Dual-Task Stroop Paradigm for Detecting Cognitive Deficits in High-Functioning Stroke Patients
Summary
Clinical assessment scales are notsensitive enough to cognitive dysfunction in high-functioning stroke patients. The dual-task paradigm presents advantages and potential in the assessment and cognitive training of cognitive dysfunction. The study here proposes a dual-task Stroop paradigm to identify cognitive dysfunction in high-functioning stroke patients.
Abstract
General clinical cognitive assessment scales are not sensitive enough to cognitive impairment in high-functioning stroke patients. The dual-task assessment has advantages for identifying cognitive deficits in high-functioning stroke patients and has been gradually applied in clinical assessment and cognitive training. Moreover, the Stroop paradigm has higher sensitivity and specificity for attentional assessment than conventional clinical cognitive assessment scales. Therefore, this study presents the dual-task assessment based on the Stroop paradigm to identify cognitive deficits in high-functioning stroke patients. This study demonstrates a single- and dual-task evaluation based on the Stroop paradigm and confirms its feasibility through case experiments and synchronized functional near-infrared spectroscopy evaluation. The Stroop reaction time and correct rate are used as the main indicators to evaluate the cognitive level of the subjects. This study protocol aims to provide new ideas to figure out the ceiling effect in general clinical assessment failure for high-functioning stroke patients.
Introduction
Stroke is the leading cause of disability in humans1 and can cause varying degrees of motor, cognitive, emotional, and other functional deficits2. Some stroke patients with better prognosis and only slight functional defects show greater functional autonomy in daily activities, but the functional state of their disability may not be sufficient to support their return to work or previous activities. These patients are referred to as high-functioning stroke patients3,4. Due to their minor functional deficits, it is hard to identify their dysfunctions, especially in terms of cognitive functions, through the general assessment of function scales, such as the Montreal cognitive assessment (MoCA)5 and clinical dementia rating (CDR)6, which have a ceiling effect and poor sensitivity for identifying mild functional defects in high-functioning stroke patients. Therefore, it is necessary to develop objective and simple methods to identify cognitive dysfunction in high-functioning stroke patients.
In recent years, the advantages of the dual-task paradigm in assessment and training have gradually become valued7,8. For example, patients may perform normally on simple cognitive single tasks (e.g., calculation) but show varying degrees of cognitive decline when additional tasks are added9,10 (e.g., walking while counting). Manaf et al. found that stroke patients often use compensatory strategies when performing cognitive-motor dual tasks, such as maintaining stability by sacrificing cognitive task performance11. Therefore, the dual-task assessment may have advantages in identifying cognitive deficits in patients with high-functioning stroke. On the one hand, the content of the dual-task assessment is closer to daily life than a single task, such as walking while observing the surrounding environment or talking and calling. In previous studies, the walking + naming task and walking + crossing obstacles task were designed to simulate walking in real environments12.
On the other hand, the executive ability in dual tasks has a close relationship with divided attention (belonging to the category of advanced cognitive function)13. Divided attention is the ability to handle multiple tasks simultaneously and allocate attention to two or more tasks14. This cognitive skill is of great significance to improve the efficiency of daily activities. Therefore, the results of the dual-task assessment can be used for reflecting the individual's divided attention. Normally, people can deal with two or more simple tasks simultaneously in their daily lives and are not disturbed. However, when brain function is impaired, there may be more dual-task interference when faced with simple dual tasks; that is, when performing dual tasks, the reduced divided attention may be likely to cause the performance of one or two tasks to be impaired15. It is concluded that dual-task execution is more likely to be able to detect advanced cognitive function impairment in patients with high-functioning stroke.
The Stroop paradigm is a classical experimental paradigm to study the Stroop effect (also known as the conflict effect)16, which has been widely used in attention assessment in cognitive function tests, especially in the field of attention inhibition17. The classical Stroop effect refers to the fact that it is difficult for individuals to respond quickly and accurately to non-dominant stimuli due to the interference of the dominant response. This results in a longer response time and lower response accuracy for non-dominant stimuli. The difference in reaction time or accuracy rate between dominant and non-dominant reactions is the Stroop effect18. Therefore, the Stroop requires high levels of attention19. Smaller Stroop effects represent higher attentional inhibition, while larger Stroop effects represent a decline in attentional inhibition18.
The Stroop paradigm may be more suitable for assessing cognitive dysfunction in patients with high-functioning stroke and has higher sensitivity and specificity for attention assessment than the traditional clinical assessment scale20. Therefore, this study designed a dual-task assessment based on the Stroop paradigm to identify cognitive deficits in high-functioning stroke patients. The protocol also includes clinical assessment of cognitive function, lower limb motor function, and balance function in stroke patients to ensure that patients can complete the dual-task assessment. Functional near-infrared spectroscopy (fNIRS) was used as an objective evaluation tool for brain function to detect the activation of brain function in high-functioning stroke patients under the dual task. The effectiveness and feasibility of the dual-task assessment scheme based on the Stroop paradigm were verified from the perspective of neuroimaging, which provides new aspects for clinical practice.
Protocol
This project was approved by the Medical Ethics Association of the Fifth Affiliated Hospital of Guangzhou Medical University (No. KY01-2020-08-06) and has been registered at the China Clinical Trial Registration Center (No. ChiCTR2000036514). Informed consent was obtained from patients for using their data in this study.
1. Recruitment
- Recruit stroke patients with stable conditions as confirmed by imaging examination-diagnosis conforms to the diagnostic criteria of cerebrovascular disease of the Chinese Medical Association Neurology Branch (2005). Choose patients with stroke at Brunnstrom stage IV21.
- Ensure the patients can complete basic daily activities independently. Ensure the patients are without obvious cognitive impairment and meet the following requirements: MoCA in the normal range; no unilateral neglect (Albert's Test, number of omissions ≤2)22; no other neurological diseases, such as language defects; and can cooperate with relevant instructions to complete this study.
- Ensure the subjects participate in the test voluntarily and sign an informed consent form.
2. Clinical evaluation
- Record the subject's information, including name, gender, date of birth, education level, body mass index, medical history, and medication history.
- Perform cognitive function assessment.
- Perform MoCA23 on stroke patients by asking 11 questions addressing subjects' attention and concentration, executive function, memory, language, visual structure skills, abstract thinking, computing, and orientation.
- The total score of the MoCA is 30, which is related to education level. If the subject took less than 12 years of education, add one point to the total score of MoCA. Consider a score of 26 and higher as normal23.
- Perform a CDR24 on the stroke patients. Collect information during structured interviews with stroke patients and their families and assess the subjects' abilities in six aspects: memory, orientation, judgment and problem solving, work and social interaction, family life and personal hobby, and independent living.
- The highest possible score is 3. Assess the scores obtained as follows: total score = 0 indicates no dementia; total score = 0.5 indicates suspected dementia; total score = 1 indicates mild cognitive impairment; total score = 2 indicates moderate cognitive impairment; and total score = 3 indicates severe cognitive impairment24.
- Perform the Albert's test to detect the presence of unilateral spatial neglect (USN) in patients with stroke. Ask the subject to cross out all the lines that are placed in random orientations on a piece of paper.
- Present the subject with a series of 40 black lines, each about 2 cm long, randomly oriented on a sheet of white 11 in x 8.6 in size paper in six rows. Assess the presence or absence of USN, based on the number of lines left uncrossed on each side of the test sheet. If any lines are left uncrossed and more than 70% of these uncrossed lines are on the same side as the motor deficit, this indicates unilateral spatial neglect.
- Perform motor function assessment.
- Perform the Fugl-Meyer Assessment (FMA) on the stroke patients to assess motor function, sensation, balance, joint range of motion, and joint pain in patients with post-stroke hemiplegia. The motor domain includes items assessing movement, coordination, and the reflex actions of the shoulder, elbow, forearm, wrist, hand, hip, knee, and ankle.
- The motor function score ranges from 0 (hemiplegia) to 100 points (normal motor performance), divided into 66 points for the upper extremities and 34 points for the lower extremities. Assess the score as follows: 0-49 points indicate severe motor impairment; 50-84 points indicate marked motor impairment; 85-95 points indicate moderate motor impairment; and 96-99 points indicate slight motor impairment.
- Perform balance function assessment.
- Perform the Berg balance scale (BBS)27 on the stroke patient, with a total of 14 items from easy to difficult, including sitting balance, standing balance, body transfer, turning, and single-leg standing.
- Asses the scores as follows: the highest score on the scale is 56; a total score of <40 points suggests a risk of falling; 0-20 points scored indicates poor balance function and that a wheelchair is required; 21-40 points scored suggests that the subject has a certain balance function and needs to walk with assistance; 41-56 points scored suggests good balance function and that the subject can walk independently28.
- Perform risk of falling assessment.
- Perform the timed up and go test (TUGT)29 on stroke patients. Ask the subject to stand up from the chair, walk for 3 m, turn their body, then return and sit in the chair at a comfortable speed to ensure safety. Concurrently, ask the evaluator to time the whole process from issuing the departure order to sitting in the chair.
- Assess the result obtained as follows: if the total time for the subject to complete TUGT ≥14 s, it indicates that the subject has the risk of falling29.
3. Stroop task evaluations
- Perform the Stroop single task evaluation (Stroop task only; Figure 1).
- Ask the patient to sit in a stable chair.
- Run the commercial stimulus presentation software and select the congruence test trials. Make a new profile for the patient. Select the congruence test trials of the Stroop task and repeat three trials.
- Carry out the following experimental paradigm. Design the experiment with a patient rest time of 10 s and then ask the patient to perform one cognitive test with a frequency of 6 s for a total of three trials, with each trial having a 60 s stimulus + 60 s rest.
- Set the total duration of the experiment to 370 s (the specific process is shown in Figure 1). In the resting stage, ask the patient to relax. When the experiment is in the stimulation stage, ask the patient to perform the attention-related test, complete the task in 6 s, and complete it 10x in 60 s.
- Ask the patients to follow the instructions for the two test trials as described below.
- Select the congruence test trials. Click the arrow button to the left (←) as soon as possible when
 is shown on the left of the square. Click the arrow button to the right (→) as soon as possible when
is shown on the left of the square. Click the arrow button to the right (→) as soon as possible when  is shown on the right of the square.
is shown on the right of the square. - Select the incongruence test trials, which share the same step as the congruence test trials. Click the arrow button to the left (←) as soon as possible when
 is shown on the left of the square, ignoring the meaning of the character and focusing on its position.
is shown on the left of the square, ignoring the meaning of the character and focusing on its position. - Click the arrow button to the right (→) as soon as possible, when
 is shown on the right of the square, ignoring the meaning of the character and focusing on its position. Finish the task, save the data, and export the data to a self-built database.
is shown on the right of the square, ignoring the meaning of the character and focusing on its position. Finish the task, save the data, and export the data to a self-built database.
- Select the congruence test trials. Click the arrow button to the left (←) as soon as possible when
- Perform the Stroop dual-task evaluation (Stroop task + balance control).
- Ask the patient to sit on a balance ball with the therapist being responsible for the patient's protection. Let the patient complete the Stroop experimental paradigm with the steps mentioned above (steps 3.1.1.-3.1.5.).
- When the experiment is in a resting stage, ask the patient to keep balance and relax on the balance ball as much as possible. When the experiment is in the state of stimulation, ask the patient to carry out the attention-related test while maintaining balance on the balance ball as much as possible.
- Ask the patient to sit on a balance ball with the therapist being responsible for the patient's protection. Let the patient complete the Stroop experimental paradigm with the steps mentioned above (steps 3.1.1.-3.1.5.).
4. fNIRS evaluation
- Place 10 light sources and 12 receivers on the fNIRS test cap to correspond to this study's four regions of interest (ROIs), which include the left prefrontal cortex (LPFC), right prefrontal cortex (RPFC), left promoter cortex (LPMC), and right promoter cortex (RPMC).
- Preparation of the subject
- Inform the subjects of the experimental purpose and observe the patients.
- Ensure the Cz site at the top of the test cap, the fourth point from the forehead to the occipital lobe on the midline of the full cap. Ensure the midpoint of the connection lies between the nasal root to the lower edge of the occipital protuberance, the intersection point of the connection from the nasal root to the occipital protuberance, or the connection between the superior auricular fossa of both ears (cymba conchae).
- Place the cap on the subject's head and adjust the position of the cap so that the Cz point on the subject's head coincides with the Cz point on the cap. Tighten the tie on both sides of the cap and allow the subject's ears to pierce through the gap; the front of the cap is naturally attached to the forehead, and the back is naturally attached to the occiput.
- Acquisition and pre-acquisition
- Open the software, select the experimental subject, and input the patients' basic information. Set the sampling frequency to 11 Hz.
- Click the Pre-acquisition button to start pre-acquisition and calibrate the test signal. According to the signal intensity of each point displayed by the functional near-infrared spectroscopy, adjust the weak signal points by moving the cap or further exposing the scalp. When the signal intensity of each point collected by the cap tends to be stable, stop pre-collection, and click the automatic gain button. Click the Start button to collect the signal.
NOTE: Ensure the signal quality in acquisition and pre-acquisition as follows. The original light intensity signal curve should be stable, accompanied by a 1-2 Hz heartbeat signal fluctuation, and the value should meet the reasonable threshold set by the equipment. The intensity of the signal can be indicated by color, where a gray display signal intensity is low, yellow is good, green is excellent, and red is too strong.
- Perform Stroop single task evaluation synchronized with fNIRS. Then, perform Stroop dual-task evaluation synchronized with fNIRS.
5. Data processing and analysis
- Process general information and clinical evaluation data of the patients.
- Analyze the near-infrared data using the NirSpark software package in MATLAB.
- Perform data pre-procession.
- Click the Exclude button to eliminate the time interval unrelated to the experiment. Click the Motion button to eliminate motion artifacts caused by physiological activities like breathing, heartbeat, pulse, etc., and involuntary activities like blinking, swallowing, etc., and convert the light intensity signal to an optical density signal.
- Click the Filter button to select the bandpass filter (0.01-0.2 Hz) to remove physiological and instrumental noise. Click the Hemo button to calculate the relative changes of oxyhemoglobin (HbO2) and deoxyhemoglobin (HbR) according to the modified Beer-Lambert Law and convert the optical density signal into the blood oxygen concentration signal.
NOTE: HbO2 is more sensitive to changes between conditions than HbR, so subsequent analysis uses only HbO2 data in this study protocol.
- General linear model (GLM) building
- Choose HbO2 in Hemo Type as the analysis data. Click the Specification button to take seconds as the time unit and select the standard HRF type as the basis function. Then, eliminate the rest stage to establish the GLM design matrix and select the stimulus stage in the task according to the experimental design.
- Click the Estimation button to fit the established design matrix with the collected data. Click the View button to check out the calculated β value.
NOTE: GLM is a linear combination of observed hemodynamic signals (dependent variable) as interesting regressions (task variable), redundant covariates (such as surface noise measured in short-range channels), and error terms.
- Calculate the β value as follows. Calculate experimental data in the ROIs by using the established linear correlation model. Obtain the GLM parameters of the required channel and derive the β value of brain activation under each experimental condition (that is, the weight coefficient in the linear model) for analysis.
- Perform data pre-procession.
- Run the commercial stimulus presentation software to export the performance data of cognitive tasks in the Stroop task and obtain the accuracy (ACC) and reaction time (RT) for final data analysis.
Representative Results
This study presents results from a high-functioning stroke patient, who was a 71-year-old male who suffered from ischemic stroke with left hemiplegia 2 years ago. The magnetic resonance imaging (MRI) presented bilateral chronic infarction from the basal ganglia to the radiating crown. He was able to walk and live independently in the community but was not satisfied with his cognitive recovery. However, the functional assessments were all within the normal range: FMA = 100, BBS = 56/56, TUGT = 6, MoCA = 26/30, CDR = 0.5, Albert's Test = 0. Moreover, we also recruited one young female healthy subject as the control. The subjects' information is shown in Table 1.
The single/dual-task assessment results based on the Stroop paradigm showed that, in high-functioning stroke patient performing the single-task Stroop test, the RT of the congruence test trials was shorter than that of the incongruence test trials, and the ACC was comparable to the incongruence test trials (RTCongruence = 547.62 ms, RTIncongruence = 565.07 ms; ACCCongruence = ACCIncongruence = 100%). When performing dual-task congruence test trials, the RT of high-functioning stroke patients was higher than that of healthy young subjects, and their ACC was also relatively lower (RTstroke = 587.03 ms, RThealth = 363.07 ms; ACCstroke = 93.33%, ACChealth = 100%), and the difference in the incongruence test trials was greater than that in the congruence test trials (RTstroke = 613.03 ms, RThealth= 384.67 ms; ACCstroke = 90%, ACChealth = 100%; Table 2).
The results for brain function showed that the β value of ROIs in the stroke patient was lower than that in the healthy young subject during the process of performing dual tasks (RDLPFC: βstroke = −0.006, βhealth = 0.1366; LDPFC: βstroke = −0.0196, βhealth = 0.0976). The rest of the brain regions are shown in Figure 2 and Figure 3.
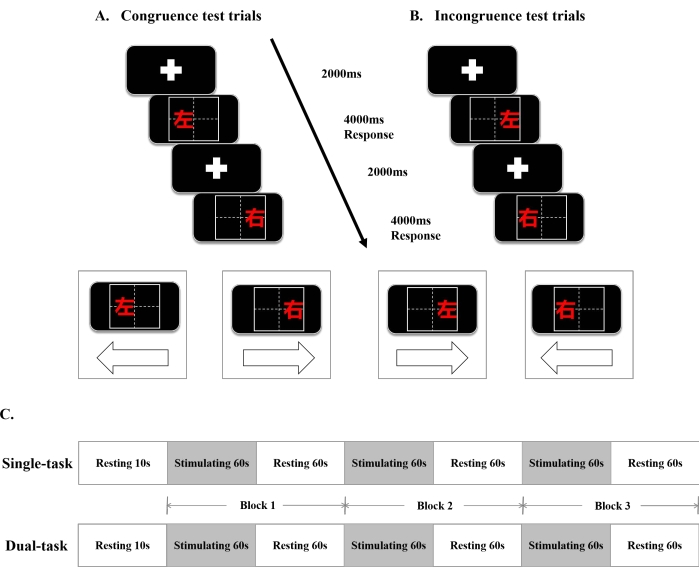
Figure 1: The single/dual-task Stroop paradigm and the fNIRS design. (A) Congruence test trials. (B) Incongruence test trials. (C) The timeline diagram of the single/dual-task Stroop paradigm. Abbreviations:ms = millisecond; s = second;  = left;
= left;  = right. Please click here to view a larger version of this figure.
= right. Please click here to view a larger version of this figure.
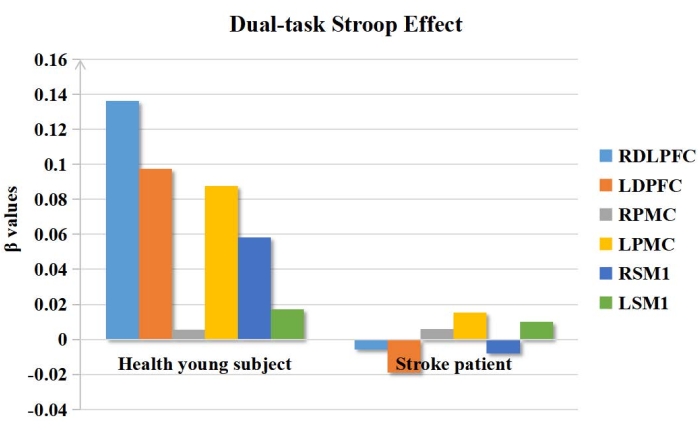
Figure 2: The β values in ROIs of the dual-task Stroop effect. The β values of ROIs in the stroke patient was lower than that of the healthy young subject during the dual-task Stroop. Abbreviations: ROIs = regions of interest; RDLPFC = right dorsolateral prefrontal cortex; LDPFC = left dorsolateral prefrontal cortex; RPMC = right promoter cortex; LPMC = left promotor cortex; RSM1 = right primary sensory-motor cortex 1; RPMC = right primary sensory-motor cortex. Please click here to view a larger version of this figure.
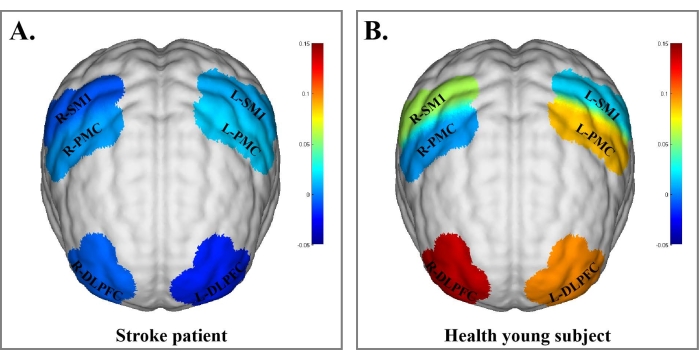
Figure 3: Blood oxygen concentration in brain regions of the stroke patient and healthy young subject under the dual-task Stroop effect. (A) Blood oxygen concentration in brain regions of the stroke patient under the dual-task Stroop effect. (B) Blood oxygen concentration in brain regions of the healthy young subject under the dual-task Stroop effect. The β values are indicated by color bars. The results of brain function showed that the β value of ROIs in the stroke patient was lower than that in the healthy young subject during dual-task performance. Abbreviations: R-DLPFC = right dorsolateral prefrontal cortex; L-DLPFC = left dorsolateral prefrontal cortex; R-PMC = right promoter cortex; L-PMC = left promotor cortex; R-SMI = right primary sensory-motor cortex; R-PMC = right primary sensory-motor cortex. Please click here to view a larger version of this figure.
| Characteristics | Healthy young subject | Stroke patient |
| Age (year) | 21 | 71 |
| Gender | female | male |
| BMI (kg/m2) | 22.27 | 23.81 |
| Cognitive assessment | ||
| Montreal Cognitive Assessment (MoCA) | 30/30 | 26/30 |
| Clinical Dementia Rating (CDR) | 0 | 0.5 |
| Albert’s Test | 0 | 0 |
| Motor and balance assessment | ||
| Brunnstrom stage | NT | V stage |
| Fugl-Meyer Assessment (FMA) | 100 | 100 |
| Berg Balance Scale (BBS) | 56/56 | 52/56 |
| Timed Up and Go Test (TUGT) (s) | 6 | 11 |
| Abbreviations: BMI, Body Mass Index; kg/m2, kilogram per square meter; NT, Not testable; s, second. | ||
Table 1: The baseline information and characteristics of the healthy young subject and the stroke patient.
| Congruence test trials | Incongruence test trials | |||
| ACC | RT(ms) | ACC | RT(ms) | |
| the stroke patient | 93.33% | 587.03 | 90% | 613.03 |
| the healthy young subject | 100% | 363.07 | 100% | 384.67 |
| Abbreviations: ACC, accuracy; RT, reaction time; ms, millisecond. | ||||
Table 2: The ACC and RT of the healthy young subject and the stroke patient in the dual task. Abbreviations: ACC = accuracy; RT = reaction time; ms = millisecond.
Discussion
In our study, the results of the routine clinical cognitive assessment scales for the high-functioning stroke patient did not show any significant cognitive deficits. However, these assessment scales might show a ceiling effect and be less sensitive for identifying the mild cognitive deficits of high-functioning stroke patients. Hence, this protocol further selected ACC and RT in dual-task assessment based on the Stroop paradigm as major indicators to identify the cognitive deficits of high-functioning stroke patients. The results showed that, when the high-functioning stroke patient performed the dual-task Stroop paradigm, their RT was significantly longer than that of the healthy young subject, the ACC was also relatively lower, and the difference in the incongruence test trials was greater than that in the congruence test trials. Besides, the study also used fNIRS to detect the subjects' extent of brain activation in cognitive regions during the execution of the single/dual task in real-time so as to verify the feasibility of the scheme. The data show that the β value of ROIs of the high-functioning stroke patient was lower than that of the healthy subject.
This study protocol designed the Stroop paradigm combined with motion control and the motor functional assessment scale modules of the routine clinical scales, including the FMA, BBS, and TUGT. Among them, the FMA was used to assess subjects' lower limb motor function, BBS was used to assess balance function, and TUGT was used to assess the risk of falling. The assessment results were all within the normal range of motor function. The assessment results of the routine clinical scales showed that the stroke patient included in the study was a high-functioning stroke patient. On the other hand, it also ensured that the included subject was capable of completing the motor task in the experiment. In addition, the cognitive functioning assessment scale modules of the routine clinical scales included the MoCA, CDR, and Albert's Test. Among them, the MoCA and CDR were used to assess the level of cognition, and Albert's Test was used to assess whether the subject suffered from unilateral spatial neglect. Considering that the clinical cognitive functioning assessment scales are semi-quantitative and have a ceiling effect and that there is a lack of sensitivity in the assessment of patients with mild cognitive dysfunction, which causes certain limitations in the evaluation of clinical scales for high-functioning stroke patients, a superior approach needs to be found to solve this problem. Moreover, the study protocol used the ACC and RT of the Stroop paradigm as objective indicators to improve the sensitivity of the assessment results.
According to the representative results, when the high-functioning stroke patient performed the single-task Stroop paradigm, the RT of the congruence test trials was shorter than that of the incongruence test trials, and the ACC was comparable between the two test trials. During the single-task paradigm, the high-functioning stroke patient was able to complete the Stroop test well, showing no obvious cognitive deficits. However, when the high-functioning stroke patient performed the dual-task Stroop paradigm, the RT was significantly higher than that of the healthy young subject, and the ACC of the high-functioning stroke patient was lower. Moreover, the difference in the incongruence test trial was more significant than in the congruence test trial. During the dual-task paradigm, the high-functioning stroke patient had a weakened ability to perform both tasks simultaneously due to his potential cognitive deficits. The patient often uses compensatory strategies (i.e., to maintain stability by sacrificing cognitive task performance), which exposes the cognitive deficits in terms of relatively poor task performance. In the incongruence test trials, the difficulty of the cognitive tasks increased, which made the difference in performance between the high-functioning stroke patient and the healthy young subject more significant and more easily exposed the cognitive deficits of the high-functioning stroke patient. Therefore, this study proposes a dual-task assessment approach based on the Stroop paradigm to identify cognitive deficits in high-functioning stroke patients.
In addition, the study also used the fNIRS technique to verify the feasibility of this protocol. In a case study, fNIRS was used to monitor the subjects' brain activation in cognitive regions in real-time during single/dual-task periods, and six ROIs from cognitive areas were selected to calculate the β value30. The results of the case study showed that the β value of ROIs in the stroke patient was lower than that in the healthy subject. In the process of performing the dual task, the healthy subject used brain resources to complete the cognitive task and motor task simultaneously through activating more brain regions; when the high-functioning stroke patient performed the dual task, sufficient brain areas were not active because of partial damage to brain function. Therefore, enough brain resources were not generated to meet the requirements of performing the cognitive and motor tasks at the same time, which made the performance lower than that of the healthy subject. According to the results of fNIRS monitoring, the degree of brain activation in the high-functioning stroke patient was indeed less than that in the healthy subject, which confirmed the feasibility of using the dual-task Stroop paradigm to identify cognitive deficits in high-functioning stroke patients.
Although the number of included subjects is limited in this study, an earlier case study by Zlatko Matjačić et al.31 proved that disturbance balance training using a robot may be a feasible method, and this finding illustrates the effectiveness of the case study shown here. Moreover, this study displays the whole process of the experimental design and demonstrates the feasibility of this protocol with the help of the results of a case study. Before the trial, subjects should understand the rules and perform the processes of the Stroop test sufficiently. Additionally, one to two pretests should be performed by subjects before the formal experiment to make smooth progress and improve the accuracy of the data. Besides, the safety of the high-functioning stroke patient needs to be ensured all the time on the balance ball during the dual-task Stroop paradigm, so one must ensure that there is a professional staff member in charge of the subjects' safety.
This protocol has some limitations. First, this study aims to demonstrate a dual-task assessment method that can identify cognitive deficits in high-functioning stroke patients. The representative results present only one subject's assessment results. Second, this protocol only takes the balance-cognitive task as the dual-task paradigm and fails to show a variety of dual-task assessment schemes. Future studies will be needed to supplement this.
This study proposes the dual-task Stroop paradigm, which could be used to identify cognitive deficits in high-functioning stroke patients.
Declarações
The authors have nothing to disclose.
Acknowledgements
This study was supported by grants from the National Natural Science Foundation of China (No. 81804004, 81902281), China Postdoctoral Science Foundation (No. 2018M643207), Shenzhen Municipal Health Commission Project (No. SZBC2018005), Shenzhen Science and Technology Project (No. JCYJ20160428174825490), the General Guidance Program of Guangzhou Municipal Health and Family Planning (No. 20211A010079, 20211A011106), Guangzhou and University Foundation (No. 202102010100), Guangzhou Medical University Foundation (No. PX-66221494), Key Laboratory of Guangdong Higher Education Institutes [Grant Number: 2021KSYS009] and Guangdong Province Department of Education [Grant Number: 2021ZDZX2063].
Materials
| Balance Ball | Shanghai Fanglian Industrial Co, China | PVC-KXZ-EVA01-2015 | NA |
| E-Prime 3.0 | Psychology softwares Tools | commercial stimulus presentation software | |
| fNIRS | Hui Chuang, China | NirSmart-500 | NA |
Referências
- Dichgans, M., Pulit, S. L., Rosand, J. Stroke genetics: Discovery, biology, and clinical applications. The Lancet. Neurology. 18 (6), 587-599 (2019).
- Chen, G., Leak, R. K., Sun, Q., Zhang, J. H., Chen, J. Neurobiology of stroke: Research progress and perspectives. Progress In Neurobiology. 163-164, 1-4 (2018).
- Maratos, M., Huynh, L., Tan, J., Lui, J., Jarus, T. Picture this: Exploring the lived experience of high-functioning stroke survivors using photovoice. Qualitative Health Research. 26 (8), 1055-1066 (2016).
- Platz, T., Prass, K., Denzler, P., Bock, S., Mauritz, K. H. Testing a motor performance series and a kinematic motion analysis as measures of performance in high-functioning stroke patients: reliability, validity, and responsiveness to therapeutic intervention. Archives of Physical Medicine and Rehabilitation. 80 (3), 270-277 (1999).
- Trzepacz, P. T., Hochstetler, H., Wang, S., Walker, B., Saykin, A. J. Relationship between the Montreal Cognitive Assessment and Mini-mental State Examination for assessment of mild cognitive impairment in older adults. BMC Geriatrics. 15, 107 (2015).
- McDougall, F., et al. Psychometric properties of the Clinical Dementia Rating – Sum of boxes and other cognitive and functional outcomes in a prodromal Alzheimer’s disease population. The Journal of Prevention of Alzheimer’s Disease. 8 (2), 151-160 (2021).
- McHorney, C. A., Tarlov, A. R. Individual-patient monitoring in clinical practice: Are available health status surveys adequate. Quality of Life Research. 4 (4), 293-307 (1995).
- Silsupadol, P., et al. Effects of single-task versus dual-task training on balance performance in older adults: a double-blind, randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 90 (3), 381-387 (2009).
- Feld, J. A., et al. Relationship between dual-task gait speed and walking activity poststroke. Stroke. 49 (5), 1296-1298 (2018).
- Liu, Y. -. C., Yang, Y. -. R., Tsai, Y. -. A., Wang, R. -. Y. Cognitive and motor dual task gait training improve dual task gait performance after stroke – A randomized controlled pilot trial. Scientific Reports. 7 (1), 4070 (2017).
- Manaf, H., Justine, M., Ting, G. H., Latiff, L. A. Comparison of gait parameters across three attentional loading conditions during timed up and go test in stroke survivors. Topics In Stroke Rehabilitation. 21 (2), 128-136 (2014).
- Ou, H., et al. Motor dual-tasks for gait analysis and evaluation in post-stroke patients. Journal of Visualized Experiments. (169), e62302 (2021).
- Hirano, D., Goto, Y., Jinnai, D., Taniguchi, T. Effects of a dual task and different levels of divided attention on motor-related cortical potential. Journal of Physical Therapy Science. 32 (11), 710-716 (2020).
- Loetscher, T., Potter, K. -. J., Wong, D., das Nair, R. Cognitive rehabilitation for attention deficits following stroke. The Cochrane Database of Systematic Reviews. 2019 (11), (2019).
- Chen, C., Leys, D., Esquenazi, A. The interaction between neuropsychological and motor deficits in patients after stroke. Neurology. 80, 27-34 (2013).
- Puglisi, G., et al. Frontal pathways in cognitive control: Direct evidence from intraoperative stimulation and diffusion tractography. Brain. 142 (8), 2451-2465 (2019).
- MacLeod, C. M. Half a century of research on the Stroop effect: An integrative review. Psychological Bulletin. 109 (2), 163-203 (1991).
- Su, M., Wang, R., Dong, Z., Zhao, D., Yu, S. Decline in attentional inhibition among migraine patients: An event-related potential study using the Stroop task. The Journal of Headache and Pain. 22 (1), 34 (2021).
- Tsang, C. S. L., Chong, D. Y. K., Pang, M. Y. C. Cognitive-motor interference in walking after stroke: test-retest reliability and validity of dual-task walking assessments. Clinical Rehabilitation. 33 (6), 1066-1078 (2019).
- Bai, Q., Hu, J., Zhang, L. J., Chen, Y., Zhang, Y. H., Wang, X. C., Chi, L. Y. Application value of Stroop test in the evaluation of cognitive function in asymptomatic cerebral infarction. China Journal of Alzheimer’s Disease and Related Disorders. 4 (4), 269-274 (2021).
- Pandian, S., Arya, K. N. Stroke-related motor outcome measures: Do they quantify the neurophysiological aspects of upper extremity recovery. Journal of Bodywork and Movement Therapies. 18 (3), 412-423 (2014).
- Albert, M. L. A simple test of visual neglect. Neurology. 23 (6), 658-664 (1973).
- Nasreddine, Z. S., et al. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society. 53 (4), 695-699 (2005).
- Morris, J. C. The Clinical Dementia Rating (CDR): Current version and scoring rules. Neurology. 43 (11), 2412-2414 (1993).
- Sullivan, K. J., et al. Fugl-Meyer assessment of sensorimotor function after stroke: Standardized training procedure for clinical practice and clinical trials. Stroke. 42 (2), 427-432 (2011).
- Sanford, J., Moreland, J., Swanson, L. R., Stratford, P. W., Gowland, C. Reliability of the Fugl-Meyer assessment for testing motor performance in patients following stroke. Physical Therapy. 73 (7), 447-454 (1993).
- Downs, S. The Berg Balance Scale. Journal of Physiotherapy. 61 (1), 46 (2015).
- Blum, L., Korner-Bitensky, N. Usefulness of the Berg Balance Scale in stroke rehabilitation: A systematic review. Physical Therapy. 88 (5), 559-566 (2008).
- El Said, S. M. S., Adly, N. N., Abdul-Rahman, S. A. Executive function and physical function among community-dwelling Egyptian older adults. Journal of Alzheimer’s Disease. 80 (4), 1583-1589 (2021).
- Al-Yahya, E., et al. Prefrontal cortex activation while walking under dual-task conditions in stroke: A multimodal imaging study. Neurorehabilitation and Neural Repair. 30 (6), 591-599 (2016).
- Matjacic, Z., Zadravec, M., Olensek, A. Feasibility of robot-based perturbed-balance training during treadmill walking in a high-functioning chronic stroke subject: A case-control study. Journal of Neuroengineering and Rehabilitation. 15 (1), 32 (2018).

