Isolation, Culture, and Imaging of Human Fetal Pancreatic Cell Clusters
Summary
A protocol to isolate, culture, and image islet cell clusters (ICCs) derived from human fetal pancreatic cells is described. The method details the steps necessary to generate ICCs from tissue, culture as monolayers or in suspension as aggregates, and image for markers of proliferation and pancreatic cell fate decisions.
Abstract
For almost 30 years, scientists have demonstrated that human fetal ICCs transplanted under the kidney capsule of nude mice matured into functioning endocrine cells, as evidenced by a significant increase in circulating human C-peptide following glucose stimulation1-9. However in vitro, genesis of insulin producing cells from human fetal ICCs is low10; results reminiscent of recent experiments performed with human embryonic stem cells (hESC), a renewable source of cells that hold great promise as a potential therapeutic treatment for type 1 diabetes. Like ICCs, transplantation of partially differentiated hESC generate glucose responsive, insulin producing cells, but in vitro genesis of insulin producing cells from hESC is much less robust11-17. A complete understanding of the factors that influence the growth and differentiation of endocrine precursor cells will likely require data generated from both ICCs and hESC. While a number of protocols exist to generate insulin producing cells from hESC in vitro11-22, far fewer exist for ICCs10,23,24. Part of that discrepancy likely comes from the difficulty of working with human fetal pancreas. Towards that end, we have continued to build upon existing methods to isolate fetal islets from human pancreases with gestational ages ranging from 12 to 23 weeks, grow the cells as a monolayer or in suspension, and image for cell proliferation, pancreatic markers and human hormones including glucagon and C-peptide. ICCs generated by the protocol described below result in C-peptide release after transplantation under the kidney capsule of nude mice that are similar to C-peptide levels obtained by transplantation of fresh tissue6. Although the examples presented here focus upon the pancreatic endoderm proliferation and β cell genesis, the protocol can be employed to study other aspects of pancreatic development, including exocrine, ductal, and other hormone producing cells.
Introduction
A primary limitation to cell-based insulin replacement therapies in type 1 diabetes is the paucity of human islets available for transplantation. The ability to regulate proliferation and differentiation of human pancreatic precursor cells into insulin-producing cells that meet the metabolic demands of an insulin-deficient state remains a critical building block for a cell-based therapy to treat type 1 diabetes.
Until the advent of hESC derived insulin-producing cells, human fetal pancreatic endocrine cells or their precursors were viewed as potential sources of cells for clinical transplantation. Although the scientific and regulatory landscape has changed in the past few years, there remains a vital need to understand how the human fetal pancreas develops. Many now view therapeutic use of human fetal cells as unlikely, however if effective and safe methods to expand the cells were established, therapeutic use of these cells could again be explored. A major hurdle that remains is that in vitro transformation of human fetal pancreatic cells aggregates (ICCs) into glucose responsive, insulin secreting endocrine cells is currently an inefficient process. Although much work over almost 30 years has elucidated and delineated the expression profile of transcription factors required for the development of endocrine pancreas, there remain gaps in our knowledge about how temporal expression of transcription factors is regulated and related to cell function.
Until the advent of hESC derived insulin-producing cells, human fetal pancreatic endocrine cells or their precursors were viewed as potential sources of cells for clinical transplantation. Although the scientific and regulatory landscape has changed in the past few years, there remains a vital need to understand how the human fetal pancreas develops. Many now view therapeutic use of human fetal cells as unlikely, however if effective and safe methods to expand the cells were established, therapeutic use of these cells could again be explored. A major hurdle that remains is that in vitro transformation of human fetal pancreatic cells aggregates (ICCs) into glucose responsive, insulin secreting endocrine cells is currently an inefficient process. Although much work over almost 30 years has elucidated and delineated the expression profile of transcription factors required for the development of endocrine pancreas, there remain gaps in our knowledge about how temporal expression of transcription factors is regulated and related to cell function.
Recently, the stem cell field has employed the accumulated knowledge about temporal transcription factor expression during islet development to drive the production of cells that express the markers of mature endocrine cells. Although genesis of insulin producing cells from hESC and induced pluripotent cells (iPSC) has made substantial and significant advances in the past few years, the most effective protocols require two distinct differentiation phases: 1) an early in vitro differentiation to generate cells expressing pancreatic precursor transcription factors, followed by 2) in vivo maturation after transplant — a so called “black box” period. To move forward, advances in understanding the biology underlying islet maturation in vivo, regardless of cell source, must be understood at a biochemical level. The similarity between the results obtained with ICCs and hESC suggests that a number of critical biochemical processes that regulate the transition of human pancreatic precursor cells into mature, glucose responsive, insulin secreting cells in vitro remain unknown. A central part of this understanding will be to develop novel methodologies to derive functional endocrine cell populations from pancreatic progenitor cells and hESC will require not only biochemical approaches that elucidate the maturation events, but methods to analyze the changes.
Why do we believe that imaging human fetal pancreatic cells is a critical aspect of identifying changes in islet maturation? The answer lies partially in the historical quest to generate insulin producing cells. Both model and tissue-culture systems for pancreatic precursors and islets have allowed researchers to explore the significant differences that exist between maturation of animal islets and human islets in vitro. A limitation to the exploration of human fetal pancreas development is that the gestational ages that can be legally used only give rise to heterogeneous cell aggregates. Although the isolated fetal human cells resemble islets, staining after in vitro culture from gestational ages 9-23 weeks reveals less than 15% contain markers for endocrine cells, with most cells not staining for islet hormones. However, after transplantation and in vivo maturation, a large majority of cells express endocrine markers 6,25. The results from these studies are being echoed today with hESC differentiation protocols that are only able to generate modest populations of single hormone positive endocrine cells after in vitro differentiation. In vitro methods to enhance populations of hormone positive cells will likely provide insight into in vivo islet maturation. Furthermore, understanding the molecular events that drive human fetal pancreatic development will likely improve efforts to derive insulin producing cells from hESC and further delineate the mechanisms that regulate β cell regeneration and pancreatic cell transdifferentiation.
The similarities between human fetal pancreatic cell and hESC maturation can be extended to cell function. Like murine cells, both human fetal cells and differentiated hESC are unable to release insulin in response to glucose after islet neoformation in vitro26,27. However, upon transplantation into nude mice and maturation, both human islet-like clusters and insulin producing cells derived from hESC exhibit an endocrine phenotype. Three months after grafting, almost 90% of the transplanted cells from either population are insulin positive, and function normally as determined by the release of C-peptide17,26. These results indicate that transplantation provides context and unidentified cues that promote islet maturation. Optimized imaging protocols, such as the one described here, for human fetal pancreatic cells will aid in the search to identify factors that modulate and accelerate maturation. Fundamental biochemical exploration of human fetal pancreatic cells and hESC differentiated towards an endocrine lineage at this stage of development is essential for measuring efficiency of maturation.
The following protocol, outlined in Figure 1, provides our current method for the isolation of human fetal pancreatic cells, called ICCs from whole human fetal pancreas and imaging of these cells. This protocol requires an initial preparation of cells from tissue, which can be subsequently grown as a monolayer or in suspension. Preparation of cells for imaging of commonly used markers of endocrine cell proliferation and maturation is described.
Generation and imaging of ICCs in the absence or presence of a variety of chemical modifying agents provides a rapid method, compared with transplantation models, to help identify culture conditions and compounds that accelerate maturation of human fetal pancreatic cells into fully functional exocrine, ductal, or hormone producing pancreatic cells.
Protocol
Notes before getting started:
- Human fetal pancreata were obtained from the Birth Defects Research Laboratory, University of Washington (Seattle, Washington, USA) who harvested the tissue. Informed consent for tissue donation, storage, and use of the samples was obtained from the donors by the center. The protocol consent statement was provided in writing and The University of California, San Diego Human Research Protections Program approved the whole study (Protocol #081237XT).
- It is essential to maintain both the human fetal pancreas and the container holding the pancreas on ice during the entire procedure. The dissociation and digestion should be performed as fast as possible.
- Send the clinic where the human fetal pancreas was obtained from the buffer for storage and transport of the pancreas. (RPMI-1640 + 10% normal human serum (NHS), 300 mM trehalose SG, penicillin/streptomycin, and fungizone).
1. Dissection of Human Fetal Pancreas
- Dissolve 5 mg of RT collagenase XI in HBSS to give a final concentration of 2.5 mg/ml. Filter sterilize the solution with a 0.22 micron syringe filter into a sterile (autoclaved) scintillation vial and store at 4 °C. In a tissue culture hood, set out 2 sterile Petri dishes, a sterile small crucible (if a crucible is unavailable, a small beaker may be substituted), sterilized scissors, and forceps. Add 2 ml HBSS to one Petri dish to wash the pancreas. Aspirate liquid from the tube containing the fetal pancreas, leaving approximately 1 ml.
- Remove the pancreas with forceps into the 60 mm Petri dish without HBSS. For these experiments, fetal ICCs are generated from fresh pancreata with gestational ages ranging from 9 to 23 weeks. Isolation from pancreata at earlier gestionational ages is difficult due to the size of the pancreas. The protocol is likely applicable to gestational ages beyond 23 weeks, however acquisition of pancreata after this time is difficult because of federal (U.S.) restrictions. Occasionally, the fetal pancreas arrives with splenic, fat, or connective tissue attached from the original dissection. The extra tissue is easily visible to the naked eye and should be removed from the pancreas before starting the protocol.
- Rinse the pancreas in a minimal volume of cold HBSS (~0.5 ml) in the Petri dish.
- Move the cleaned pancreas to the small sterile crucible using sterile forceps and place in an ice bucket. Place the crucible in a holder for a 50 ml centrifuge tube and, using 2 pairs of scissors, vigorously slice the pancreas for several minutes. (Usually 2-5 min, but the time depends on the size and firmness of the tissue). Cutting technique is important. Hold one side of the scissors in a fixed position moving only the opposite handles. The tips of the scissors should rest on the bottom of the crucible. Continue with rapid scissor motion to break the pancreas into small pieces. The smaller the pieces of tissue, the better the collagenase will work.
- Add 1.5 ml of HBSS + the chopped up pancreas to the vial containing the collagenase and place in a water bath shaker set to 37 °C at 200 rpm for up to 10 min. Do not check more frequently than once during the first 5 min. Digestion time depends on the tissue quality, as little as 6 min may be sufficient. The end point is when the particles are small and uniform.
- Fill the vial (10-15 ml) with cold HBSS to stop the collagenase activity. Place on ice and allow the clumps to settle for 10 min. Often at this point, some cell death has occurred and DNA is released into the media. This can make the media ‘stringy’; in this case, add 100 µl DNase (10 mg/ml stock) to the solution.
- After the tissue in the scintillation vial has settled for 10 min, aspirate off the top layer leaving it slightly less than half full (7-8 ml). Transfer the cells to a 15 ml conical tube, add 5 ml HBSS. Centrifuge for 5 min at 300 x g.
- Aspirate the HBSS and resuspend the cells in 5 ml media containing RPMI-1640, glutamax, 10% normal human serum (NHS), 10 mM HEPES pH 7.2, penicillin/streptomycin, and fungizone. Plate on 60 mm Petri dish. For researchers trying to generate β cells, add HGF (10 ng/ml final) to the media. Additionally, a number of groups have demonstrated that supplementing the culture media with the incretin hormone GLP-1 also increases β cells28. Cells should be left in suspension for 72 hr to aggregate and form ICCs.
- After 72 hr in suspension, cells can be plated on the matrix of the human cell line HTB9 matrix as described previously29. Regardless of growth conditions, the media should be changed every 48 hr.
2. Immunofluorescence of Markers of Endocrine Cell Proliferation and Maturation in ICCs Grown in Suspension, Monolayer, or on Glass Coverslips
- To measure cell proliferation, BrdU labeling of either adherent cells or cells in suspension is performed for 12 hr prior to PFA fixation. BrdU reagent is diluted 1:100 and filter sterilized in RPMI-1640, glutamax, 10% NHS, 10 mM HEPES pH 7.0, penicillin/streptomycin, and fungizone.
- For cells in suspension: Centrifuge for 5 min at 300 x g and aspirate culture medium. Add 10 ml PBS to wash the ICCs, centrifuge for 5 min at 300 x g and aspirate. If the ICCs are going to be embedded in paraffin, please follow optional protocol 3.1-3.17. For adherent cells: Remove culture medium and wash cells with PBS as described above. Fix cells for 20 min with 4% PFA at RT, then wash twice with PBS. At this point, the plates can be wrapped with Parafilm and stored in PBS at 4 °C for up to 1 week.
- Incubate the cells with 0.2% Triton-X 100 in PBS for 10 min at RT. Wash the cells twice with PBS and apply Blocking Buffer (2% donkey serum, 2% bovine serum albumin, 50 mM glycine diluted in PBS) for 1 hr. Wash the cells with Working Buffer (Blocking Buffer diluted 1:10). Dilute the antibody in working buffer. For cells grown on glass coverslips, dilute the antibody in 60 μl total volume. For cells in a 6-well dish, dilute the antibody in 600 µl total volume. To stain multiple epitopes, a cocktail of antibodies may be applied. As a control, use IgG or pre immune serum in place of the specific antibody. Control samples must be incubated with control IgG from the same species as the primary antibody being used.
- Incubate the primary antibody either 1.5 hr at RT or O/N at 4 °C. Aspirate the primary antibody and wash 3x with Working Buffer at RT.
- Dilute the secondary antibody at 1:200 for Rhodamine and FITC conjugated antibodies, 1:500 – 1:1,000 for the Alexa conjugated antibodies. It is important to note that all secondary antibodies are light sensitive. Cover the samples in aluminum foil to prevent loss of signal. Incubate for 1 hr at RT.
OPTIONAL: To visualize the nuclei, DAPI can be added at 1:500 during the secondary incubation. This is useful for quantitation of protein expression in the total cell population. - Aspirate the secondary antibody and wash 3x with Working Buffer at RT. For cells grown on a coverslip, gently lift the coverslip with forceps while immersed in the buffer; wash it by immersing in PBS. For cells grown in a 6-well plate, add PBS to wash and aspirate. At this point they are ready to examine under an inverted microscope.
- Touch the edge of the coverslip gently on a Kimwipe to get rid of excess PBS. Add a drop of mounting gel on a glass slide and invert the coverslip onto the slide. Remove excess mounting gel by aspiration. Tap the coverslip gently with the back of a 200 μl pipet tip to remove bubbles.
- Dry at room temperature for about 20 min or O/N at 4 °C and examine under a fluorescent or confocal microscope.
3. (Optional) Immunofluorescent Staining of Proteins from Paraffin Embedded ICCs
- Prepare a 3% agarose solution and let cool to 55-60 °C.
- Transfer the ICCs incubated in suspension to a 15 ml conical tube, and centrifuge at 1,500 x g for 5 min at room temperature.
- Aspirate the media from the cells and fix with 500 μl 4% PFA for 10 min at RT. Do not mix the pellet, unless the pellet is very large.
- Wash the pellet twice with 750 μl PBS. Like the 4% PFA, this waste is considered hazardous and should be disposed of according to your institution's hazardous waste specifications.
- Gently flick the cell pellet to loosen and add 150-200 μl of the agarose down the wall of the 15 ml conical tube.
- Mix by gently flicking the tube, but do not form bubbles.
- Allow to solidify at 4 °C for 5-10 min.
- Use a 21 G needle to dislodge the pellet and place in a fresh 15 ml conical tube.
- Paraffin embedding and the preparation of sections on slides can be done on site using a microtome or by your core microscopy facilities.
- Deparaffinize tissue, hydrate, and wash with water quickly.
- Add 0.2 M glycine for 30 min at RT to quench the remaining aldehyde.
- Wash the slide twice with PBS for 2 min each.
- For antigen retrieval, bring 10 mM Citrate Buffer (pH 6.0) to boil over hot plate. Immerse the slides in the buffer, wait for it to come back to a boil, and wait for 15 min.
- Remove the beaker from the hotplate. Wait approximately 40 min for the slides to cool in the buffer.
- Wash the slides twice with H2O for 5 min each, wash the slides twice with PBS for 5 min each, block with 2% normal donkey serum in PBS for 1 hr.
- Incubate with primary antibody, diluted to correct concentration in Working Buffer containing 0.2% Triton X-100. Generally, the primary antibody is incubated overnight if staining for transcription factors and for 1.5 hr if staining for hormones, markers of proliferation, and/or differentiation.
- Follow steps 2.3-2.9 described above.
Representative Results
Careful preparation of fetal ICCs is critical to the success of this protocol. Representative pictures of how the cells typically look at defined periods after plating are shown in Figure 2. After purification, the freshly plated cell aggregates appear as small, sparse clear clusters that contain few cells (Figure 2A). After the first 24 hr (Figure 2B), many of the cell clusters become larger, but numerous small clusters remain. By 48 hr, the clusters have expanded significantly, but remain asymmetrical (Figure 2C). At 72 hr, the ICCs should be clear, relatively uniform in size and shape (Figure 2D). It is at this point that the cells can be either plated on matrices, such as HTB-9, for 24 hr prior to immunofluorescence or allowed to grow for another 72 hr in the absence or presence of chemicals or drugs that may alter expression of genes required for pancreatic endocrine cell generation. Figure 3 highlights a number of commonly used antibodies to assess either ICC proliferation or differentiation towards pancreatic endoderm. In Figure 3A, ICCs were plated on HTB-9, grown for 4 days, and stained for PDX1, a critical marker of pancreatic development. Although in vitro staining of ICCs is performed routinely in our laboratory, more often, human fetal ICCs are transplanted under the kidney capsule of nude mice and allowed to proliferate and differentiate in vivo6,9,30-32. At specified times after transplantation, mice are sacrificed and the kidney containing the transplanted ICCs is removed, fixed in 4% paraformaldehyde, and embedded in paraffin. Sequential 5-μm sections are generated either on site using a microtome or by a core microscopy facility. Epitope unmasking and staining of proteins from paraffin embedded tissue for immunofluorescent microscopy is described in optional protocol 3.10-3.17. In Figure 3B, transplanted ICCs were stained with the epithelial cell marker pan cytokeratin (PanCK; green) and with Ki67 (red) to assess cell proliferation. In another example, both human insulin (green) and glucagon (red) were detected after transplantation and maturation under the kidney capsule of a nude mouse (Figure 3C).
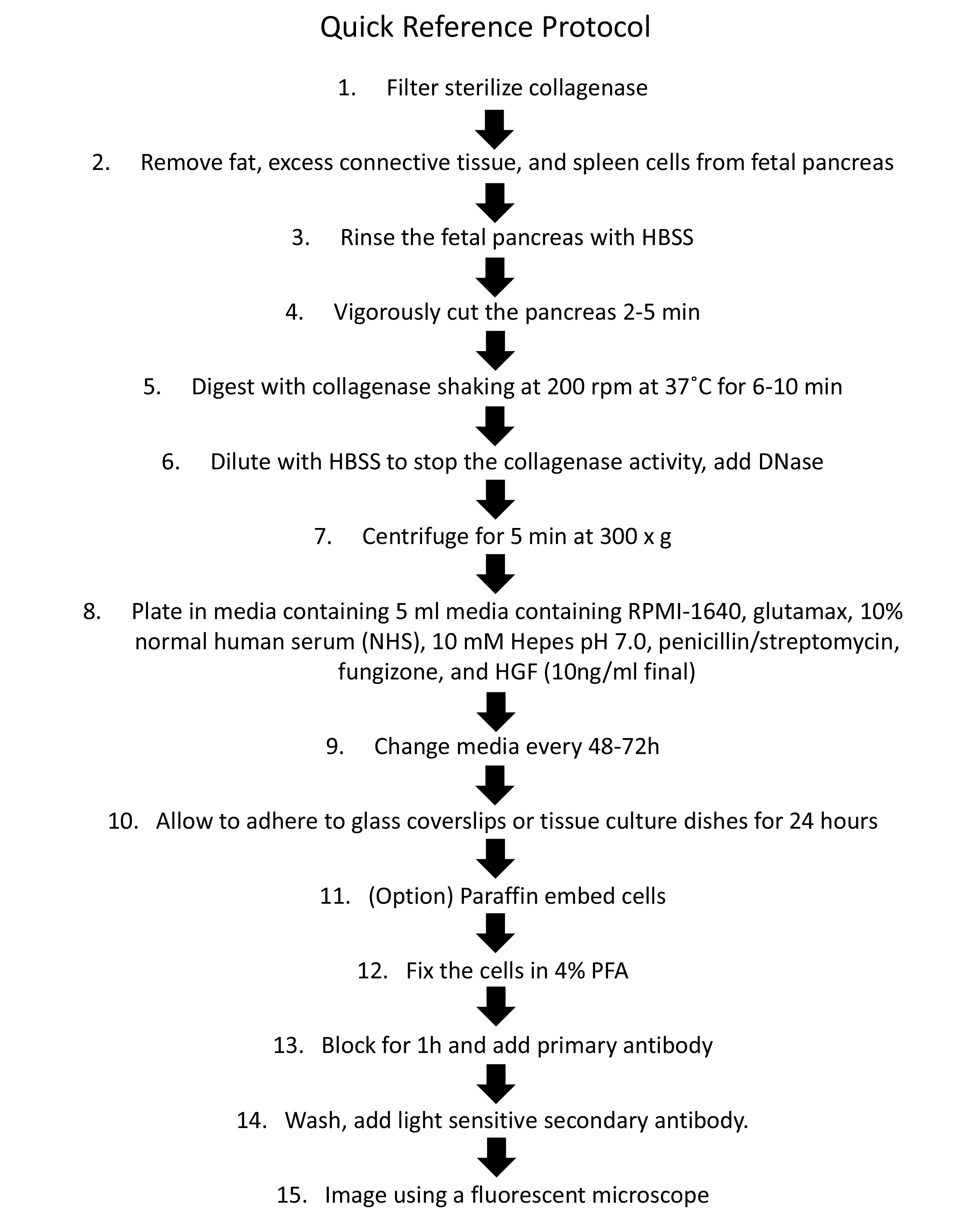
Figure 1. Flow chart of human fetal ICC preparation and staining for Immunofluorescence.

Figure 2. Representative fetal ICCs preparation at 0, 24, 48, or 72 hr after plating. (A) ICCs in suspension were imaged immediately after plating, (B) 24 hr after plating, (C) 48 hr after plating, or (D) 72 hr after plating. Scale bar for A-C, 10X magnification = 300 µm, scale bar for D, 20 magnification = 100 µm. Please click here to view a larger version of this figure.
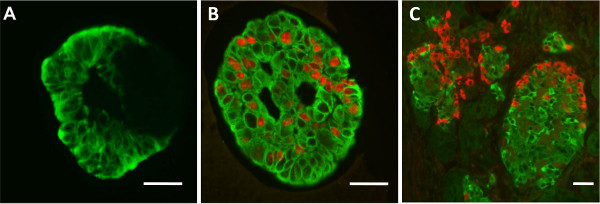
Figure 3. Immunofluorescence of plated ICCs. Routinely, ICCs are imaged for (A) the pancreatic endoderm marker PDX1 (green), (B) endocrine cells (pan-CK; green) and proliferation (Ki67; red), (C) insulin (green) and glucagon (red). Scale bar for A-C, 40X magnification = 20 μm.
Discussion
The methods presented here enable one to generate ICCs from human fetal pancreas and subsequently image for markers of cell proliferation and pancreatic endoderm. The process of human fetal pancreas dissociation required about 90 min, followed by a 72 hr ICC formation period, an approach that is substantially different from protocols to isolate β cell progenitor cells from mouse. The protocol presented here provides a reproducible method that allows the researcher to explore human fetal pancreatic development. Two different types of longitudinal studies can be performed. First, the potential to generate functional pancreatic cell types (ductal cells, exocrine cells, and hormone positive cells) from different gestational ages can be assessed after transplantation. Second, ICCs from a single gestational age can be grown in culture, treated with selected pharmacological agents and transplanted at different time points during ICC culture to explore differences in cell fate. With the tremendous efforts currently being directed at hESC differentiation into insulin producing cells, the problems associated with insulin secretion in response to physiological stimuli are again being revived. Human ICCs provide a unique model system to study this critical aspect of fetal pancreas cell proliferation and β cell development.
As with any protocol to isolate cells from tissues, details are critical for success. A number of parameters are unfortunately outside of the control of the laboratory personnel performing the experiment. Two problems encountered by this laboratory include poor quality of starting material and delivery of non-pancreatic tissue. Healthy fetal pancreatic tissue is firm to a scissor cut. If the tissue cuts too easily, it is a sign that the pancreatic enzymes have begun to digest the pancreas itself. From this there is unfortunately no recovery and the preparation is best cancelled. Infrequently, an inexperienced technician removing the pancreas will confuse sections of the gut for the pancreas. These samples will have much more elasticity than a pancreas and a notable lumen will be present. Again, these samples should be discarded.
When the protocol above is followed as described, there are rarely any issues that arise to throw the isolation off track. A few points to remember to ensure a smooth isolation include, to use sharp scissors for precise pancreas cutting and to make sure to not leave any tissue sample too big to digest. If the cuts are not small enough, then the collagenase does not work effectively, and few ICCs are formed. Conversely, when using a new batch of collagenase, start with a similar level if IU (international units) for digestion as previously used. However, decrease the incubation time to ensure that over digestion does not occur. This troubleshooting technique ensures that the IU label does not vary significantly from batch to batch.
Taken in perspective, this technique for isolation of human fetal ICCs is relatively standard in the field. Most laboratories confirmed our findings that addition of HGF to the media helps the cells survive and proliferate33. In summary, we have developed a method to isolate human fetal ICCs fresh pancreata with gestational ages ranging from 9 to 23 weeks. The cells can be grown as a monolayer or in suspension for experiments to visualize pancreatic endocrine transcription factors and human insulin.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This work was supported by the California Institute for Regenerative Medicine (RB3-02266) and the NIH (DK54441).
Materials
| Trehalose SG | Hayashibara | Trehalose SG | |
| Collagenase XI | Sigma | C-9407 | |
| Hank’s Balanced Salt Solution (HBSS) | Life Technologies | 24020-117 | |
| RPMI 1640 with glutamate | Life Technologies | 11879020 | no glucose or HEPES |
| Human AB Sera, Male Donors | Omega Scientific | HS-30 | |
| Fungizone | Life Technologies | 15290018 | |
| Gentamicin Solution 50 mg/ml | Invitrogen | 15750060 | |
| 1M Hepes, pH 7.0 | Life Technologies | 15630080 | |
| Penicillin – Streptomycin 100X Solution | Life Technologies | 15070063 | |
| Glutamax | Life Technologies | 35050061 | |
| Hepatocyte Growth Factor (HGF) | Peprotech | 100-39 | |
| GLP-1 | Peprotech | 130-08 | |
| Fetal Bovine Serum | Invitrogen | 16000-044 | |
| Dnase | Sigma | DN25 | |
| Sterile Petri Dishes, 60 x 15 mm; Stackable, venting ribs | Spectrum Laboratory Products, Inc. | D210-13 | |
| PBS | Gibco | 14190 | |
| 16% PFA | Electron Microscopy Sciences | 15710 | |
| Triton X-100 | Sigma | T9284 | |
| Donkey Serum | Jackson ImmunoResearch | 017-000-121 | |
| BrdU | Life Technologies | 00-0103 | |
| anti-insulin (mouse monclonal; 1:1000) | Sigma | I2018 | |
| anti-glucagon (mouse monoclonal; 1:2000) | Sigma | G2654 | |
| PDX1 (mouse monoclonal) | Novus Biologicals | NBP1-47910 | |
| PDX1 (goat polyclonal) | AbCam | 47383 | |
| PDX1 (rabbit polyclonal) | AbCam | 47267 | |
| AlexaFluor 546 (rabbit) | Invitrogen | A11010 | |
| AlexaFluor 546 (mouse) | Invitrogen | A11003 | |
| AlexaFluor 488 (rabbit) | Invitrogen | A11008 | |
| AlexaFluor 488 (mouse) | Invitrogen | A11001 | |
| Ki67 | Lab Vision Neomarkers | RM 9016-50 | |
| pan-CK (mouse monoclonal; 1:100) | Immunotech | 2128 | |
| CK19 | AbD Serotech | MCA 2145 | |
| DAPI | Cell Signaling | 4083 | |
| HTB9 cell line | ATCC | 5637 | see Beattie 1997 reference to generate matrix |
| Agarose | Sigma | A-6013 |
References
- Tuch, B. E., Ng, A. B. P., Jones, A., Turtle, J. R. Histologic differentiation of human fetal pancreatic explants transplanted into nude mice. Diabetes. 33, 1180-1187 (1984).
- Tuch, B. E., Grigoriou, S., Turtle, J. R. Growth and hormonal content of human fetal pancreas passaged in athymic mice. Diabetes. 35, 464-469 (1986).
- Hullett, D. A., Falany, J. L., Love, R. B., Butler, J. A., Sollinger, H. W. Human fetal pancreas: Potential for transplantation. Transplantation Proceedings. XIX (1), 909-910 (1987).
- Hullett, D. A., Bethke, K. P., Landry, A. S., Leonard, D. K., Sollinger, H. W. Successful long-term cryopreservation and transplantation of human fetal pancreas. Diabetes. 38, 448-453 (1989).
- Tuch, B. E. Reversal of diabetes by human fetal pancreas. Transplantation. 51, 557-562 (1991).
- Beattie, G. M., Lopez, A. D., Otonkoski, T., Hayek, A. Transplantation of human fetal pancreas: fresh vs. cultured fetal islets or ICCS. J Mol Med. 77, 70-73 (1999).
- Joglekar, M. V., et al. The miR-30 family microRNAs confer epithelial phenotype to human pancreatic cells. Islets. 1, 137-147 (2009).
- Joglekar, M. V., Joglekar, V. M., Joglekar, S. V., Hardikar, A. A. Human fetal pancreatic insulin-producing cells proliferate in vitro. J Endocrinol. 201, 27-36 (2009).
- Kayali, A. G., et al. The SDF-1alpha/CXCR4 Axis is Required for Proliferation and Maturation of Human Fetal Pancreatic Endocrine Progenitor Cells. PLoS One. 7, (2012).
- Otonkoski, T., et al. Hepatocyte growth factor/scatter factor has insulinotropic activity in human fetal pancreatic cells. Diabetes. 43, 947-953 (1994).
- D’Amour, K. A., et al. Production of pancreatic hormone-expressing endocrine cells from human embryonic stem cells. Nat Biotechnol. 24, 1392-1401 (2006).
- Xu, X., et al. Endoderm and pancreatic islet lineage differentiation from human embryonic stem cells. Cloning Stem Cells. 8, 96-107 (2006).
- Jiang, J., et al. Generation of insulin-producing islet-like clusters from human embryonic stem cells. Stem Cells. 25, 1940-1953 (2007).
- Shim, J. H., et al. Directed differentiation of human embryonic stem cells towards a pancreatic cell fate. Diabetologia. 50, 1228-1238 (2007).
- Kroon, E., et al. Pancreatic endoderm derived from human embryonic stem cells generates glucose-responsive insulin-secreting cells in vivo. Nat Biotechnol. 26, 443-452 (2008).
- Van Hoof, D., D’Amour, K. A., German, M. S. Derivation of insulin-producing cells from human embryonic stem cells. Stem Cell Res. 3, 73-87 (2009).
- Schulz, T. C., et al. A scalable system for production of functional pancreatic progenitors from human embryonic stem cells. PLoS One. 7, (2012).
- Lees, J. G., Tuch, B. E. Conversion of embryonic stem cells into pancreatic beta-cell surrogates guided by ontogeny. Regen Med. 1, 327-336 (2006).
- Rezania, A., et al. Maturation of human embryonic stem cell-derived pancreatic progenitors into functional islets capable of treating pre-existing diabetes in mice. Diabetes. 61, 2016-2029 (2012).
- Bai, L., Meredith, G., Tuch, B. E. Glucagon-like peptide-1 enhances production of insulin in insulin-producing cells derived from mouse embryonic stem cells. J Endocrinol. 186, 343-352 (2005).
- Semb, H. Definitive endoderm: a key step in coaxing human embryonic stem cells into transplantable beta-cells. Biochem Soc Trans. 36, 272-275 (2008).
- Van Hoof, D., Mendelsohn, A. D., Seerke, R., Desai, T. A., German, M. S. Differentiation of human embryonic stem cells into pancreatic endoderm in patterned size-controlled clusters. Stem Cell Res. 6, 276-285 (2011).
- Beattie, G. M., Otonkoski, T., Lopez, A. D., Hayek, A. Maturation and function of human fetal pancreatic cells after cryopreservation. Transplantation. 56, 1340-1343 (1993).
- Sandler, S., et al. Tissue culture of human fetal pancreas. Effects of nicotinamide on insulin production and formation of isletlike cell clusters. Diabetes. 38 Suppl 1, 168-171 (1989).
- Otonkoski, T., Beattie, G. M., Cirulli, V., Mally, M. I., Hayek, A., Sharvetnick, N., Landes, R. G. . Pancreatic regeneration. , (1997).
- Otonkoski, T., Beattie, G. M., Mally, M. I., Ricordi, C., Hayek, A. Nicotinamide is a potent inducer of endocrine differentiation in cultured human fetal pancreatic cells. J Clin Invest. 92, 1459-1466 (1993).
- Xie, R., et al. Dynamic chromatin remodeling mediated by polycomb proteins orchestrates pancreatic differentiation of human embryonic stem cells. Cell Stem Cell. 12, 224-237 (2013).
- Hardikar, A. A., et al. Functional maturation of fetal porcine beta-cells by glucagon-like peptide 1 and cholecystokinin. Endocrinology. 143, 3505-3514 (2002).
- Beattie, G. M., Cirulli, V., Lopez, A. D., Hayek, A. Ex vivo expansion of human pancreatic endocrine cells. J Clin Endocrinol Metab. 82, 1852-1856 (1997).
- Beattie, G. M., et al. Trehalose: a cryoprotectant that enhances recovery and preserves function of human pancreatic islets after long-term storage. Diabetes. 46, 519-523 (1997).
- Hayek, A., Beattie, G. M. Experimental transplantation of human fetal and adult pancreatic islets. J Clin Endocrinol Metab. 82, 2471-2475 (1997).
- Otonkoski, T., Beattie, G. M., Lopez, A. D., Hayek, A. Use of hepatocyte growth factor/scatter factor to increase transplantable human fetal islet cell mass. Transplant. Proc. 26, 33-34 (1994).
- Beattie, G. M., et al. A novel approach to increase human islet cell mass while preserving beta-cell function. Diabetes. 51, 3435-3439 (2002).

