淋巴结考试
English
COMPARTILHAR
Visão Geral
资料来源: 公共卫生与社会医学系助理教授理查德 · 格利克曼-西蒙,MD,塔夫斯大学医学院马
淋巴系统有两个主要功能: 细胞外液后回到静脉的循环,揭露对免疫系统的抗原物质。随着收集到的液体穿过淋巴管及其返回途中在全身的循环,它遇到多个节点组成的淋巴细胞高度集中集群。大多数淋巴通道和节点驻留在身体深处,因此,不可以访问物理考试 (图 1)。只有在地表附近的节点可以检查或触诊。淋巴结是通常不可见,并且规模较小的节点也非显而易见。然而,更大的节点 (> 1 厘米) 在脖子、 腋窝、 和腹股沟区往往为嵌入在皮下组织中的柔软、 滑爽、 动产、 非标、 豆形肿块的检出。
淋巴结肿大通常表明感染或较少,淋巴引流区癌症。节点可能成为扩大、 固定、 坚定,和/或根据病理本投标。例如,位非常软、 投标明显的下颌骨角附近的淋巴结可能表明感染的扁桃体,而位非常坚定、 扩大、 非标可触知的女性病人腋下的淋巴结可能是乳腺癌的标志。
区域淋巴结引流区域的局部感染通常仍然看不见但也许变得扩大和招标触诊。伤口感染或蜂窝组织炎也可能导致淋巴管炎或淋巴结炎、 传染链的淋巴通道和节点的一个条件。这可能伴随着红色的条纹和全身症状,如发热、 发冷和不适的外观。在罕见的情况下,强度的炎症反应可能会导致节点以坚持周围的软组织,固定他们的地方。
许多的转移性癌症首先传播到区域淋巴结。与不同的感染,恶性细胞的浸润淋巴结可能会导致他们感到不规则和公司 (甚至岩石般坚硬),但仍非标。如果癌症侵入外胶囊,节点可能成为固定到周围软组织或缠结在一起。淋巴瘤,原发癌固有的淋巴系统,可能会出现在身体任何地方作为单个或多个淋巴结肿大,可能变得足够大,而在检查时,看到的一般硬和非标上触诊。除了淋巴瘤,弥漫性淋巴结肿大可能是广义的感染性或炎性疾病,如艾滋病毒、 单核细胞增多或结节病的征兆。
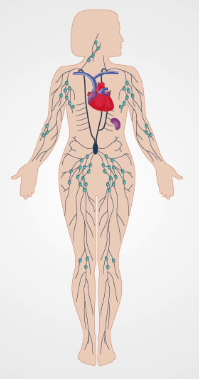
图 1。淋巴系统。
Procedimento
Applications and Summary
Most lymph nodes lie too deep to be accessible via physical examination. The superficial nodes are most efficiently assessed during regional examinations of the head and neck, breasts and axillae, upper extremities, lower extremities, and/or external genitalia. Because lymph nodes are constantly interacting with extracellular fluid draining from nearby tissues, their examination can provide information about the presence and status of infections or malignancies in the area. Nodes draining the site of a soft tissue infection are apt to become enlarged and tender but generally remain soft, smooth, and mobile. Hard, non-tender, matted, or fixed nodes are more typical of a spreading malignancy. Diffuse lymphadenopathy may indicate systemic diseases such as lymphomas, HIV, mononucleosis, or sarcoidosis. Finding a single abnormal node should prompt an examination of all nodes.
Transcrição
The lymph node examination forms an essential part of the evaluation for infectious diseases and cancer. The lymphatic system is comprised of organs including the spleen, lymphatic channels and lymph nodes. The channels are responsible for returning the lymph formed from extracellular fluid back to the venous circulation.
On its way, the lymph encounters multiple lymph nodes. These nodes consist of highly concentrated clusters of lymphocytes, which play a critical role in maintaining immunity. Most lymph channels and nodes reside deep within the body and are too small to be assessed by physical examination. However, superficial, larger nodes, close to or more than one centimeter in diameter-primarily located in the head and neck region, the axillae and the inguinal areas-can be palpated and assessed.
Lymph nodes in these areas normally present as soft, smooth, movable, non-tender, bean-shaped structures imbedded in the subcutaneous tissue. However, sometimes nodes may become enlarged, fixed, firm, and/or tender depending on the pathology present. This condition is referred to as lymphadenopathy and it usually indicates an infection or, less commonly, a cancer in the area of lymph drainage. This video will review the anatomical location of the key lymph nodes as well as demonstrate the procedural steps of this examination.
Let’s begin by briefly reviewing the lymph nodes in the head and neck area. The list of palpable nodes in this region is extensive including the preauricular and posterior auricular nodes located in front and behind the ear, respectively, the mastoid node positioned superficial to the mastoid process and the occipital nodes found at the base of the skull. Around the mandible are the tonsillar nodes, the submandibular nodes, and the submental nodes. Another group of nodes surround the sternomastoid muscle. These include the superficial and deep cervical nodes. The last groups of nodes are the clavicular nodes, including the supra- and the infra-clavicular nodes. The infraclavicular nodes are also known as the apical nodes.
Upon entering the examination room, introduce yourself and briefly explain the maneuvers you’re going to conduct. Before beginning with the examination, sanitize your hands by using topical disinfectant solution. Start by asking the patient to flex their neck slightly forward and inspect for noticeably enlarged nodes. Following inspection, palpate the preauricular node located in front of the ear. Throughout the exam, palpate using the pads of your index and middle fingers to note the size, shape, number, pliability, texture, mobility, and tenderness of nodes bilaterally.
Next, move to the posterior auricular node located behind the ear followed by the mastoid node located superficial to the mastoid process, and the occipital nodes found posteriorly at the base of the skull. Then move onto the tonsillar nodes located at the angle of mandible, the submandibular nodes that lie midway between the angle and tip of the mandible, and the submental nodes located a few centimeters from the tip. Next, palpate the superficial cervical nodes situated beneath and anterior to the sternomastoid muscles. The deep cervical nodes are rarely palpable. This is followed by palpation of the posterior cervical nodes located between the anterior edge of the trapezius and posterior edge of the sternomastoid muscles. Finally, palpate the supraclavicular nodes found deep within the angle formed by the sternomastoid muscle and clavicle, and the infraclavicular, or the apical nodes, located on the underside of the clavicle.
Following palpation of the head and neck nodes, move to the axillae and upper extremities. The three groups of axillary nodes-lateral, subscapular, and pectoral-drain their lymph into the central axillary nodes that lay deep within the axillae. The central nodes, in turn, drain lymph into the apical and supraclavicular nodes. Of the four axillary groups, only the central nodes are usually palpable. Since most breast cancers drain here, the axillary and clavicular lymphatics need to be examined more carefully in women. Most parts of the upper extremities drain more or less directly into the axillary lymph nodes. One exception is drainage from the ulnar aspects of the hand and forearm, which first encounters the epitrochlear nodes above the elbow.
To examine the left axillary nodes, position yourself in front and to the left of the seated patient. Gently grasp the patient’s left wrist or elbow and slightly abduct the arm. Inform the patient that the following maneuver may feel slightly uncomfortable. Move your right hand high up into the left axilla, just behind the pectoralis muscle. With your fingers pointing toward the mid-clavicle, press them against the patient’s chest wall, and slide them downward to feel the central nodes. Subsequently, you can palpate the apical and supraclavicular nodes if missed during the head and neck examination. While supporting the patient’s left arm in the same position, palpate the patient’s epitrochlear nodes, which are located medially about three centimeters above the elbow. Repeat the entire examination on the patient’s right using your left hand.
With the patient’s axilla and upper extremity examination complete, proceed to the lower extremities. This region includes the superficial inguinal lymph nodes, which are located high in the anterior thigh and drain various regions of the legs, abdomen, and perineum. These nodes are often large enough to palpate, even when normal, and can be subdivided into two groups: the horizontalgroup located just below the inguinal ligament and the vertical group located just below the femoral artery pulse.
In order to palpate these nodes, ask the patient to lay supine with their hips fully extended or slightly flexed. Once the patient is comfortable begin palpating the horizontalgroup of nodes just below the inguinal ligament. Move your hand along the entire length of the ligament, taking note of the nodes’ size, shape and firmness. Finally, palpate the vertical group of nodes, which is medial to the horizontal group and just below the femoral artery pulse. This concludes the lymph node examination. Thank the patient for their cooperation.
You have just watched JoVE’s video documenting the lymph node examinations of patients’ head and neck areas, axillae, upper extremities and lower extremities. You should now understand the systematic sequence of steps that every physician should follow in order to conduct an effective lymph node exam. As always, thanks for watching!
