects cell motility and invasion of metastatic melanoma. Cancer Cell. 1 (3), 279-288 (2002).
- Henry, C., et al. Expression of the novel Wnt receptor ROR2 is increased in breast cancer and may regulate both β-catenin dependent and independent Wnt signalling. Journal of Cancer Research and Clinical Oncology. 141 (2), 243-254 (2014).
- Anastas, J. N., et al. A protein complex of SCRIB, NOS1AP and VANGL1 regulates cell polarity and migration, and is associated with breast cancer progression. Oncogene. 31 (32), 3696-3708 (2012).
- Niehrs, C. The complex world of WNT receptor signalling. Nature Reviews Molecular Cell Biology. 13 (12), 767-779 (2012).
- Dong, B., et al. Functional redundancy of frizzled 3 and frizzled 6 in planar cell polarity control of mouse hair follicles. Development. 145 (19), (2018).
- Bernascone, I., et al. Sfrp3 modulates stromal-epithelial crosstalk during mammary gland development by regulating Wnt levels. Nature Communications. 10 (1), 2481 (2019).
- Hendrickx, G., et al. WNT16 requires Gα subunits as intracellular partners for both its canonical and noncanonical WNT signalling activity in osteoblasts. Calcified Tissue International. 106 (3), 294-302 (2020).
- Avgustinova, A., et al. Tumour cell-derived Wnt7a recruits and activates fibroblasts to promote tumour aggressiveness. Nature Communications. (7), 10305 (2016).
- Tseng, J. C., et al. CAPE suppresses migration and invasion of prostate cancer cells via activation of noncanonical Wnt signaling. Oncotarget. 7 (25), 38010-38024 (2016).
- Wang, Q., et al. A novel role for Wnt/Ca2+ signaling in actin cytoskeleton remodeling and cell motility in prostate cancer. PLoS One. 5 (5), 10456 (2010).
- Gibbs, B. C., et al. Prickle1 mutation causes planar cell polarity and directional cell migration defects associated with cardiac outflow tract anomalies and other structural birth defects. Biology Open. 5 (3), 323-335 (2016).
- Cui, C., et al. a PCP protein required for ciliogenesis, regulates directional cell migration and cell polarity by direct modulation of the actin cytoskeleton. PLoS Biology. 11 (11), 1001720 (2013).
- Gombos, R., et al. The formin DAAM functions as molecular effector of the planar cell polarity pathway during axonal development in Drosophila. The Journal of Neuroscience. 35 (28), 10154-10167 (2015).
- Toubat, O., et al. Neural Crest Cell-derived Wnt5a Regulates Planar Cell Polarity in Cranial Second Heart Field Progenitor Cells. Circulation. 142, 12540 (2020).
- Li, D., et al. Spatial regulation of cell cohesion by Wnt5a during second heart field progenitor deployment. Biologia do Desenvolvimento. 412 (1), 18-31 (2016).
- Sinha, T., et al. Loss of Wnt5a disrupts second heart field cell deployment and may contribute to OFT malformations in DiGeorge syndrome. Human Molecular Genetics. 24 (6), 1704-1716 (2015).
- Humphries, A. C., et al. From instruction to output: Wnt/PCP signaling in development and cancer. Current Opinion in Cell Biology. (51), 110-116 (2018).
- Shi, D. L. Decoding Dishevelled-Mediated Wnt Signaling in Vertebrate Early Development. Frontiers in Cell and Developmental Biology. (8), 588370 (2020).
- Butler, M. T., et al. Planar cell polarity in development and disease. Nature Reviews Molecular Cell Biology. 18 (6), 375-388 (2017).
- Bradshaw, L., et al. Dual role for neural crest cells during outflow tract septation in the neural crest-deficient mutant Splotch2H. Journal of Anatomy. 214 (2), 245-257 (2009).
- Kodo, K., et al. Regulation of Sema3c and the interaction between cardiac neural crest and second heart field during outflow tract development. Scientific Reports. 7 (1), 6771 (2017).
- Waldo, K. L., et al. Cardiac neural crest is necessary for normal addition of the myocardium to the arterial pole from the secondary heart field. Biologia do Desenvolvimento. 281 (1), 66-77 (2005).
- Schleiffarth, J. R., et al. Wnt5a is required for cardiac outflow tract septation in mice. Pediatric Research. 61 (4), 386-391 (2007).
- Nguyen, B. H., et al. Culturing and Manipulation of O9-1 Neural Crest Cells. Journal of Visualized Experiments. (140), e58346 (2018).
- Suarez-Arnedo, A., et al. An image J plugin for the high throughput image analysis of in vitro scratch wound healing assays. PLoS One. 15 (7), 0232565 (2020).
- Martinotti, S., et al. Scratch wound healing assay. Methods in Molecular Biology. (2109), 225-229 (2020).

