Intense Pulsed Light for the Treatment of Dry Eye Owing to Meibomian Gland Dysfunction
Instructor Prep
concepts
Student Protocol
All participants were provided both verbal and written informed consent before any study procedure. The protocol of the study was carried out in accordance with the Declaration of Helsinki and was approved by the local Institutional Review Board.
1. Automated Ocular Surface Workup
- Noninvasive break-up time (BUT) and lipid layer thickness (LLT) evaluation
- "Install the "I.C.P." program by SBM Sistemi on the computer connected to the device.
- Apply the device on the slip lamp.
- Open the application and insert the patient’s data.
- Select the exam to be performed in the menu: select NIBUT to measure the noninvasive BUT or Interferometry to evaluate the lipid layer type and thickness grade.
- Instruct the patient to put the chin and forehead in the correct position on the slit lamp with the device, and place the camera of the device in front of patient’s eye at a correct distance (about 1-2 cm).
- Ask the patient to blink twice, and then stare without blinking for as long as possible.
- Keep the instrument still and click the proper button to acquire the video. The system will provide the value of noninvasive BUT (time in s) or LLT (grade from 1 to 7).
Note: These exams are completely noninvasive, and it is not necessary to use any topical anesthetic or vital staining for the acquisitions and measurements. - Repeat the same procedure for the other eye, if required.
- Meibomian gland loss (MGL) assessment
- Install the “I.C.P.” program by SBM Sistemi on the computer connected to the device.
- Open the program and insert patient’s data.
- Select Meibomian gland in the menu of the exams.
- Apply the device on the slip lamp.
- Gently evert the lower eyelid using a cotton swab.
- Acquire an infrared image of the inner part of the lower eyelid in order to obtain a good quality image of the meibomian glands, which appear whitish.
- Draw the margins of the lower eyelid area on the touchscreen and click to fill the area.
Note: The system automatically calculates the percentage of meibomian gland area in relation the total area of the eyelid. In addition, it is possible to use ImageJ software (National Institute of Health; http://imagej.nih.gov/ij) to analyze the images, and measure the MGL value as the percentage of gland loss in relation to the total tarsal area of the eyelid, as previously described16. - Repeat the same procedure for the other eye, if required.
- Tear osmolarity measurement
- Clip the single use test card with a microchip into the top of the pen. The pen confirms when the test card is correctly attached.
- Gently move down the lateral lower eyelid using a cotton swab to create a little space between the eyeball and the eyelid.
- Place the tip of the test card in this space to collect a sample of tear fluid (50 nL) from the inferior lateral meniscus of the tear film. The pen confirms when the tear fluid sample has been properly collected.
Note: It is recommended to collect tear fluid at the outermost area of the eyelid to minimize the risk of corneal injuries. - Dock the pen in the reader unit. The system reader measures and displays on the screen the osmolarity of the tear in mΩ/L.
- Repeat the same procedure for the other eye, if required.
Note: Separate test cards are needed for each eye.
- Subjective symptoms assessment
- Administer the Ocular Surface Disease Index (OSDI) questionnaire.
- Ask the patient the 12 questions of the OSDI questionnaire, and circle the number in the box that best represents each answer.
Note: The patient needs to answer 12 questions and give a score from 0 to 4 to each answer. - Calculate the sum of the scores of each question, and the total number of questions answered.
- Assess the severity of patient’s ocular discomfort symptoms using the specific chart.
- Fitzpatrick skin phototype assessment
- Determine the patient’s Fitzpatrick skin phototype score basing on the color of the patient’s skin and its reaction to sun exposure, as previously described by Fitzpatrick17.
Note: Patient’s Fitzpatrick skin phototype score is necessary to determine the proper treatment parameters for each patient.
- Determine the patient’s Fitzpatrick skin phototype score basing on the color of the patient’s skin and its reaction to sun exposure, as previously described by Fitzpatrick17.
2. Intense Pulsed Light (IPL) treatment
- Seat the patient comfortably in a treatment chair or lying down on a couch in office.
- Press the start button on the LCD touchscreen of the control unit to activate the device.
- Select the treatment for MGD by pressing the proper button on the LCD touchscreen.
- Select the desired treatment energy level using the up and down arrows on the LCD touchscreen and then press on the Tick button to confirm the choice. Six different energy levels can be chosen, ranging from 9 J/cm2 to 13 J/cm2.
Note: Treatment energy level is determined basing on the Fitzpatrick skin phototype grading scale from I to V (grade VI is not suitable for IPL treatment). Darker skins need lower energy levels. - Validate each of the six safety features by pressing the six icon-buttons one by one and then press the Tick button to confirm that the procedure is performed in total safety.
Note: A summary with all the selections made will be displayed on the LCD touchscreen. - Press the Tick button to start the device and wait a few seconds until the device is ready for the treatment.
- Put the eyewear or the eye mask on the patient’s eyes in order to protect eyes from the emitted therapeutic lights.
- Wear safety glasses to protect the eyes from the emitted light (200-1400 nm).
- Apply a thick layer of optical gel over the skin under the lower eyelid, from the edge of the nose up to the temple, in order to conduct the light and help to spread the energy homogeneously.
Note: The gel layer should be at least 1 cm thick. - Take the device handpiece from the central unit and gently push its head in direct contact with the skin of the area to be treated.
- Press the Start button over the handpiece to emit a single treating IPL pulse.
- Apply 5 single IPL pulses distributed along the area, starting from the inner canthus and progressing to the temporal area, trying to be as close as possible to the lower eyelid margin in order to obtain the greatest effect. (Figure 1)
Note: The upper eyelids are not treated directly because of the risk of light penetration through the eyelid with possible light absorption and subsequent structural damage and inflammation of the intraocular pigmented structures (i.e., iris tissue, ciliary body, uveal tissues). - Remove gently the optical gel from the treated skin area.
- Place a warm compress over the eyelids of both eyes for 2-3 min.
- Repeat the same procedure for the other eye, if required.
Note: The total time session lasts only few minutes (about 10 min). Based on the physician’s choice, the meibomian gland of the lower eyelid of both eyes could be manually expressed after IPL treatment using expressor forceps or two cotton swabs.
3. Post-treatment Therapy
- Prescribe topical steroid eye drops 2 times per day for the following 10 days after the first session of IPL.
Note: Patients are encouraged to continue warm compresses and topical lubricants use at least twice daily during the treatment period. - Repeat IPL treatment after 15 and 45 days to complete the starting treatment protocol.
Note: The standard protocol consists of 3 sessions at day 0, day 15 and day 45. Another additional optional session could be performed at day 75, based on the physician and the patient’s preferences. Repeated treatments could be necessary at regular follow-up to maintain the efficacy after the 3 initial sessions (loading-phase), depending on the single clinical case.
4. Post-treatment Assessment
- Examine carefully the patient’ eyes and eyelids at the slit lamp.
- Repeat noninvasive BUT, LLT, meibography and tear osmolarity to evaluate the treatment efficacy.
- Administer the OSDI questionnaire to the patient to evaluate the patient’s symptoms.
- Ask the patient whether he perceived improvements from his baseline ocular discomfort symptoms according to a 5-grade scale: none = 0, trace = 1, mild = 2, moderate = 3, high = 4.
Note: It is recommended to wait at least 15 days after the third session before evaluating the clinical results obtained with the procedure.
Intense Pulsed Light for the Treatment of Dry Eye Owing to Meibomian Gland Dysfunction
Learning Objectives
Nineteen patients (7 males and 12 females, mean age 39.3 ± 7.0 years) (mean ± standard deviation) underwent IPL treatment between September 2016 and June 2017. Fifteen days after the third IPL treatment session, noninvasive BUT significantly increased from 7.6 ± 0.6 s to 9.8 ± 0.7 s (mean ± standard error of the mean) (p = 0.017), and LLT grade significantly improved from 2.3 ± 0.1 to 3.4 ± 0.3 (p = 0.003). No statistically significant changes were found for MGL and tear osmolarity (23.9 ± 3.6% vs 25.4 ± 2.6% and 304.5 ± 2.4 mΩ/L vs 300.6 ± 2.4 mΩ/L, respectively; always p>0.05) (Figure 2). In addition, mean OSDI score did not differ significantly before and after the last treatment session (p>0.05).
Seventeen patients (89.5% of the total) showed an improvement of ocular discomfort symptoms after the treatment (mean grade 2.0 ± 1.2 out of 4). Figure 3 shows the distribution of patients' perceived improvement in symptoms according to the 5-grade scale. The perceived improvement in symptoms was significantly correlated with the improvement of LLT after the treatment (r = 0.476, p = 0.039).
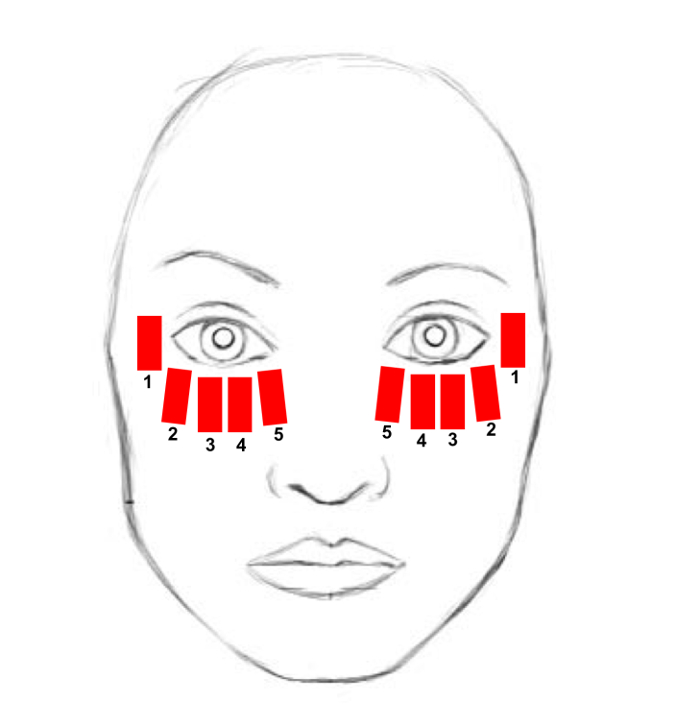
Figure 1. Treatment area. The treatment area includes the lower eyelid, from the inner to the lateral canthus, the cheekbone and the temporal zone. Each red rectangle schematically represents the site of a single IPL pulse application. The numbers indicate the sequence of IPL pulse applications. Please click here to view a larger version of this figure.
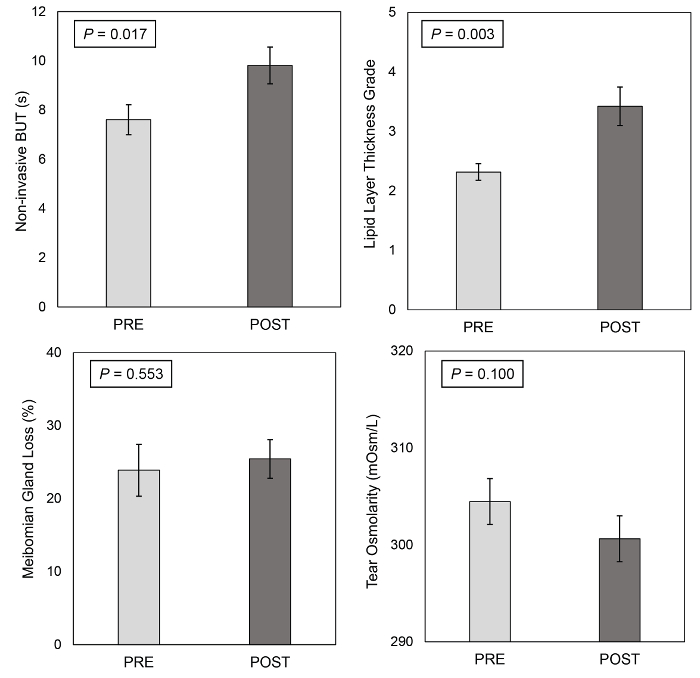
Figure 2. Automated ocular surface workup before and after the treatment. Noninvasive BUT, lipid layer thickness (LLT), meibomian gland loss (MGL) and tear osmolarity before and 15 days after the third intense pulsed light treatment session. Error bars represent the standard error of the mean. Please click here to view a larger version of this figure.
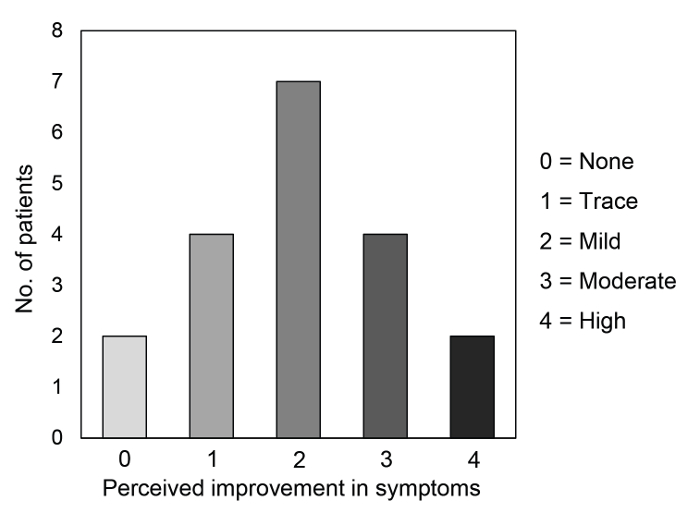
Figure 3. Patients' perceived improvement in dry eye symptoms after the treatment. The distribution of the patients according to the 5-grade scale about their perceived improvement in symptoms assessed 15 days after the third intense pulsed light treatment session. Please click here to view a larger version of this figure.
List of Materials
| I.C.P. Tearscope | SBM Sistemi, Turin, Italy | 1340864/R | Device for noninvasvive break-up time and lipid layer thickness evaluation |
| I.C.P. MGD | SBM Sistemi, Turin, Italy | 15006 | Device performing infrared meibomography and meibomian gland loss evaluation |
| TearLab Osmolarity System | TearLab Corporation, San Diego, CA, USA | 83861QW | Device for the measurement of tear osmolarity |
| E>Eye | E-Swin, Paris, France | Intense pulsed regulated light treatment device | |
| BM 900 Slit Lamp Biomioscropy | Haag-Streit, Koeniz, Switzerland | BM 900 | Slit Lamp Biomiscroscopy |
| Tobradex eye drops | Alcon Inc., Fort Worth, TX, USA | S01CA01 | Eye drops instilled immediately after the procedure in office |
Lab Prep
Dry eye disease (DED) is an increasingly common condition and one of the most common complaints of patients. The vast majority of DED is caused by the so-called "evaporative" subtype, that is mainly caused by meibomian gland dysfunction (MGD). Intense pulsed light (IPL) devices employ high intensity pulses of polychromatic lights with a broad range of wavelength (515-1200 nm). IPL treatment has been utilized for years in the field of dermatology, and then its use was applied to ophthalmology for the treatment of MGD. Recently, a new device employing IPL was specifically designed for the periocular application. This procedure determines the thermal selective coagulation and ablation of superficial blood vessels and telangiectasias of the eyelids skin, reducing the release of inflammatory mediators and tear cytokines levels, and improving meibomian glands outflow. IPL treatment is noninvasive and easy to perform, lasts for only a few minutes and can be conducted in an office setting. In the present study, 19 patients underwent 3 sessions of IPL treatment. After treatment, both mean noninvasive break-up time and lipid layer thickness grade significantly increased, as a result of an improvement of tear film stability and quality, respectively. Conversely, no statistically significant changes were found for meibomian gland loss and tear osmolarity. Furthermore, the vast majority of the treated patients (17/19; 89.5% of the total) perceived an improvement of their ocular discomfort symptoms after IPL treatment. Although IPL treatment provides an improvement of both ocular surface parameters and ocular discomfort symptoms after one cycle of three sessions, regular repeated treatments are usually required to maintain the persistence over the time of its beneficial effects.
Dry eye disease (DED) is an increasingly common condition and one of the most common complaints of patients. The vast majority of DED is caused by the so-called "evaporative" subtype, that is mainly caused by meibomian gland dysfunction (MGD). Intense pulsed light (IPL) devices employ high intensity pulses of polychromatic lights with a broad range of wavelength (515-1200 nm). IPL treatment has been utilized for years in the field of dermatology, and then its use was applied to ophthalmology for the treatment of MGD. Recently, a new device employing IPL was specifically designed for the periocular application. This procedure determines the thermal selective coagulation and ablation of superficial blood vessels and telangiectasias of the eyelids skin, reducing the release of inflammatory mediators and tear cytokines levels, and improving meibomian glands outflow. IPL treatment is noninvasive and easy to perform, lasts for only a few minutes and can be conducted in an office setting. In the present study, 19 patients underwent 3 sessions of IPL treatment. After treatment, both mean noninvasive break-up time and lipid layer thickness grade significantly increased, as a result of an improvement of tear film stability and quality, respectively. Conversely, no statistically significant changes were found for meibomian gland loss and tear osmolarity. Furthermore, the vast majority of the treated patients (17/19; 89.5% of the total) perceived an improvement of their ocular discomfort symptoms after IPL treatment. Although IPL treatment provides an improvement of both ocular surface parameters and ocular discomfort symptoms after one cycle of three sessions, regular repeated treatments are usually required to maintain the persistence over the time of its beneficial effects.
Procedure
Dry eye disease (DED) is an increasingly common condition and one of the most common complaints of patients. The vast majority of DED is caused by the so-called "evaporative" subtype, that is mainly caused by meibomian gland dysfunction (MGD). Intense pulsed light (IPL) devices employ high intensity pulses of polychromatic lights with a broad range of wavelength (515-1200 nm). IPL treatment has been utilized for years in the field of dermatology, and then its use was applied to ophthalmology for the treatment of MGD. Recently, a new device employing IPL was specifically designed for the periocular application. This procedure determines the thermal selective coagulation and ablation of superficial blood vessels and telangiectasias of the eyelids skin, reducing the release of inflammatory mediators and tear cytokines levels, and improving meibomian glands outflow. IPL treatment is noninvasive and easy to perform, lasts for only a few minutes and can be conducted in an office setting. In the present study, 19 patients underwent 3 sessions of IPL treatment. After treatment, both mean noninvasive break-up time and lipid layer thickness grade significantly increased, as a result of an improvement of tear film stability and quality, respectively. Conversely, no statistically significant changes were found for meibomian gland loss and tear osmolarity. Furthermore, the vast majority of the treated patients (17/19; 89.5% of the total) perceived an improvement of their ocular discomfort symptoms after IPL treatment. Although IPL treatment provides an improvement of both ocular surface parameters and ocular discomfort symptoms after one cycle of three sessions, regular repeated treatments are usually required to maintain the persistence over the time of its beneficial effects.
