Portable Thermographic Screening for Detection of Acute Wallenberg’s Syndrome
Summary
Acute Wallenberg's syndrome can be misdiagnosed as a non-stroke disease, such as auditory vertigo. Thus, careful neurological examination, which is sometimes difficult for non-neurologists, is necessary for precise diagnosis. Here, we present a simple, rapid, noninvasive, and cost-effective method for detection of acute Wallenberg's syndrome using portable thermography.
Abstract
Wallenberg's syndrome (WS) is a type of brainstem infarction. WS patients often show Horner's syndrome, dissociated sensory disturbance, truncal ataxia, and hoarseness. However, they rarely show tactile sensory disturbance and paralysis of the extremities. Additionally, acute brainstem infarction is often not apparent in magnetic resonance images. These symptomatic and imaging characteristics sometimes lead to misdiagnosis of WS as a non-stroke disease, including auditory vertigo. Although careful neurological examination is necessary to prevent misdiagnosis of WS, this type of examination may be difficult for non-neurologists to whom affected patients initially present. Lateral differences in body surface temperature (BST) constitute a recognized and widespread symptom of WS. We previously reported that most acute WS patients exhibit lateral differences in BST at multiple locations and that these lateral differences in BST could easily be detected by thermographic measurement. Here, we present the method for use of portable thermography to detect acute WS, using a simple, rapid, noninvasive, and cost-effective approach. To assess lateral differences in BST among patients with suspected WS, BST was measured as soon as possible in the examination room or in the patient's bedroom. Measurements were performed bilaterally at four locations where images could easily be acquired (face, palm of the hand, abdomen, and dorsum of the foot) using a portable thermal camera. When lateral differences in BST are observed macroscopically, especially in multiple locations on the same side, a diagnosis of WS should be suspected. Macroscopic assessment of BST laterality can be made within 2 min of the acquisition of thermographic images. This method may be useful in preventing misdiagnosis of acute WS as a non-stroke disease, especially when such patients initially present to non-neurologists.
Introduction
Wallenberg's syndrome (WS) is a type of brainstem infarction. Acute WS patients are sometimes initially misdiagnosed with non-stroke diseases because of the symptomatic and magnetic resonance imaging (MRI) characteristics of WS. To accurately diagnose acute WS, careful neurological examination is necessary, which may be difficult for non-neurologists to whom affected patients initially present. Here, we present a simple, rapid, noninvasive, and cost-effective method for the detection of acute WS using portable thermography.
WS is caused by the infarction of a wedge of the dorsal lateral medulla oblongata, due to occlusion of the vertebral artery or posterior inferior cerebellar artery1,2. WS may be misdiagnosed as a non-stroke disease because of a combination of unique symptomatic and MRI characteristics that contrast with those typically observed in cerebral infarction. Hemiparesis and tactile sensory disturbance, which tend to be observed in patients with other types of cerebral infarction, are rare in WS patients; however, they exhibit various combinations of clinical symptoms, including hoarseness and dysphagia, dissociated sensory disturbance, vertigo, gaze-induced nystagmus, ataxia, and Horner's syndrome1,2,3,4,5,6,7,. Another unique characteristic of WS patients is the limited severity of symptoms, which is similar to that in other types of brainstem infarctions7,8,9,10,11. Some patients with brainstem infarctions have arrived at the outpatient clinic on foot and reported only minor complaints7. In some patients with WS, vertigo is the only presenting symptom, and it can therefore be difficult to differentiate between WS and auditory vertigo12. Furthermore, WS can affect young patients, due to its potential etiology of artery dissection2. MRI analysis of brainstem infarction, including WS, is unique in that the high-intensity diffusion-weighted imaging signal may be delayed in some patients7,13,14.
The above characteristics are thought to cause misdiagnosis of WS. Dysphagia may cause aspiration pneumonia or asphyxia, and artery dissection may cause subarachnoid hemorrhage15; therefore, overlooking WS may result in the development of life-threatening conditions for the patient. Although careful neurological examination is necessary to prevent the misdiagnosis of WS, it is likely that a patient will first present to a non-neurologist. Therefore, a rapid and simple method for screening of acute WS may be clinically useful.
Previously, we reported that 89% of acute WS patients exhibit laterality of BST, which is presumed to result from disturbance of the central autonomic nervous tract due to infarction at the lateral medulla7. Because this autonomic nervous tract descends from the lateral brainstem (including the ventro-lateral medulla) and contains the connective pathway of sweating and skin blood flow16, disturbance of sweating and vasoconstriction lead to increased BST on the ipsilateral side of WS. In the prior report, we also showed that the laterality of BST can be easily detected within 2 min using thermographic measurement in most patients with WS7,17. Here, we report a method for the detection of laterality of BST using thermography, which may be useful in preventing misdiagnosis of acute WS.
Protocol
All methods described here were approved by the Human Research Ethics Committee Institutional Review Board of Kanto Central Hospital.
NOTE: We used a commercially available portable thermal camera and dedicated software (see the Table of Materials), and have constructed our protocols based on the use of these specific instruments.
1. Preparation for Measurements
- Charge the thermal camera before use.
- Turn on the camera.
- Push the center button on the camera to display the menu. Select Color from the menu and select Iron or Rainbow color.
- Push the center button on the camera to display the menu. Select Measurement and then Center spot measurement to measure the BST in real time.
2. Patient Selection
- Test all patients with suspected WS. Patients with dizziness, vertigo, ptosis, hoarseness, dysphagia, anisocoria, or dissociated sensory disturbance may have WS.
- Subjectively determine the laterality of BST by palpating the patient with suspected WS.
3. Acquisition of Thermographic Images
- Instruct the patient to take off their socks and shoes. Have the patient remove clothing (if consent is granted) to enable examination of the abdominal region.
- Acquire images in an examination room or in the patient's bedroom, as soon as WS is suspected. Ask the patient to assume a supine posture or sitting position during image acquisition. Ask the photographer to stand 50-100 cm from the patient.
NOTE: Lighting conditions in the room do not influence the results of the thermographic measurements. - Acquire one image at each of four areas for each patient: 1) frontal face, 2) bilateral palm, 3) abdomen, and 4) bilateral dorsum of the foot (Figure 1). These four areas are uncomplicated locations for image acquisition, even in bedridden patients who cannot move because of dizziness, vertigo, nausea and vomiting.
NOTE: Blankets or drafts caused by air conditioning may influence the BST. If such influence is suspected, cover all extremities and the trunk with blankets, then acquire additional images after an interval of >10 min. Drip infusion therapy at the extremities also may influence the BST. If possible, slow down or stop the infusion, then acquire images after an interval of >10 min.
4. Assessing the Laterality of BST
- Consider BST to exhibit laterality when the BST between the right and left sides is markedly different macroscopically and the degree of laterality is >0.5 °C18. If the laterality of BST is not obvious or appears to be ≤0.5 °C, perform advanced analysis with dedicated software as described below.
NOTE: When laterality of BST is observed in multiple locations on the same side of the patient, there is a strong possibility that the patient has WS in the ipsilateral side of the medulla on the warmer side, as determined by BST.
5. Advanced Assessment of the Laterality of BST
- Initialize the thermal imaging and analysis software.
- Select and open the acquired image to be analyzed.
- Select the Ellipse measurement button on the left side tab, and indicate ellipses with diameters of >5 mm at four locations: 1) the nasolabial fold on the face; 2) the palm of the hand; 3) thoracic spine levels 8-10, approximately 5 cm from the umbilicus of the torso; and 4) the center of the dorsum of the foot.
- Check the average BST from each location and compare it to the BST on the contralateral side of the body.
6. Confirming WS
- Perform a careful neurological examination if the patient exhibits laterality of BST to confirm a diagnosis of WS. In addition to screening by neurological examination, check for the presence of Horner's syndrome including ptosis and constricted pupil, as well as the presence of dissociated sensory disturbance, to determine whether the patient exhibits acute WS.
- Consider hospital admission when WS cannot be ruled out based on the results of thermographic measurement and neurological examination.
- Consider repeated thin-slice brainstem MRI after an interval of a few days to diagnose WS.
Representative Results
Acquisition of thermographic images and macroscopic assessment to determine whether BST exhibits laterality may be performed within 2 min in most patients. Most acute WS patients exhibit laterality of BST at multiple locations. Some patients exhibit laterality of BST throughout the body (Figure 2A), whereas some exhibit laterality only in a few locations (Figure 2B). The warmer side, as determined by BST, is ipsilateral to the location of WS (Figure 2D,E). Importantly, however, a WS patient with a very small infarction may not exhibit laterality of BST (Figure 2C,F). When a patient does not exhibit a central nervous disorder (e.g., auditory vertigo), laterality of BST is typically not observed (Figure 1). However, when a patient exhibits vascular stenosis, BST may be lower in the extremities with vascular stenosis than in extremities on the contralateral side. Laterality of BST is observed in only one limb in nearly all patients with vascular stenosis. However, patients may exhibit vascular stenosis in both the upper and lower limbs (Figure 3).
The precise degree of BST can be analyzed with dedicated software (Figure 4). This analysis may be required when the laterality of BST is not apparent macroscopically, especially on the face and trunk, because lateral differences in the faces and trunks of WS patients tend to be smaller than those of the extremities in such patients7.
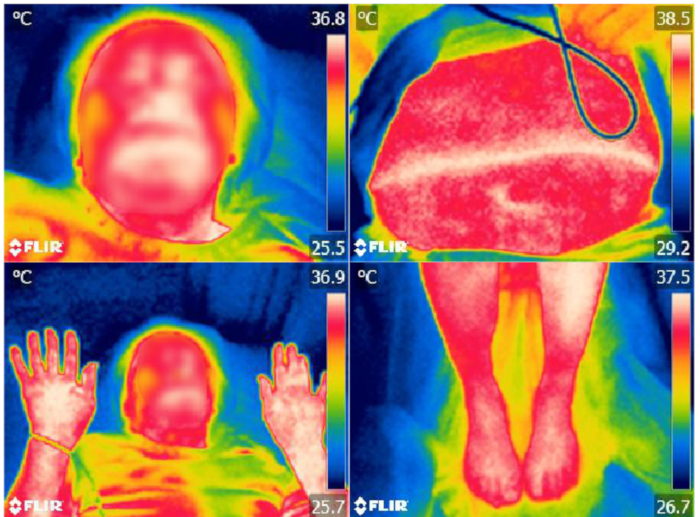
Figure 1: Thermographic images of the face, bilateral palm, abdomen, and bilateral foot of a patient with auditory vertigo. Laterality of BST is not detected. The patient's face is blurred to protect privacy. Please click here to view a larger version of this figure.
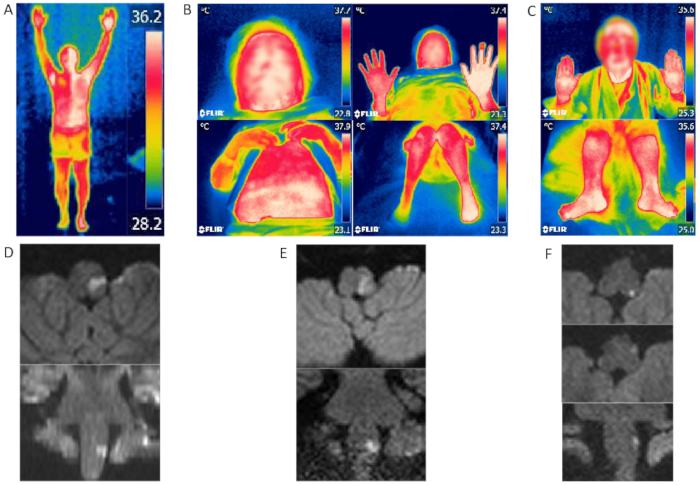
Figure 2: Thermographic images and MRI findings of WS patients. (A, D) WS patient with laterality of BST throughout the body. The warmer side of the patient's body is ipsilateral to the infarction. (B, E) WS patient with laterality of BST of the upper and lower limbs. The warmer side is also ipsilateral to the infarction. (C, F) Brain MRI/diffusion-weighted imaging of this patient revealed a very small high-intensity lesion at the edge of the lateral medulla, but no lateral difference in BST. Patients' faces are blurred to protect privacy. Figure 2B-F were modified from Takahashi et al.7. Please click here to view a larger version of this figure.
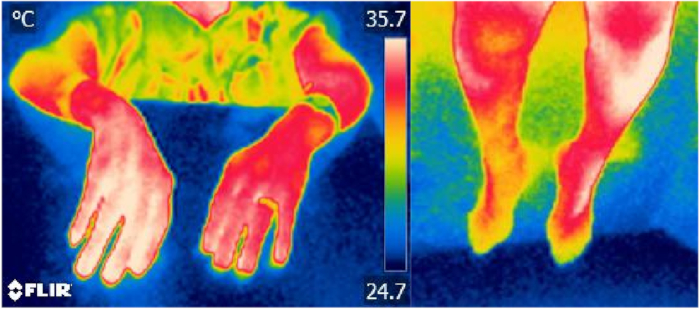
Figure 3: Left upper and right lower extremities of a patient with arterial sclerosis and vascular stenosis. Arterial sclerosis and vascular sclerosis diagnoses were based on ankle-brachial index; thermography reveals higher BST on the contralateral side. Please click here to view a larger version of this figure.
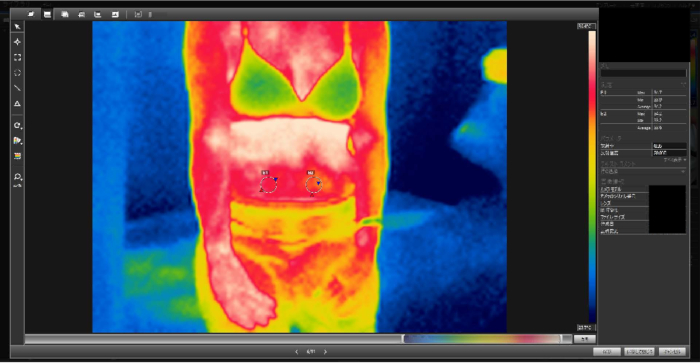
Figure 4: Laterality of BST in the abdomen of a WS patient. Results were equivocal macroscopically, but analysis by ellipse measurement in the analysis software showed a 0.6 °C discrepancy in the average BST between the right and left sides of the abdomen. Please click here to view a larger version of this figure.
Discussion
Critical steps of this protocol are the establishment the initial suspicion of WS and the decision to acquire thermographic images of the patient. Acquiring thermographic images and assessing the laterality of BST is a simple approach, even for non-neurologists who may examine patients upon initial presentation to the emergency department or a general clinic. If a patient exhibits laterality of BST, especially at multiple locations on the same side, the physician should consider the possibility of WS. Because most WS patients with laterality of BST also exhibit other clinical symptoms, including Horner's syndrome and dissociated sensory disturbance7, the physician should then perform a careful neurological examination or consult a neurologist. This protocol may reduce the possibility of overlooking WS.
A limitation of this method is that it cannot be used to confirm a diagnosis of WS-it should only be used when WS is suspected. To confirm a diagnosis of WS, neurological examination and MRI are needed. However, if WS is suspected by a primary physician, this protocol reduces the possibility that the patient will be allowed to go home, thereby reducing the likelihood of misdiagnosis of WS. Other central nervous diseases can result in laterality of BST6; these include other types of brainstem infarctions, as well as supratentorial brain infarction, which may impair the autonomic nervous tract. However, these diseases can be diagnosed easily without thermography because of the high prevalence of hemiparesis and tactile sensory disturbance that are readily observed by physicians who evaluate such patients at the time of initial presentation. Vascular stenosis of the extremities can also result in the laterality of BST19. When a patient exhibits >19% laterality on branch-ankle pulse wave velocity20, the patient may have vascular stenosis, which can affect BST. To rule out these diseases other than WS and to confirm the diagnosis of WS, repeated brain MRI7,13,14, ankle-brachial index20, and contrast enhancement computed tomography are sometimes necessary.
Another limitation is that the characteristics of the thermal camera we used do not fulfill the equipment recommendation of the thermography guidelines from the International Academy of Clinical Thermography21. However, the thermography characteristic assessed in this study was the ability to distinguish the laterality of BST by >0.5 °C. Because the camera can distinguish differences in BST of ≥0.1 °C, the characteristics of our camera may not influence the results of this method.
The degree of lateral discrepancy of BST in most WS patients is greatest at the foot region7; thus, manual assessment of the laterality of BST by palpation of the lower extremities may be an alternative method to this protocol when thermography cannot be used. However, thermographic measurement is superior to palpation because thermographic measurement offers greater objectivity.
The most important merits of this method are that thermographic measurement is rapid, simple, noninvasive, and cost-effective. Although the sensitivity and specificity of this method for identifying WS and other diseases, including other central nervous diseases and auditory vertigo, have not yet been proven, thermographic measurement could be used as a triage method for clinicians during evaluation of patients with dizziness or vertigo. Multicenter studies regarding the laterality of BST are warranted for patients with WS, as well as for those with other central nervous diseases or dizziness.
Disclosures
The authors have nothing to disclose.
Acknowledgements
Not applicable
Materials
| FLIR E5 | FLIR Systems | P/N: 63905-0501 | |
| FLIR Tools | FLIR Systems | RRID:SCR_016330 |
References
- Kim, J. S. Pure lateral medullary infarction: Clinical-radiological correlation of 130 acute, consecutive patients. Brain. 126 (8), 1864-1872 (2003).
- Kameda, W., et al. Lateral and medial medullary infarction: a comparative analysis of 214 patients. Stroke. 35 (3), 694-699 (2004).
- Nowak, D. A., Topka, H. R. The clinical variability of Wallenberg’s syndrome: the anatomical correlate of ipsilateral axial lateropulsion. Journal of Neurology. 253 (4), 507-511 (2006).
- Ogawa, K., Suzuki, Y., Oishi, M., Kamei, S. Clinical study of 46 patients with lateral medullary infarction. Journal of Stroke and Cerebrovascular Diseases. 24 (5), 1065-1074 (2015).
- Parathan, K. K., Kannan, R., Chitrambalam, P., Aiyappan, S. K., Deepthi, N. A rare variant of Wallenberg’s syndrome: Opalski syndrome. Journal of Clinical & Diagnostic Research. 8 (7), 8-9 (2014).
- Korpelainen, J. T., Sotaniemi, K. A., Myllylä, Asymmetrical skin temperature in ischemic stroke. Stroke. 26 (9), 1543-1547 (1995).
- Takahashi, M., et al. Utility of thermographic measurements of laterality of body surface temperature to prevent misdiagnosis of acute Wallenberg’s syndrome. Brain and Behavior. 8, (2018).
- Kim, J. S., Lee, J. H., Lee, M. C. Patterns of sensory dysfunction in lateral medullary infarction. Clinical-MRI correlation. Neurology. 49 (6), 1557-1563 (1997).
- Glass, T. A., et al. Outcome at 30 days in the New England Medical Center Posterior Circulation Registry. Archives of Neurology. 59 (3), 369-376 (2002).
- Akhtar, N., et al. Ischaemic posterior circulation stroke in State of Qatar. European Journal of Neurology. 16 (9), 1004-1009 (2009).
- Fitzek, S., et al. Time course of lesion development in patients with acute brain stem infarction and correlation with NIHSS score. European Journal of Radiology. 39 (3), 180-185 (2001).
- Choi, H. S., Park, S. C., Lee, Y. J., Kang, J. W. Lateral medullary infarction presenting with vertigo without other neurological signs. Otolaryngology-Head and Neck Surgery. 147 (6), 1162-1163 (2012).
- Oppenheim, C., et al. False-negative diffusion-weighted MR findings in acute ischemic stroke. American Journal of Neuroradiology. 21 (8), 1434-1440 (2000).
- Tsuyusaki, Y., et al. "Invisible" brain stem infarction at the first day. Journal of Stroke and Cerebrovascular Diseases. 23 (7), 1903-1907 (2014).
- Tiu, C., et al. Vertebral artery dissection: a contemporary perspective. Maedica. 11 (2), 144-149 (2016).
- Low, P. A. . Clinical Autonomic Disorders: Evaluation and Management. , (1997).
- Takahashi, M., et al. Teaching NeuroImages: the half-split man. Neurology. 87 (11), (2016).
- Vardasco, R., Ring, F., Plassmann, P., Jones, C. Thermal symmetry of the upper and lower extremities in healthy subjects. Thermology International. 22 (2), 53-60 (2012).
- Nakazato, Y., Shimazu, K., Tamura, N., Hamaguchi, K. A study of skin surface temperature in patients with unilateral cerebral infarction–with special reference to central autonomic regulation of skin vasomotor response. Clinical Neurology. 35 (7), 758-763 (1995).
- Motobe, K., et al. Cut-off value of the ankle-brachial pressure index at which the accuracy of brachial-ankle pulse wave velocity measurement is diminished. Circulation Journal. 69 (1), 55-60 (2005).
- International Academy of Clinical Thermography. . Thermography Guidelines: Standards and protocols in clinical thermographic imaging. , (2002).

