Tuina Intervention in Sodium Monoiodoacetate Injection-Induced Rat Model of Knee Osteoarthritis
Summary
This protocol describes the methods of Tuina intervention in sodium monoiodoacetate injection-induced rat model of knee osteoarthritis (KOA), which provides a reference for the application of Tuina in KOA animal models. This protocol also studies the effective mechanism of Tuina for KOA, and the results will help promote its application.
Abstract
Knee osteoarthritis (KOA), a common degenerative joint disorder, is characterized by chronic pain and disability, which can progress to irreparable structural damage of the joint. Investigations into the link between articular cartilage, muscles, synovium, and other tissues surrounding the knee joint in KOA are of great importance. Currently, managing KOA includes lifestyle modifications, exercise, medication, and surgical interventions; however, the elucidation of the intricate mechanisms underlying KOA-related pain is still lacking. Consequently, KOA pain remains a key clinical challenge and a therapeutic priority. Tuina has been found to have a regulatory effect on the motor, immune, and endocrine systems, prompting the exploration of whether Tuina could alleviate KOA symptoms, caused by the upregulation of inflammatory factors, and further, if the inflammatory factors in skeletal muscle can augment the progression of KOA.
We randomized 32 male Sprague Dawley (SD) rats (180-220 g) into four groups of eight animals each: antiPD-L1+Tuina (group A), model (group B), Tuina (group C), and sham surgery (group D). For groups A, B, and C, we injected 25 µL of sodium monoiodoacetate (MIA) solution (4 mg MIA diluted in 25 µL of sterile saline solution) into the right knee joint cavity, and for group D, the same amount of sterile physiological saline was injected. All the groups were evaluated using the least to most stressful tests (paw mechanical withdrawal threshold, paw withdrawal thermal latency, swelling of the right knee joint, Lequesne MG score, skin temperature) before injection and 2, 9, and 16 days after injection.
Introduction
Knee osteoarthritis (KOA) is a common degenerative osteoarthritis, characterized by chronic pain and disability, and relatively severe KOA will lead to irreversible structural damage to the joint1. The high global prevalence of KOA has become a major global public health challenge2,3, which seriously impairs the quality of life of patients4,5. Studies have shown that KOA affects more than 260 million people worldwide6. With the aging of the population, the total prevalence rate of KOA in China is as high as 17.0% over the age of 40, which puts a heavy burden on the families of those affected7,8.
According to Chinese medicine, KOA belongs to the category of "paralysis"9, and the Yellow Emperor's Classic of Internal Medicine associates tendons, bones, and flesh with paralysis. Hence, we need to pay attention to the connection between the cartilage, muscle, synovium, as well as other tissues around the knee joint in KOA. In modern medicine, both muscle and bone inflammation, which are major components of the immune homeostasis of arthritis, drive the progression of KOA pain. However, most studies focus on cartilage inflammation and synovial inflammation in bone joints, and there is a paucity of articles examining inflammatory phenomena in skeletal muscles. Therefore, more research on the role of skeletal muscle in inflammation is needed to gain a more comprehensive understanding of KOA and provide ideas for more effective treatment modalities. In a review of the literature, we found that inhibition of the immune-related factor programmed death ligand 1 (PD-L1) exacerbated the progression of KOA10,11 and that there was differential expression of IL-15 and FOXO1 in the skeletal muscle of patients with KOA12, as well as significant skeletal muscle inflammation in patients with end-stage KOA, which was also associated with changes in gait. It has been shown that the skeletal muscle can also secrete factors closely related to inflammatory immunity such as IL-6, and that TNF-α is also closely related to the PD-L1 pathway and KOA13,14,15.
Currently, available treatments for KOA include weight control, exercise, medication, and surgery, which usually include intra-articular injections, analgesic medication, arthroscopic surgery, and periprosthetic osteotomy of the knee16. Currently, KOA disease progression cannot be completely stopped or reversed, and without a clear understanding of the complex mechanisms underlying KOA pain, KOA patients are at risk for overuse of analgesic medications and a high incidence of side effects8. Most treatment strategies are effective only for short periods and focus only on the temporary relief of symptoms rather than on the pathogenesis of the disease. Therefore, KOA pain remains a priority and a challenge for treatment, posing a serious clinical challenge. However, Tuina can directly stimulate the skeletal muscles around the affected joint in KOA treatment and can provide some benefits. Combined with the previous description, it is the ideal therapy to study the role of skeletal muscle tissue in KOA, and clarifying the role of skeletal muscle tissue in inflammation can also provide better theoretical support for Tuina of KOA.
Studies have shown that massage therapy, osteopathic manipulative therapy, and spinal manipulation can help relieve pain and restore body function17,18. These manipulations can act on local inflammation and relieve spasms and analgesia through external mechanical action. They can relieve pain after total knee arthroplasty, reduce the use of analgesic drugs, promote postoperative recovery, and improve biomechanical balance19. Swedish massage is feasible in the treatment of osteoarthritis and can reduce stress and improve quality of life20. The therapeutic effect of Tuina on KOA has been preceded by certain studies.
In this experiment, our team will explore whether the expression of PD-L1 and related inflammatory factors in skeletal muscle can induce KOA and promote its development based on the MIA-induced KOA model in rats. Tuina will also be implemented to see whether it can alleviate KOA symptoms caused by increased inflammatory factor expression. Tuina will be combined with PD-L1 inhibition to demonstrate the association between Tuina-mediated PD-1 pathway in skeletal muscle inflammation affecting KOA development and pain, laying the foundation for further multi-level studies on the therapeutic mechanisms of Tuina intervention in KOA.
In summary, this paper describes the investigation and elaboration of the mechanisms of skeletal muscle inflammation in the development of KOA and its pain, as well as the therapeutic effects of Tuina on KOA, from the perspective of immune-inflammatory factor expression, combined with behavioral related indicators, to provide modern research evidence for the "imbalance of tendon and bone" theory in traditional Chinese medicine.
Protocol
All experiments were approved and supervised by the Animal Care and Use Committee of the Shanghai University of Traditional Chinese Medicine (approval number: SYXK2018-0040), which conforms to the stipulations in the World Medical Association Helsinki Declaration.
1. Animal preparation
- House 32 Sprague Dawley (SD) male rats aged 8 weeks and weighing 180-220 g in a specific pathogen-free housing apparatus under 12 h light/12 h dark cycles at 24 ± 2 °C and 60% humidity with a standard rodent pellet diet. All experimental operations on animals comply with the welfare ethics of experimental animals and animal experimental safety regulations.
- Randomize and cage rats into four groups of eight animals each after 1 week of adaptive feeding: antiPD-L1+Tuina (group A), model (group B), Tuina (group C), and sham surgery (group D).
2. Intra-articular injection of monosodium iodoacetate (MIA) in the knee
NOTE: Except for group D, the KOA rat model will be prepared by the knee joint cavity injection of MIA in all the groups. For group D, inject 25 µL of sterile physiological saline into the right knee joint cavity.
- Anesthetize the rat by placing it in an anesthetic cage and then introducing 2.5% isoflurane until it is fully anesthetized. Confirm the animal is fully anesthetized by waiting for the point when the young rat is lying on its back, its limbs stop moving, and there is no response in toe pinch (pedal reflex), palpebral reflex, and muscle relaxation.
- Add pet eye ointment and eye drops to the anesthetized young rats to prevent eye dryness.
- Shave the right hind limb of the rats and disinfect the knee joint with three alternating rounds of iodophor and 75% ethanol.
- To maintain a standardized experimental condition, carefully fix the knee flexion at a precise angle of 90°, ensuring that the patellar ligament is oriented upwards. Subsequently, inject 25 µL of MIA solution, consisting of 4 mg of MIA diluted in 25 µL of sterile saline solution into the right knee joint cavity of the rats.
NOTE: This injection was carried out with a specialized microinjector, ensuring accuracy and consistency in the procedure21,22,23. Put the rats back into the cages until they wake up. The animal that has undergone surgery is not returned to the company of other animals until fully recovered. - At the end of the study, euthanize the rats by injecting 1% pentobarbital sodium as a 100 mg/kg dose.
3. Implementation of Tuina
NOTE: The implementation ofTuina will be guided by the theory that "for patients with tendon and bone imbalance, tendons need to be treated first". Both groups A and B started the intervention on the first day after the successful evaluation of the model, and both groups were operated once a day for 14 days. The remaining two groups were only observed for 14 days without any intervention. The operators of the manipulation must be strictly trained before the experiment to ensure the consistency of force, frequency, and rhythm.
- Accurately locate the rat acupuncture point, including EX-LE4, ST35, SP10, ST34, SP9, and GB34 (Figure 1 and Table 1), where finger kneading methods will be carried out by using Experimental Acupuncture24.
- Fix the rat in the prone position on the rat fixation equipment.
- After it is quiet and the lower limbs are relaxed, knead the EX-LE4 and ST35 of the affected limb with the thumb and the index finger simultaneously for 4 min at 120-140 times/min.
- Knead the anterior and medial-lateral muscles of the affected limb with the thumb and the index finger for 3 min at 120-140 times/min, focusing on the SP10, ST34, and the muscles near the knee joint. Emphasize the manipulation of those stiff muscles with an intensity so that the rat does not struggle.
- Knead the posterior calf muscles of the affected limb from top to bottom for 3 min at 120-140 times/min by using the thumb, the index finger, and the middle finger. To fully expose the treatment area, use the ring finger and the little finger to hold the ankle joint of the affected limb and gently tug on the affected limb. Focus on SP9, GB34, and the muscles near the knee joint with emphasis on the rigid muscles and intensity so that the rat does not struggle.
4. Measurement of behavioral index
- Measurement of plantar mechanical pain threshold
NOTE: Measure plantar mechanical pain thresholds 1 day before MIA injection as well as 2, 9, and 16 days after injection.- Bring the rats to a plantar test room with a stainless-steel grid bottom and a plastic cage body in a quiet environment at room temperature (22 ± 2) °C for 30 min of adaptation.
- Use an electronic mechanical pain tester with a plastic test needle of 0.8 mm in diameter to stimulate the central area of the right hindfoot of the rats vertically. Evenly and gradually increase the stimulation intensity until the rats show paw retraction and avoidance reactions.
- Record the reading of the electronic screen as the mechanical pain threshold of the right plantar foot of the rat.
- Measure each rat 5x at 5 min intervals.
- Remove the maximum and minimum values from the five values. Take the average value of the middle three values through the trimmed mean method as the result (Table 2).
- Measurement of paw mechanical withdrawal threshold
NOTE: Measure paw mechanical withdrawal threshold 1 day before MIA injection, 2, 9, and 16 days after injection.- Bring the rats to a heated plantar test room with a 30 °C glass bottom and a plastic cage body in a quiet environment at room temperature (22 ± 2) °C for 30 min of adaption.
- Stimulate the right hind plantar center area with a light source heating device at a stimulation temperature of 65 °C until the rat shows a paw retraction and avoidance response.
- Record the time reading of the electronic screen as the right plantar thermal pain threshold of the rat.
- Measure each rat 5x continuously at 5 min intervals.
- Remove the maximum and minimum values from the five values. Take the average value of the middle three values through the trimmed mean method as the result (Table 3).
5. Measurement of swelling of the right knee joint
NOTE: Measure the swelling of the right knee joint of rats 1 day before MIA injection, 2, 9, and 16 days after the injection.
- Anesthetize the rat by placing it in an anesthetic cage and exposing it to 2.5% isoflurane until it is fully anesthetized.
- Place the rat in a flat position on the operating table.
- Measure the width of the right knee joint with vernier calipers (Figure 2 and Table 4).
6. Measurement of the Lequesne MG score
NOTE: Measure the Lequesne MG score in rats at 2, 9, and 16 days after MIA injection. Lequesne et al developed an index of severity for osteoarthritis for the hip (ISH), which can be used to assess the effectiveness of therapeutic interventions. We consider four parameters: pain stimulation, gait change, joint mobility, and joint swelling.
- Bring the rats to a manipulation platform in a quiet environment at room temperature (22 ± 2) °C.
- Have two operators, blinded to each other, measure the local pain stimulation response, gait change, joint movement, and joint swelling.
- Stimulate the lateral side of the right knee joint with a plastic test needle and score on a scale of 0-3 according to the response. 0 no response; 3 a good response; 1 contraction of the affected limb; 2 contraction and spasm of the affected limb, accompanied by mild generalized reactions, such as trembling, licking, and sucking.
- Place the rat on the operating table and observe the gait of its right hind limbs. Score on a scale of 0-3 according to the response. 0 no disturbance in the movement of the affected limb, normal running, and strong footwork; 3 the affected limb cannot participate in walking, touch the ground, or stomp on the ground; 1 mild trekking during running with strong stomps; 2 the affected limb participates in walking, but the disturbance in movement of the rats (trekking) is obvious.
- Flex and extend the right knee joint of the rat by hand and observe the joint mobility. Score on a scale of 0-3 according to the response. 0 joint mobility angle of more than 90°; 3 joint mobility angle of less than 15°; 1 joint mobility angle or 45°-90°; 2 joint mobility angle of 15°-45°.
- Touch the right knee joint of the rat and compare the response with that of a normal rat. Score on a scale of 0-2 according to the response. 0 no obvious swelling and visible bony markings; 2 marked swelling and no bony markings; 1 mild swelling and superficial bony markings.
- Add these scores to produce the Lequesne MG score for each rat and calculate the average value through the trimmed method (Table 5).
7. Measurement of skin temperature
NOTE: Measure the skin temperature 1 day before MIA injection and 9 and 16 days after injection.
- Anesthetize the rat by placing it in an anesthetic cage and then introducing isoflurane until it is fully anesthetized.
- Place the rat in a lateral position on the operating table, at room temperature (22 ± 2) °C.
- Straighten the right knee joint by gently grasping the foot with the hand. Photograph to determine the skin temperature by using a Filr infrared camera.
- Read the skin temperature of the knee joint and around the knee joint of the rat by using supporting editing software. Set control points at the ankle joint and knee joint where the temperature gradually decreases.
8. Statistical analysis
- Use statistical software to express the experimental data in quartiles.
- Use the trim mean method to deal with the outliers. The outcomes of behavioral tests are noted as the mean ± standard error of the mean.
- Perform independent samples t-test for comparison between groups. Analyze the behavioral data using a two-way repeated measure analysis of variance (ANOVA), followed by Bonferroni's multiple comparison tests. Where data do not exhibit normality or homoscedasticity, perform a non-parametric test (Kruskal-Wallis k samples).
NOTE: P < 0.05 indicates that the differences are statistically significant. All the data meet the assumptions of the statistical tests that are applied.
Representative Results
The described protocol was implemented in a clinical setting at Yueyang Hospital of Integrated Traditional Chinese and Western Medicine. Figure 1 shows the exact location of the acupoints pushed in rats, and Table 1 illustrates the common benefits of stimulating these points. Table 2 and Table 3 offer compelling evidence of notable pain relief achieved through Tuina therapy, even in the absence of PD-1 pathway inhibition. The findings presented in Table 4, Table 5, and Figure 2 additionally illustrate the correlation between Tuina application and the progression of knee osteoarthritis (KOA), implying that manual therapy could serve as an adjunctive approach for enhancing KOA symptom management in rats. We injected each rat in the Manual therapy Anti-PD-L1 (MTA) group with a dose of 200 µg of anti-PD-L1 to block the pathway after 3 days of the osteoarthritis induction of MIA. Then, the rats were subjected to manual therapy in the rat acupuncture points, including EX-LE4, ST35, SP10, ST34, SP9, and GB34, every 2 days for 2 weeks, using finger kneading methods after 3 days post osteoarthritis induction.
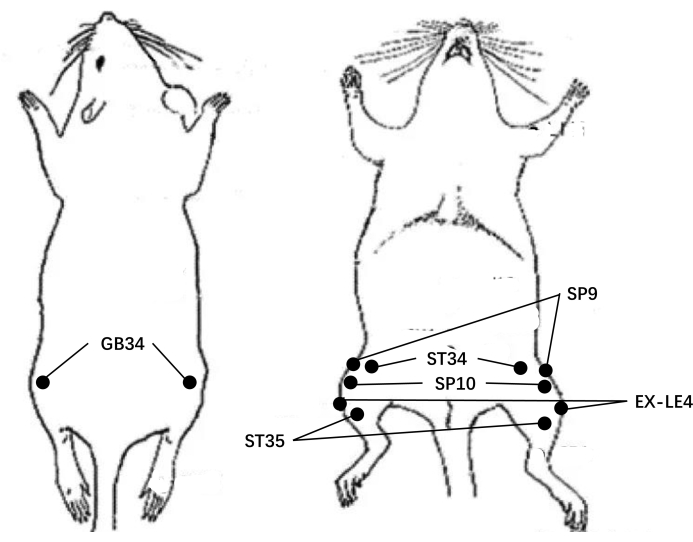
Figure 1: The diagram of the points in rats. Please click here to view a larger version of this figure.
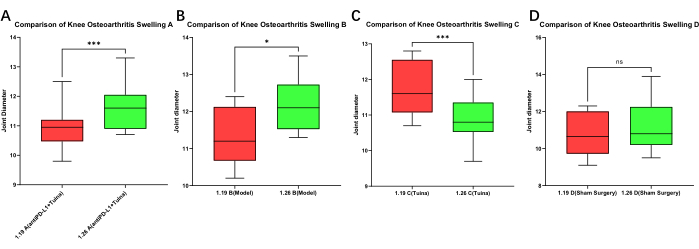
Figure 2: Various degrees of swelling of the knees in rats. The swelling can be controlled through the implementation of Tuina. Before the PD-L1 pathway was blocked, the right knee joint diameters (the knee that was injected with MIA) were measured (on January 19th) and measured again after 1 week. The effects of Tuina on controlling the swelling of the knee become insignificant after PD-L1 blockade. *** represent P < 0.0001, ** represent P < 0.01, * represents P < 0.05). Please click here to view a larger version of this figure.
| Acupuncture Points | Functions |
| EX-LE4 | Relieve knee swelling and pain |
| ST35 | Allevate joint dysflexia |
| SP10 | Ease medial femoral pain |
| ST34 | Joint paralysis intervention |
| SP9 | Relieve knee pain |
| GB34 | Relieve lower limb paralysis |
Table 1: The effect of stimulating these points.
| Baseline | 1 week | 2 weeks | |
| Group A | 58.01 | 29.61 | 27.9 |
| (antiPD-L1 + Tuina) | |||
| Group B | 31.76 | 25 | 23.52 |
| (model) | |||
| Group C | 34.15 | 32.45 | 37.53 |
| (Tuina) | |||
| Group D | 40.26 | 43.93 | 51.3 |
| (Sham surgery) |
Table 2: Comparison of mechanical pain thresholds between groups at baseline (the day of PD-L1 blockade), 1 week, and 2 weeks after successful induction. The data in the table are the mean values of each group measured on that day. The P value between any two groups is <0.05 except the P value between groups A and B.
| Baseline | 1 week | 2 weeks | |
| Group A | 9.67 | 6.72 | 7.82 |
| (antiPD-L1 + Tuina) | |||
| Group B | 7.5 | 7.25 | 6.39 |
| (model) | |||
| Group C | 11.67 | 8.63 | 9.26 |
| (Tuina) | |||
| Group D | 12.8 | 10.8 | 10.14 |
| (Sham surgery) |
Table 3: Comparison of the thermal pain thresholds between groups at baseline, 1 week, and 2 weeks after successful induction. The data in the table are the mean values of each group measured on that day. The P value between any two groups is <0.05 except the P value between groups A and B.
| Baseline | 1 week | 2 weeks | |
| Group A | 10.96 | 11.68 | 10.56 |
| (antiPD-L1 + Tuina) | |||
| Group B | 11.3 | 12.18 | 11.79 |
| (model) | |||
| Group C | 11.75 | 10.88 | 10.35 |
| (Tuina) | |||
| Group D | 10.8 | 11.23 | 10.49 |
| (Sham surgery) |
Table 4: Comparison of knee osteoarthritis swelling between groups at baseline, 1 week, and 2 weeks after successful induction. The data in the table are the mean values of each group measured on that day. The P value between any two groups is <0.05 except the P value between groups A and B)
| Baseline | 1 week | 2 weeks | |
| Group A | 3.13 | 4.25 | 3.88 |
| (antiPD-L1 + Tuina) | |||
| Group B | 2.63 | 4.5 | 4.75 |
| (model) | |||
| Group C | 2.75 | 1.88 | 2.25 |
| (Tuina) | |||
| Group D | 0 | 0 | 0 |
| (Sham surgery) |
Table 5: Comparison of Lequesne MG index between groups at baseline, 1 week, and 2 weeks after successful induction. The data in the table are the mean values of each group measured on that day. The P value between any two groups is <0.05 except the P value between groups A and B.
Discussion
This study aims to assess the improvement of KOA after Tuina intervention by using standardized behavioral indicators and investigate the mechanisms of Tuina for KOA and the association between skeletal muscle and KOA. Unlike pharmacological and surgical therapies, Tuina has a positive regulatory effect on the motor, immune, and endocrine systems. Tuina can relieve inflammation and pain produced by disease by acting on different targets. For example, by regulating the TLR4 pathway and miRNA, it can inhibit the activation of glial cells, modulate altered brain function, regulate downstream inflammatory cytokines, and suppress peripheral inflammation25,26,27. At the same time, Tuina can also intervene in the autonomic nervous system and hypothalamic-pituitary-adrenal axis that are dysfunctional in chronic pain disorders, thus helping to restore autonomic nervous system homeostasis and trigger an immunoendocrine response, which can relieve pain by regulating endocrine and physiological processes28,29,30. Additionally, when Tuina externally stimulates muscles, parasympathetic excitation31, and extravascular pressure in vitro cause skeletal muscle contraction and vasodilation, which contributes to the congestive response and promotes metabolism32,33. Therefore, as a non-pharmacological and non-surgical treatment, Tuina is a promising therapy for the relief of KOA.
We also reviewed the literature on the therapeutic effects of aerobic exercise, traditional Chinese medicine (TCM), and electroacupuncture on the KOA model induced by monosodium iodoacetate (MIA). Aerobic exercise can inhibit chondrocyte apoptosis by regulating the expression of TRPV5, and the combination of aerobic exercise and glucosamine hydrochloride capsules may be even more effective34,35. Compounds purified from Chinese herbs, such as Casticin and vanillic acid, can reduce knee osteoarthritis synovial inflammation and pain-related behavior/mediator in vivo. Compounds purified from Chinese herbs, such as Casticin and vanillic acid36, can reduce KOA synovial inflammation and pain-related behavior/mediator in knee osteoarthritis in vivo. In addition, vanillic acid can protect knee joints by inhibiting NLRP3 inflammasome activation37. Furthermore, electroacupuncture has been demonstrated to inhibit the NLRP3 inflammasome and reduce pyroptosis, leading to the preservation of cartilage tissue and the treatment of KOA38.
Unlike TCM, Tuina requires different forms of movement for clinical treatment, combining multiple techniques and passive movement of the patient, which is often a problem for new practitioners in choosing the appropriate technique, site of action, and strength of action. In addition, the evaluation of posttreatment efficacy is a major challenge in manipulative therapy, as it has mostly been limited to subjective descriptions of patients, with no objective data to evaluate methods and practices. Therefore, we aimed to investigate the mechanisms of skeletal muscle inflammation in the development of KOA and pain and examine the therapeutic effects of Tuina on KOA based on a rat model of KOA, induced with MIA, combined with behavioral and inflammatory factor-related indicators. At the same time, since Tuina is guided by the theory that "for patients with tendon and bone imbalance, tendons need to be treated first", the rat acupuncture point list in Experimental Acupuncture will be used to accurately locate the EX-LE4, ST35, SP10, ST34, SP9, and GB34 to implement finger-kneading rubbing methods. Therefore, the operators performing the manipulation should be strictly trained before the intervention is applied to ensure the consistency of force, frequency, and rhythm.
Table 2 and Table 3 provide evidence that pain has been significantly relieved by the Tuina without the blockade of the PD-1 pathway. The results in Table 4, Table 5, and Figure 2 further demonstrate the relationship between the implementation of Tuina and KOA progression, suggesting that manual therapy can be a supplementary treatment for KOA to improve the rats' KOA symptoms. Therefore, treatment with Tuina may be an effective intervention to combat the progression of KOA; however, more in-depth studies are required to clarify its mechanism.
Furthermore, there are some limitations to this experimental protocol. First, as there are overactive or quiet rats and there may be some error in the measurement of mechanical pain, each measurement needs to be timed with regular intervals between each measurement. Second, this experimental design is designed to study the MIA-induced KOA rat model, and further research is needed to illustrate the clinical therapeutic effects of Tuina. However, our team focused on the effect of KOA on skeletal muscle, the improvement of muscle and KOA by Tuina, and the relation with the PD-1 pathway, aiming to investigate the mechanism of Tuina intervention in KOA. In the future, we will aim to promote the feasibility, safety, and efficacy of manipulation therapy and conduct further research on the clinical efficacy of Tuina on skeletal muscle. While studying the association between tendons and bones, the pathogenesis of KOA, and the mechanisms of manipulation therapy intervention, we also hope to apply our research findings and ideas to other diseases.
Declarações
The authors have nothing to disclose.
Acknowledgements
This study is supported by National Natural Science Foundation of China (NO.82105042, 82205302); Shanghai Post-doctoral Excellence Program (NO.2020371); China Postdoctoral Science Foundation (NO.2021M692156); Shanghai Sailing Program (NO.20YF1450900); Science Foundation of Yueyang Hospital of Integrated Traditional Chinese and Western Medicine (NO.2021yygq03). The funders had no role in the design, execution, or writing of the study.
Materials
| Anti-PD-L1 | Abcam, Cambridge, MA, USA | ab80276 | |
| electric von Frey esthesiometer | IITC/Life Science, Woodland Hills, CA, USA | ALMEMO 2450 | |
| GraphPad Prism 9.0 | GraphPad Software | Software for stastistical analysis | |
| monosodium iodoacetate | Sigma-Aldrich Inc | I9148 | Resolved into normal saline for injection |
| pentasorbital sodium | Sigma-Aldrich Inc | P3761 | |
| Sprague Dawley (SD) male rats | Shanghai Jihui Experimental Animal Breeding Co., Ltd | No. SCXK (Hu) 2017-0012 | |
| thermal analgesia tester | IITC/Life Science | Model 390 |
Referências
- Katz, J. N., et al. Diagnosis and treatment of hip and knee osteoarthritis: A review. JAMA. 325 (6), 568-578 (2021).
- Culvenor, A. G., et al. Prevalence of knee osteoarthritis features on magnetic resonance imaging in asymptomatic uninjured adults: a systematic review and meta-analysis. Br J Sports Med. 53 (20), 1268-1278 (2019).
- Safiri, S., et al. regional and national burden of osteoarthritis 1990-2017: a systematic analysis of the Global Burden of Disease Study 2017. Ann Rheum Dis. 79 (6), 819-828 (2020).
- Kong, L., et al. Traditional Chinese exercises on pain and disability in middle-aged and elderly patients with neck pain: a systematic review and meta-analysis of randomized controlled trials. Front Aging Neurosci. 14, 912-945 (2022).
- Nevitt, M. C., et al. Symptoms of knee instability as risk factors for recurrent falls. Arthritis Care Res (Hoboken). 68 (8), 1089-1097 (2016).
- Hunter, D. J., March, L., Chew, M. Osteoarthritis in 2020 and beyond: a Lancet Commission). Lancet. 396 (10264), 1711-1712 (2020).
- Fan, Z. J., et al. Interpretation and evaluation of the Chinese Osteoarthritis Treatment Guidelines (2021 Edition). Chinese Journal of Evidence-Based Medicine. 22 (06), 621-627 (2022).
- Chen, W., et al. Design of an epidemiological survey on the prevalence of osteoarthritis of the knee in a middle-aged and elderly population in China. Journal of Hebei Medical University. 36 (04), 487-490 (2015).
- Shao, S. Study on the mechanism of regulating the "balance of tendon and bone force" in the treatment of knee osteoarthritis by Tui Na manipulation. Shanghai University of Traditional Chinese Medicine. , 107-108 (2020).
- Liu, S. Role and mechanism of PD-1/PD-L1 pathway in osteoarthritis in mice. Shandong University. , 130-134 (2020).
- Shoujian, PD-1 promotes the repair and regeneration of contused skeletal muscle by regulating Treg cells and macrophages. Shanghai Institute of Physical Education. , 54-58 (2020).
- Levinger, P., et al. The level of FoxO1 and IL-15 in skeletal muscle, serum and synovial fluid in people with knee osteoarthritis: a case control study. Osteoporos Int. 27 (6), 2137-2143 (2016).
- Niu, Q., Xie, C., Jiang, Z. Advances in Chinese medicine based on PI3K/AKT signaling pathway for the treatment of knee osteoarthritis. Massage and Rehabilitation Medicine. , 1-5 (2022).
- Liu, S., et al. Blocking of checkpoint receptor PD-L1 aggravates osteoarthritis in macrophage-dependent manner in the mice model. Int J Immunopathol Pharmacol. 33, 2058-2073 (2019).
- Molanouri, S. M., et al. Combined effect of aerobic interval training and selenium nanoparticles on expression of IL-15 and IL-10/TNF-alpha ratio in skeletal muscle of 4T1 breast cancer mice with cachexia. Cytokine. 90, 100-108 (2017).
- Mahmoudian, A., et al. Early-stage symptomatic osteoarthritis of the knee – time for action. Nat Rev Rheumatol. 17 (10), 621-632 (2021).
- Nahin, R. L., et al. Evidence-based evaluation of complementary health approaches for pain management in the United States. Mayo Clin Proc. 91 (9), 1292-1306 (2016).
- Bervoets, D. C., et al. Massage therapy has short-term benefits for people with common musculoskeletal disorders compared to no treatment: a systematic review. J Physiother. 61 (3), 106-116 (2015).
- Xu, H., et al. Effectiveness of tui na in treating pain after total knee replacement for knee osteoarthritis. Chinese Tissue Engineering Research. 25 (18), 2840-2845 (2021).
- Ali, A., et al. Massage therapy and quality of life in osteoarthritis of the knee: a qualitative study. Pain Med. 18 (6), 1168-1175 (2017).
- Yoh, S., et al. Intra-articular injection of monoiodoacetate induces diverse hip osteoarthritis in rats, depending on its dose. BMC Musculoskelet Disord. 23 (1), 494-487 (2022).
- Lockwood, S. M., et al. Characterisation of peripheral and central components of the rat monoiodoacetate model of osteoarthritis. Osteoarthritis Cartilage. 27 (4), 712-722 (2019).
- McCoy, A. M. Animal models of osteoarthritis: Comparisons and key considerations. Vet Pathol. 52 (5), 803-818 (2015).
- Guo, X. Exploring the effect of pushing on cartilage in rats with knee osteoarthritis based on ROCK/LIMK1/Cofilin signaling pathway. Chongqing Medical University. , 42-44 (2022).
- Liu, Z. F., et al. Tuina for peripherally-induced neuropathic pain: A review of analgesic mechanism. Front Neurosci. 16, 1096-1104 (2022).
- Gebremariam, L., et al. Subacromial impingement syndrome–effectiveness of physiotherapy and manual therapy. Br J Sports Med. 48 (16), 1202-1208 (2014).
- Yao, C., et al. Transcriptome profiling of microRNAs reveals potential mechanisms of manual therapy alleviating neuropathic pain through microRNA-547-3p-mediated Map4k4/NF-kappab signaling pathway. J Neuroinflammation. 19 (1), 211-221 (2022).
- Valera-Calero, A., et al. Endocrine response after cervical manipulation and mobilization in people with chronic mechanical neck pain: a randomized controlled trial. Eur J Phys Rehabil Med. 55 (6), 792-805 (2019).
- Kovanur, S. K., et al. Measureable changes in the neuro-endocrinal mechanism following spinal manipulation. Med Hypotheses. 85 (6), 819-824 (2015).
- Colombi, A., Testa, M. The effects induced by spinal manipulative therapy on the immune and endocrine systems. Medicina (Kaunas). 55 (8), 312-314 (2019).
- Afify, A., Mark, H. F. Fluorescence in situ hybridization assessment of chromosome 8 copy number in stage I and stage II infiltrating ductal carcinoma of the breast. Cancer Genet Cytogenet. 97 (2), 101-105 (1997).
- Kirby, B. S., et al. Mechanical influences on skeletal muscle vascular tone in humans: insight into contraction-induced rapid vasodilatation. J Physiol. 583, 861-874 (2007).
- Sefton, J. M., et al. Therapeutic massage of the neck and shoulders produces changes in peripheral blood flow when assessed with dynamic infrared thermography. J Altern Complement Med. 16 (7), 723-732 (2010).
- Chen, B., et al. Aerobic exercise combined with glucosamine hydrochloride capsules inhibited the apoptosis of chondrocytes in rabbit knee osteoarthritis by affecting TRPV5 expression. Gene. 830, 146465 (2022).
- Fang, L., et al. The mechanism of aerobic exercise combined with glucosamine therapy and circUNK in improving knee osteoarthritis in rabbits. Life Sci. 275, 119375 (2021).
- Li, X., et al. Casticin suppresses monoiodoacetic acid-induced knee osteoarthritis through inhibiting HIF-1alpha/NLRP3 inflammasome signaling. Int Immunopharmacol. 86, 106745 (2020).
- Ma, Z., et al. Vanillic acid reduces pain-related behavior in knee osteoarthritis rats Through the inhibition of NLRP3 inflammasome-related synovitis. Front Pharmacol. 11, 599022 (2020).
- Zhang, W., et al. Electroacupuncture ameliorates knee osteoarthritis in rats via inhibiting NLRP3 inflammasome and reducing pyroptosis. Mol Pain. 19, 17448069221147792 (2023).

