Oblique Lumbar Interbody Fusion at L5-S1 Segment Through an Approach Between the Psoas Muscle and the Great Vessels
Instructor Prep
concepts
Student Protocol
This study was carried out in accordance with the clinical ethics committee guidelines of the First Affiliated Hospital of Zhejiang University. Written informed consent was obtained from all participating patients. The OLIF L5-S1 technique is indicated for patients with various spinal pathologies of L5-S1 involving degenerative disc disease, lumbar spondylosis, low-grade spondylolisthesis, and scoliosis. Patients with a history of trauma, neoplasia, or infection were excluded.
1. Patient position
- All patients were operated under general anesthesia with endotracheal intubation. Place patients in a lateral decubitus position on a radiolucent table, with fixation at the greater trochanter and shoulder (Figure 1A,B).
- Use a left-sided approach for multi-level spine reconstruction involving the L5-S1 junction to minimize the risk of injury to the great vessels. In the case of patients with a scoliotic spine convex or prior left-sided abdominal surgery, a right-sided approach was considered.
2. Approaching the L5-S1 intervertebral disc between the Psoas muscle and the great vessels
- Obtain an accurate lateral view of the lumbar spine using fluoroscopy. Mark the anterior superior iliac spine (ASIS) and L5-S1 disc locations on the skin. Roughly 2 cm anterior to ASIA, make a 4 cm oblique anterolateral incision toward the midpoint landmark of the L5-S1 disc (Figure 1B).
- After making a skin incision, use a vascular clamp to dissect the external oblique, internal oblique, and transversus abdominis muscles along their fiber lines (Figure 1C). Make a blunt dissection to access the retroperitoneal space and the retroperitoneal fat, peritoneum, and ureter. Shift the tissues and organs forward using tonsil sponges.
- Extend the retroperitoneal dissection over the anterior Psoas muscle border until the iliac vessels are visualized.
- Use a handheld retractor to gently mobilize the left iliac artery anteriorly to expose the entry to the L5-S1 disc, guided by the left common iliac vein. Dissect with a suction apparatus to clear fatty connective tissue in this region. This meticulous dissection creates a surgical window approximately 1.8 cm wide on the anterolateral side of the L5-S1 disc (Figure 1D).
- If the iliolumbar vein was encountered at the L5-S1 disc entry point, preserve it unless it obstructs the surgical field. In instances of obstruction, use bipolar cautery or clipping to manage the vein before the discectomy.
3. Exposure of surgical field at the L5-S1 disc
- Once the L5-S1 level is confirmed via fluoroscopy (Figure 1E), use a handled retractor and Kirschner wires to sustain proper exposure, avoiding the need for expansion retractors.
- Position the handled retractor laterally to the iliac vessels, offering gentle retraction. Insert Kirschner wires into the L5 and S1 vertebral bodies, minimizing Psoas major muscle retraction and keeping the iliolumbar vein outside the surgical window. Position the Kirschner wires close to the end plate while minimizing the neurovascular risk.
4. Discectomy and cage insertion
- Perform discectomy and endplate preparation within the surgical field. Carry out discectomy using a pituitary rongeur, followed by the preparation of the endplate using elongated angled curettes, as previously described by Kim et al.8. Carry out sequential trials with different-sized cages for disc space distraction and contralateral annulus release (Figure 1F-H).
- After selecting an appropriate cage size based on preoperative planning and intraoperative trial sizing, place a bone graft and bone marrow from the iliac crest within the cage.
- For L5-S1, the elevated position of the iliac crest poses a challenge for conventional cage insertion. Use a supplementary cage insertion approach to navigate this obstacle (Figure 2A-F).
- Insert the cage obliquely until approximately 75% of the cage is within the disc space. Use a shorter implant inserter to tap the anteromedial corner of the cage, allowing orthogonal turning and further insertion (Figure 2D-F).
- Apply strict radiological anteroposterior and lateral radioscopic control during cage insertion until optimal positioning is achieved intraoperatively. Use a small retractor to shield the iliac vessels.
5. Pedicle screws fixation
- Carry out posterior fixation using pedicle screws in the prone position. Mark pedicle entry points via fluoroscopy before surgery. Choose the connecting point of the transverse process, the upper articular process, and the vertebral lamina as the entry point for the pedicle.
- Perform a longitudinal midline skin incision with a scalpel, followed by the identification of the anatomical cleavage between the multifidus and longissimus muscles to expose the pedicle screw entry points. Insert pedicle screws with their positions confirmed using fluoroscopy. The pedicle screws were located within the pedicles.
- Close the fascia with running stitches and close the skin with an intradermic suture.
6. Postoperative period
- Remove the incision drain on the first postoperative day. Carry out postoperative pain control using nonsteroidal anti-inflammatory drugs, narcotic analgesics, and muscle relaxants.
- Obtain early lumbar X-rays at 2 to 3 postoperative days to verify cage and pedicle fixation positions.
- Allow the patients to ambulate with waist circumference protection. Most patients were discharged within 4 to 5 days after the operation.
7. Radiographic and clinical evaluation
- Obtain radiographs preoperatively, immediately postoperatively, and at 3-6 months, 9-12 months, and the last follow-up. Perform CT scans at 9 and 12 months postoperatively and at the final follow-up to assess bone union. Determine fusion status by continuous trabeculae bridging bone formation without gaps between the vertebral endplate and the cage.
- Assess lower back pain using a visual analog scale score. The Oswestry disability index was recorded preoperatively, at 1 and 12 months, postoperatively. Document perioperative data and complications.
Oblique Lumbar Interbody Fusion at L5-S1 Segment Through an Approach Between the Psoas Muscle and the Great Vessels
Learning Objectives
Clinical outcomes
A total of 20 patients underwent OLIF L5-S1 via a retroperitoneal oblique corridor between the Psoas muscle and the great vessels. The study population exhibited female predominance (n=12, 60%), with a mean age of 55.4 ± 6.8 years. OLIF L5-S1 procedures were performed on patients with isthmic spondylolisthesis (n=10), degenerative disc disease (n=6), and degenerative spondylolisthesis (n=4). The procedures included single-level (n=16) and two-level cases (n=4), involving L4-L5 (n=4) and L5-S1 (n=20). The mean blood loss volume was 133.4 ± 48.5 mL, and the average operative time was 153.6 ± 38.3 min. Based on preoperative axial MR images, the left common iliac vein (LCIV) was categorized into three types according to the difficulty of mobilization: type I – no requirement for mobilization; LCIV runs laterally for more than two-thirds of the length of the left side of the L5-S1 disc, type II – easy mobilization; LCIV obstructs the L5-S1 disc space, but the perivascular adipose tissue is present under the LCIV, and type III – potentially difficult mobilization; no perivascular adipose tissue under the LCIV. In our series, patients were classified as type I (n=3), type II (n=14), and type III (n=3) LCIV. For two patients with type III LCIV, no other perioperative complications were observed apart from iliolumbar vein lacerations during exposure.
The preoperative VAS score for lower back pain was 6.3 ± 1.5, significantly decreasing to 1.2 ± 0.8 at 12 months. The VAS score for lower limb pain was 5.6 ± 1.4 preoperatively and significantly decreased to 0.8 ± 0.3 at 12 months (Figure 3). The preoperative Oswestry disability index improved from 82.4% ± 16.2% preoperatively to 8.1% ± 2.0% at 12 months (Figure 4).
Radiographic outcomes
Postoperative radiographic examinations confirmed improved reconstruction at the lumbosacral junction for all patients. At the final follow-up, bony fusion was observed in all patients (Figure 5). No cage retropulsion or pedicle screw loosening cases were observed.
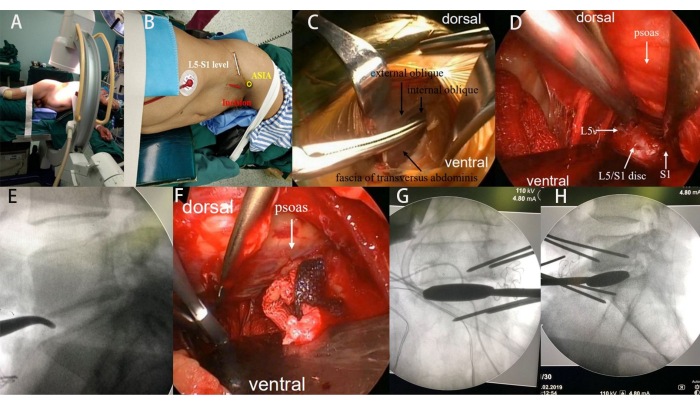
Figure 1: Intraoperative photographs. (A-B) The patient's lateral decubitus position and skin marking for the incision. (C) Blunt dissection involving the external oblique, internal oblique, and transversus abdominis muscles. (D) Exposure of the L5-S1 disc space using handheld retractors and Kirschner wire pins. (E) Intraoperative confirmation of the L5-S1 disc space by fluoroscopy. (F-H) Sequential use of different trial sizes to distract the disc space and release the contralateral annulus. Please click here to view a larger version of this figure.
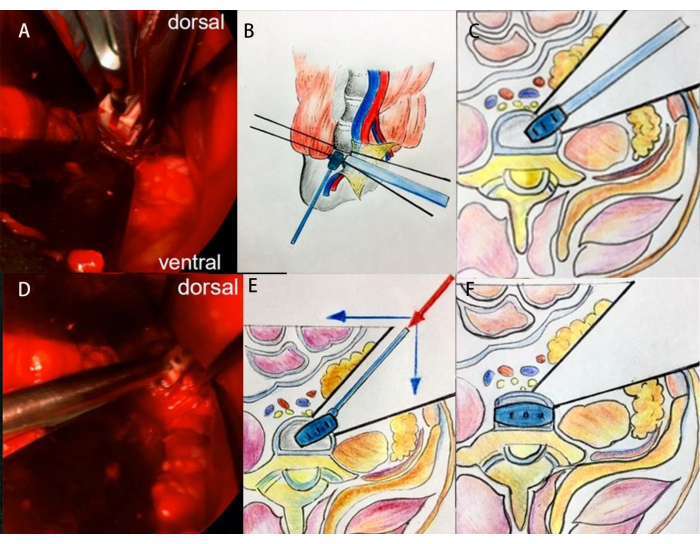
Figure 2: Intraoperative clinical images and schematic diagrams illustrating the technique for cage insertion at the L5-S1 segment. (A-C) First step of cage insertion. (D-F) The second step of cage insertion. Please click here to view a larger version of this figure.
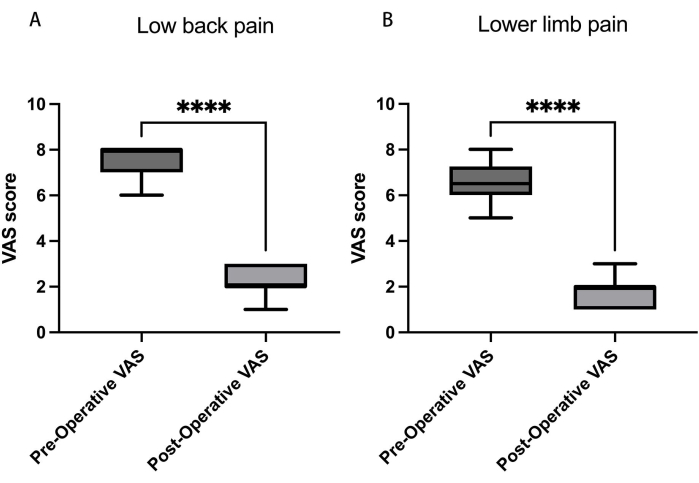
Figure 3: Visual analog scores (VAS) for low back and leg pain. (A) Over 12 months, the VAS score for lower back pain reduced from 6.3 ± 1.5 to 1.2 ± 0.8, and (B) for lower limb pain, the VAS score decreased from 5.6 ± 1.4 preoperatively to 0.8 ± 0.3. Data presented as mean ± SD. ****: Signifies a significant difference by Student's t-tests (p < 0.001). Please click here to view a larger version of this figure.
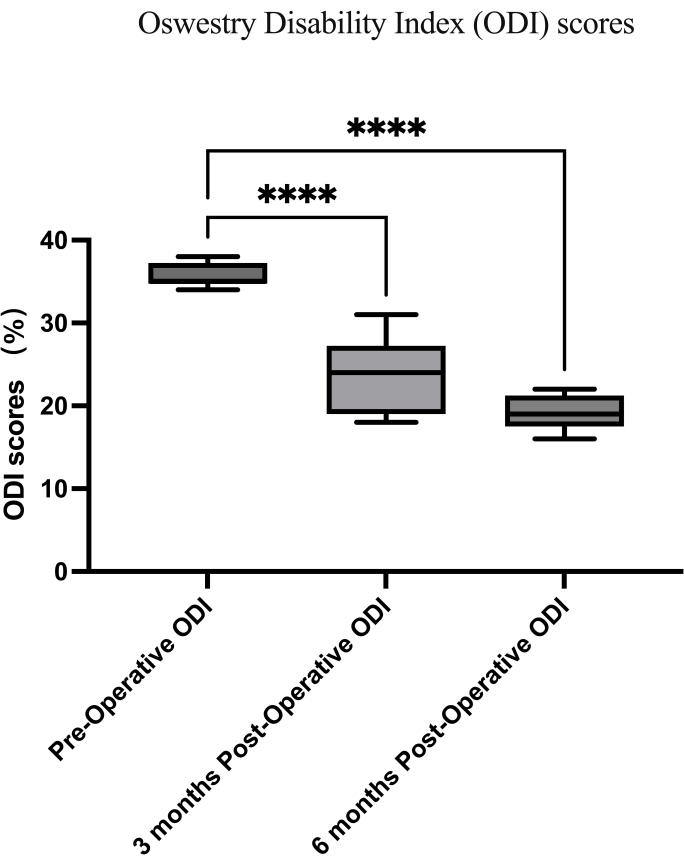
Figure 4: Oswestry disability index scores. The preoperative Oswestry disability index (ODI) improved from 82.4% ± 16.2% to 8.1% ± 2.0% at 12 months. Data presented as mean ± SD. ****: Signifies a significant difference by Student's t-tests (p < 0.001). Please click here to view a larger version of this figure.
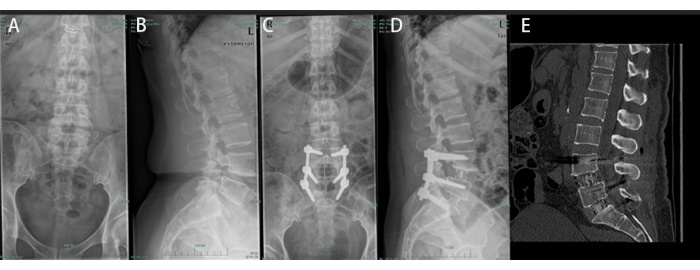
Figure 5: A 51-year-old male undergoing OLIF from L4-5 to L5-S1. (A, B) Preoperative anteroposterior and lateral radiographs displaying spondylolytic spondylolisthesis at L4-L5 and L5-S1. (C, D) Postoperative anteroposterior and lateral radiographs reveal satisfactory L4-S1 reconstruction. (E) Bony union was observed at the final follow-up. Please click here to view a larger version of this figure.
List of Materials
| Fluoroscopy System | Allengers | ||
| Handheld retractor | gSource | gS 36.9362 | |
| Kirschner wire | Sklar surgical instruments | SKU 40-1535 | |
| OLIF cages | Medtronic Sofamor Danek, Memphis, Tennessee, USA | ||
| Pedicle screws | Beijing Fule Technology Development Co. , Ltd China | ||
| Tonsil sponge | teleflex | MC-008133 | |
| Vascular clamp |
Lab Prep
Over the years, the oblique lateral interbody fusion (OLIF) technique has gained significant recognition for treating various spinal conditions in lumbar segments L2-L5. However, the adoption of OLIF for the L5-S1 segment has not been widely embraced by the spinal surgery community, given that significant concerns remain regarding the applicability of OLIF for lumbosacral fusion. In this study, a cohort of 20 patients underwent interbody fusion at the L5-S1 level using the OLIF technique through a single retroperitoneal oblique approach positioned between the Psoas muscle and the great vessels. The procedure involved discectomy and endplate preparation accomplished through a surgical window created on the anterolateral side of the L5-S1 disc. For secure interbody fusion cage placement, a supplementary cage insertion approach was employed. All patients were followed up for a minimum of 12 months. The mean preoperative visual analog scale (VAS) score for lower back pain was 6.3 ± 1.5 and experienced a significant reduction to 1.2 ± 0.8 at 12 months. The VAS score for lower limb pain significantly decreased from 5.6 ± 1.4 preoperatively to 0.8 ± 0.3 at 12 months after the surgery. Furthermore, the preoperative Oswestry disability index (ODI) improved from 82.4% ± 16.2% to 8.1% ± 2.0% at 12 months. Radiographic evaluations after surgery confirmed improved lumbosacral junction reconstruction for all patients. At the final follow-up, successful bony fusion was observed in all cases. Based on these findings, the OLIF technique for L5-S1 fusion represents an attainable approach for lumbosacral reconstruction. The procedure's success hinges on a comprehensive preoperative plan and precise intraoperative techniques.
Over the years, the oblique lateral interbody fusion (OLIF) technique has gained significant recognition for treating various spinal conditions in lumbar segments L2-L5. However, the adoption of OLIF for the L5-S1 segment has not been widely embraced by the spinal surgery community, given that significant concerns remain regarding the applicability of OLIF for lumbosacral fusion. In this study, a cohort of 20 patients underwent interbody fusion at the L5-S1 level using the OLIF technique through a single retroperitoneal oblique approach positioned between the Psoas muscle and the great vessels. The procedure involved discectomy and endplate preparation accomplished through a surgical window created on the anterolateral side of the L5-S1 disc. For secure interbody fusion cage placement, a supplementary cage insertion approach was employed. All patients were followed up for a minimum of 12 months. The mean preoperative visual analog scale (VAS) score for lower back pain was 6.3 ± 1.5 and experienced a significant reduction to 1.2 ± 0.8 at 12 months. The VAS score for lower limb pain significantly decreased from 5.6 ± 1.4 preoperatively to 0.8 ± 0.3 at 12 months after the surgery. Furthermore, the preoperative Oswestry disability index (ODI) improved from 82.4% ± 16.2% to 8.1% ± 2.0% at 12 months. Radiographic evaluations after surgery confirmed improved lumbosacral junction reconstruction for all patients. At the final follow-up, successful bony fusion was observed in all cases. Based on these findings, the OLIF technique for L5-S1 fusion represents an attainable approach for lumbosacral reconstruction. The procedure's success hinges on a comprehensive preoperative plan and precise intraoperative techniques.
Procedure
Over the years, the oblique lateral interbody fusion (OLIF) technique has gained significant recognition for treating various spinal conditions in lumbar segments L2-L5. However, the adoption of OLIF for the L5-S1 segment has not been widely embraced by the spinal surgery community, given that significant concerns remain regarding the applicability of OLIF for lumbosacral fusion. In this study, a cohort of 20 patients underwent interbody fusion at the L5-S1 level using the OLIF technique through a single retroperitoneal oblique approach positioned between the Psoas muscle and the great vessels. The procedure involved discectomy and endplate preparation accomplished through a surgical window created on the anterolateral side of the L5-S1 disc. For secure interbody fusion cage placement, a supplementary cage insertion approach was employed. All patients were followed up for a minimum of 12 months. The mean preoperative visual analog scale (VAS) score for lower back pain was 6.3 ± 1.5 and experienced a significant reduction to 1.2 ± 0.8 at 12 months. The VAS score for lower limb pain significantly decreased from 5.6 ± 1.4 preoperatively to 0.8 ± 0.3 at 12 months after the surgery. Furthermore, the preoperative Oswestry disability index (ODI) improved from 82.4% ± 16.2% to 8.1% ± 2.0% at 12 months. Radiographic evaluations after surgery confirmed improved lumbosacral junction reconstruction for all patients. At the final follow-up, successful bony fusion was observed in all cases. Based on these findings, the OLIF technique for L5-S1 fusion represents an attainable approach for lumbosacral reconstruction. The procedure's success hinges on a comprehensive preoperative plan and precise intraoperative techniques.
