Author Spotlight: Effectiveness of Extracorporeal Shockwave Therapy in Achilles Tendinopathy Treatment
Summary
Achilles tendinopathy is a common musculoskeletal condition for which loading programs are currently the standard of care. However, the treatment protocols vary. We therefore propose a protocol for Achilles tendinopathy treatment using extracorporeal shockwave therapy.
Abstract
Achilles tendinopathy is a common musculoskeletal condition characterized by pain, lower muscle strength, gait abnormality, and reduced quality of life. There are two categories of Achilles tendinopathy: insertional Achilles tendinopathy and mid-portion Achilles tendinopathy. Currently, mechanical loading programs are considered the standard of care for the population with Achilles tendinopathy.
Extracorporeal shockwave therapy (ESWT) is considered a secondary conservative treatment for tendinopathy as it is effective and safe. It can be used either as a monotherapy or as part of a multimodal treatment plan. ESWT has been extensively studied in orthopedics, where it was shown to intensify fracture healing and successfully treat overuse conditions of tendons and fascia. It is believed that shockwaves have both mechanical and cellular effects that ultimately result in the repair of damaged tendinous tissue and improved function of the Achilles tendon. However, there is a lack of consistency in the literature surrounding the effectiveness, especially the protocols. Therefore, we enrolled 36 patients with a diagnosis of Achilles tendinopathy, using radial ESWT (0.48 mJ/mm2, 2,000 shockwaves, 10 Hz, 1.6 bars, 2 sessions once a week). Freedom from pain was experienced by 16.7% of these participants, and there was a significant decrease in pain in all of them.
Introduction
The Achilles tendon is one of the most robust tendons in the body, yet it is highly susceptible to injuries. Tendons play a crucial role in enabling joint motion and stability by transmitting tensile loads produced by muscles onto bones1. Tendinopathy is a concept describing chronic tendon degeneration and deconditioning, also called tendinitis2. However, the exact cause of Achilles Tendinopathy2 remains unclear. It is believed to result from a combination of factors, including overuse stresses, impaired blood flow, and lack of flexibility2. One of the major contributors to the development of Achilles tendon injuries is the excessive load force applied during intense activities such as running, without allowing sufficient time for proper tendon repair1. This continuous stress on the tendon can lead to the gradual accumulation of microtraumas and ultimately result in injury progression3. This highlights the importance of proper management, rest, and adequate rehabilitation periods in preventing such injuries and maintaining the health of the Achilles tendon. The diagnosis of Achilles tendinopathy relies mainly on a comprehensive patient history and clinical examination4. A typical symptom is the occurrence of morning stiffness or limited range of motion after prolonged inactivity, accompanied by gradually increasing pain during physical activity2. Athletes often go through pain at the beginning and end of the training, with a period of decreased discomfort in between. However, since the condition worsens, even slight exertion can lead to the onset of pain, greatly affecting daily activities. In severe cases, individuals may even experience pain while at rest5.
The management of Achilles tendinopathy primarily involves conservative approaches, even though approximately 25%-29% of patients may eventually require surgery for the condition5. Cardoso et al.6 summarized an overview of the current treatment of Achilles tendinopathy, including medications, exercise, corticosteroid injections, platelet-rich plasma injections, manual therapy, and modalities. Among these treatments, the most widely recommended is exercise, which targets the injured tendons, especially mechanical loading exercises; eccentric exercise has been considered a better intervention. Even though it has been proven useful to decrease pain and improve function in the short term, a significant portion of patients have not responded to this strategy in a long-term study7, and some patients seek other treatments.
In recent years, extracorporeal shockwave therapy (ESWT) has demonstrated beneficial effects on musculoskeletal disorders and has become an effective treatment for tendinopathy8,9. There is now increasing evidence supporting the effectiveness of ESWT for lower extremity tendinopathy10 and upper extremity tendinopathy11. Originally used in urology for kidney stone treatment, ESWT has found therapeutic application in a wide range of medical and musculoskeletal conditions, making it a major innovation in the field of regenerative medicine12. There are two types of ESWT: focused shock waves and radial pressure waves13,14; the main difference between them is their physical characteristics. As a result, they stimulate diverse regenerative biological reactions in musculoskeletal tissue, activating proteins that play a role in chondroprotection15, vessel regeneration16,17, reducing inflammatory18, anti-apoptosis19, immunomodulation20, neurophysiological mechanisms, and pain relief11. ESWT also triggers the initiation of the healing processes, which facilitates the proliferation, differentiation, and migration of diverse cell types such as mesenchymal stem cells, endothelial cells, fibroblasts, and tendon cells. Additionally, it promotes the synthesis of collagen21. Furthermore, ESWT has been found to induce several tendon-specific responses that facilitate the healing progress22.
Although radial-ESWT is considered effective in Achilles tendinopathy treatment, there are various reports on the technique of radial ESWT without any consensus on the parameters. In this paper, we present a detailed treatment protocol for treating Achilles Tendinopathy using ESWT.
Protocol
This protocol was approved by our institution's human research ethics committee and received informed consent from the subjects. Individuals older than 18 years old, both sexes, with a definite diagnosis of Achilles tendinopathy, were enrolled. Participants who received ankle surgery recently or were diagnosed with any conditions that were contraindications to the treatment were excluded.
1. Patient evaluation
- Clinical examination
- Before implementing the protocol, clinically evaluate the patients to rule out other regions that may cause symptoms. Obtain a thorough medical history, including the history of treatments, and rule out any contraindications (e.g., pregnancy, placement over major blood vessels and nerves, presence of pacemakers or other implanted devices, open wounds, joint replacements, epiphysis, blood clotting disorders, active infection, presence of cancerous tissues, impaired mental status of the patient, and/or unwillingness to cooperate).
- Physiotherapy examination
- Perform a physical examination to assess the condition being treated through inspection and palpation and evaluate the range of motion (both active and passive) of the ankle.
- Obtain the baseline information of the patient, such as pain and range of motion, using the Victorian Institute of Sports Assessment-Achilles (VISA-A) and/or American Orthopedic Foot and Ankle Society (AOFAS) Hindfoot score as outcome measures5,9,12.
2. Application technique
NOTE: Before starting the procedure, check whether all the equipment listed in the Table of Materials is available.
- Place the patient in a comfortable prone position, with the target area exposed. If the patient is found to have significant tenderness in the calf muscles during the physical examination, expose the lower leg.
- Locate the area that requires treatment after the physical examination and mark these points using a felt tip pen.
- Choose a transmitter based on the desired depth of penetration for the treatment point (Figure 1). Use the conductor R 15 for tendinopathy and D20 (in this study, with energy 0.48 mJ/mm2) for tendinopathy and the trigger point of the deep muscle. Inform the patient that regular sounds made by the transmitters may be heard during treatment.
- Dry the skin thoroughly and apply an adequate amount of gel to the target area as a coupling agent.
NOTE: Apply the gel adequately to the treated area and ensure that the shock wave conductors are in contact with the skin surface throughout the treatment. - As the operator, work in an ergonomic position (Figure 2) to optimize comfort and efficiency. To obtain the best treatment results, ensure good contact between shock wave transducers and the patient's skin during treatment.
NOTE: Do not press the treatment output handle tightly to the affected part; this will not help the treatment. - Device setup
- Press the Power On/OFF button or touch the liquid crystal display (LCD).
- Inspect parameter options on the display and press the buttons directly on the LCD to make a selection. Adjust the parameters using the up and down buttons.
- Press the Pause or Stop buttons located on the Operator Interface to stop the output.
NOTE: Information on the intensity and number of pulses given during the treatments can be obtained from the LCD.
- Editing the treatment screen and parameter modification
- Press the edit button and wait for the Edit treatment screen to display. Increase and decrease the parameters on the Edit treatment screen by pressing the up and down buttons as needed during the treatment process based on the patient's tolerance and response.
- Select the intensity to be used (1.6 Bar in this study). Start at a lower intensity of the therapy, then gradually increase the intensity as high as the patient can tolerate. The recommended intensity range is between 1.4 Bar and 3.0 Bar23.
- Set the frequency of the treatment (10 Hz here). Choose a frequency between 8 Hz and 15 Hz for the treatment24.
- Establish the desired number of shocks to be applied (2,000 in this study); the number of shocks per treatment is 800-3,00023,24.
- Begin the treatment by pressing the Start button on the User Interface and activate the handpiece by pressing the trigger button on the handpiece. The unit begins emitting radial pressure wave energy. During the treatment, maintain the contact between the conductor and the skin tissue, and move the handle by drawing a small circle.
- Stopping and pausing therapy
- Stop the therapy by pressing the Stop button on the User Interface.
- Press the Pause button on the User Interface or the trigger button on the handpiece to pause the therapy at any time.
- Plan three sessions spaced 1 week apart25.
3. Posttreatment protocol
- Remove any residual coupling gel from the treated area.
- After treatment, ask the patients to apply ice for no more than 10 min if they feel discomfort. In some cases, patients may suffer intense pain because of an acute resorption process caused by the shock waves.
- To consolidate the therapeutic effect, if necessary, combine ESWT with other physical therapy treatments, such as modalities and exercise. Recommend that the patient do muscle exercise after treatment, especially eccentric exercise23,24.
- Ask the patients to report and look for side effects such as reddening, swelling, pain, hematoma, petechiae, red spots, and skin lesions after previous ESWT; these effects usually appear within a few days after shock wave therapy. Ensure that the symptoms disappear completely before starting treatment.
- If there are no changes in outcome measures, advise the patients to seek a new treatment module or move on to invasive procedures.
Representative Results
A retrospective study of patients with Achilles tendinopathy was performed on individuals older than 18 years old, with a definite diagnosis of Achilles tendinopathy. Exclusion criteria were recent ankle surgery or any condition that is a contraindication of ESWT.
This study included 36 participants. diagnosis with Achilles tendinopathy, 18 females and 18 males. Of these patients, their average age was 43.7 years, ranging between 18 and 64 years. All the patients complained of pain; 11 out of 36 patients had reduced range of motion (Table 1).
The treatment protocol was applied to all participants. In our study, the minimum number of sessions was one, and the maximum was eight. For these participants, a significant decrease in pain was achieved, and 4 of them were even pain-free after treatment, although all of them complained of pain at the beginning. Only 4 of them had impairment of ankle range of motion at the end. They got a significant improvement in the VISA-A Scale, which increased from 50.3 to 90.5.
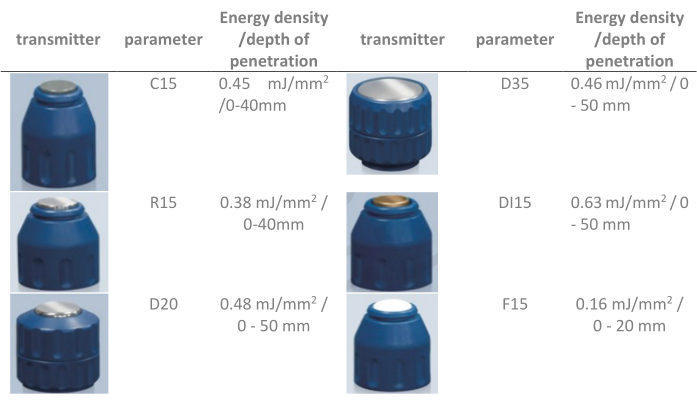
Figure 1: Illustrations of six different transmitters and their specifications. Please click here to view a larger version of this figure.

Figure 2: Applicator positioning. Please click here to view a larger version of this figure.
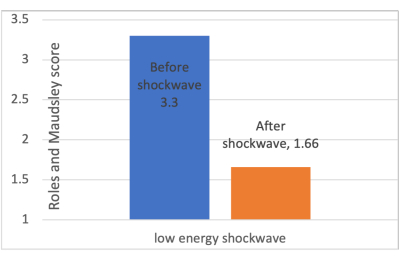
Figure 3: Changes in Roles and Maudsley scores before and after low-energy ESWT. The Roles and Maudsley scale allows the patient to subjectively describe their pain, with a score ranging from 0 to 4 points from excellent to poor. Abbreviation: ESWT = extracorporeal shockwave therapy. Please click here to view a larger version of this figure.
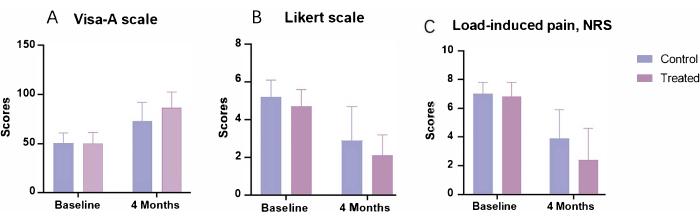
Figure 4: Changes in primary outcome measures before and after the 4 month follow-up. (A) The Victorian Institute of Sport Assessment-Achilles Scale used to evaluate the clinical severity of patients with chronic Achilles tendinopathy, had a maximum score of 100. (B) The Likert scale, used for general assessment, was scored by the patient on a 6 point scale (1 = completely recovered, 2 = much improved, 3 = somewhat improved, 4 = hardly improved, 5 = not improved, 6 = worse). (C) Numeric Rating Scale used to assess pain severity when patients with Achilles tendinopathy load, using a 0-10 scale. The control group received a 12 week eccentric exercise program, and the treated group received the same exercise protocol combined with three sessions of radial-ESWT treatment. Abbreviations: ESWT = extracorporeal shockwave therapy; VISA-A = Victorian Institute of Sport Assessment-Achilles; NRS = Numeric Rating Scale. Please click here to view a larger version of this figure.
| Demographic characteristics | ||
| Age | 43.7(18-64) | |
| Gender | Male | 18(50%) |
| Female | 18(50%) | |
| Number of sessions | 2.58(1-8) | |
| Visual Analogue Scale(VAS) | Before | 4.06(3-5) |
| After | 1.28(0-3) | |
| Stiffness | Before | 11(30.5%) |
| After | 4(11.1%) | |
| Complications | 10(27.8) | |
Table 1: Demographic characteristics. Visual Analogue Scale used Numerical rating scales with 0-10 scores; a higher score indicates greater pain intensity. Abbreviation: VAS = Visual Analogue Scale.
| Authors | N. partici-pants | Follow-up (months) | Treatment | Parameters | outcome measures (pain) | Functional improvement | |||||
| Rompe et al. 24 | 68 | 4 | eccentric loading vs eccentric loading + low-energy ESWT | radial ESWT, 2000 shocks, 3 Bar | VAS –13.5 (–22.5 to 5.5) ( P = .0016) |
Likert scale 0.8 (0.08 to 1.5), P = .035 |
|||||
| Pavone et al.26 | 40 | 12 | ESWT + eccentric exercises | Low-energy radial ESWT, 4 sessions, 800 shocks, 4 Hz | VAS −5.8 ± 1.2 SD (P < 0.001) |
AOFAS +19.8 ±5.0 SD (P < 0.001) |
|||||
| Saxena et al.27 | 60 | 12 | ESWT | low-intensity 2500 shocks, at 2.4 Bar ranging, 11 to 13 Hz | / | Roles-Maudsley 1.44 ± 0.87 SD (P < 0.001) |
|||||
| Vahdatpour et al.28 | 43 | 4 | ESWT vs Sham SWT | 1500 shocks, focused shockwaves (0.25–0.4 mJ/mm2, 2.3 Hz); 3000 shocks, radial shockwaves (1.8–2.6 mJ/mm2, 2.21 Hz). | VAS. −3.70±2.27 (p<0.001) | AOFAS 20.90±13.51, p<0.001 |
|||||
| Wheeler et al.29 | 39 | 6 | ESWT | 10 Hz and 2000 shocks | painDETECT questionnaire. −4.8 (NAT) and −3.9 (IAT) (P < 0.01) |
VISA-A 23% (0% to 43%)(IAT) and 11% (7% to 22%)(NAT) |
|||||
| Taylor et al.30 | 54 | 24 | ESWT | Low-energy radial ESWT, 2000 shots, 10 Hz, 1.5–2.5 bar | VAS −4.8 (NAT) and −3.9 (IAT) (P < 0.01) |
VISA-A +66 points (P < 0.001) |
|||||
Table 2: Case series and primary outcome measures after treatment. Abbreviations: SWT = shockwave therapy; ESWT = extracorporeal SWT; VAS = Visual Analogue Scale; NAT = Non-insertional Achilles tendinopathy; IAT = Insertional Achilles tendinopathy; VISA-A = Victorian Institute of Sport Assessment-Achilles; NRS = Numeric Rating Scale; AOFAS = American Orthopedic Foot and Ankle Society.
Discussion
This protocol outlines a standardized treatment protocol for Achilles tendinopathy utilizing radial-ESWT to reduce pain and improve lower extremity function and mobility. It is crucial to closely monitor the patient's response during treatment to avoid any potential adverse effects. In our study, we observed positive results when we used low-energy ESWT plus eccentric exercise. Table 2 lists the intervention methods and major conclusions of studies on the effectiveness of ESWT for Achilles tendinopathy24,26,27,28,29,30.
Our study showed significant improvements in pain and functional activity after ESWT treatment and did the same results of many studies21,22,23,24,25. In the study conducted by Vahdatpour et al.28, they also showed improvement in outcome measurement of scores of the functional questionnaire such as the American Orthopedic Foot and Ankle Society (AOFAS) questionnaire, except for pain relief, after receiving 4 sessions of ESWT therapy for 4 weeks. The average number of sessions in our study was 2.58, patients received at least 1 session and up to 8 sessions. There was a significant correlation between the number of sessions for shock waves and the degree of pain improvement (p < 0.05).
The effect caused by ESWT in triggering tendon regeneration in people with tendinopathy by stimulating an anti-inflammatory response was confirmed by previous studies that measured interleukins and metalloprotease concentration after ESWT treatment21,22. The effectiveness of ESWT is strongly based on the energy level, number of shocks, and frequency, and these factors need to be carefully taken into account23. Pavone26 and Saxena27 have recommended that it was more beneficial to use a low-energy radial shockwave because of the significant decrease in Roles and Maudsley scores (Figure 3). Therefore, in our protocol, we used the low-energy level (0.48 mJ/mm2). Moreover, except for ESWT treatment, we incorporated eccentric exercise, which has been confirmed to be beneficial by many researchers24,26,30,31,32. As in an RCT conducted by Rompe et al.24, 68 patients were categorized into two groups: one group received a 12 week eccentric exercise program, and the other one received the same exercise protocol combined with three sessions of radial-ESWT treatment (2,000 shocks, 3 bars, 8 Hz, 3 sessions). In the exercise-only group, 56% (19 out of 34 patients) reported complete recovery or substantial improvement, while in the combined approach group, this figure was 82% (28 out of 34 patients) (Figure 4).
In our protocol, after ESWT therapy, we added eccentric training at the end, since ESWT combined with eccentric exercises is beneficial for insertional Achilles tendinopathy27,28. A trial conducted by Rompe et al.24 showed that eccentric loading exercise associated with repetitive ESWT was more effective in pain alleviation and physical function improvement compared to eccentric loading alone for patients with midportion Achilles tendinopathy. In another study26, 40 patients who failed to recover after receiving 3 months of eccentric exercise protocols, were administered four sessions of Focused-ESWT treatment, at 2 week intervals, combined with eccentric exercise training. After the 12 month follow-up, no pain was reported in 65% of patients, and 28% were able to return to their usual activities despite experiencing some residual pain. The combined treatment approach involving ESWT and eccentric exercise was found to be effective for patients who did not observe substantial improvements after solely engaging in eccentric exercises.
The therapeutic effect of ESWT is influenced by many factors, such as the energy level30,33; in our study, we used low-dose shockwaves. Since low-energy ESWT is generally well-tolerated, anesthesia is not recommended due to the mild discomfort during impulse application. A study by Taylor et al.30 reported the risks associated with high doses of ESWT and recommended avoiding its use in patients with refractory Achilles tendon lesions since high-energy ESWT has an adverse effect on tendon recovery and can cause tissue damage. Furthermore, a study conducted by Chao et al.34 showed that lower energy levels with a low number of shocks had a positive stimulating effect, while high energy levels and high shock numbers had notably inhibitory effects.
In this study, patients received at least 1 session and up to 8 sessions; there was a significant correlation between the number of sessions and the degree of pain improvement. However, we lack data on the long-term effect of ESWT treatment, which is a limitation of our study. A study conducted by Vahdatpour et al.28 observed that in the 1 month follow-up, the ESWT group failed to show a significant improvement in outcome measures such as Visual analog scale (VAS) scores or American Orthopedic Foot and Ankle (AOFAS) scores. However, at the 4 month follow-up, there was a notable improvement in outcome measures in the group that received ESWT treatment. This suggests that it takes several weeks for the full effects of ESWT to become apparent. Similarly, Rasmussen et al.35 found there was a significant improvement in the AOFAS score at the 3 month follow-up, except for the VAS score. However, throughout the 3 month duration, the ESWT group consistently exhibited lower VAS scores, compared to the control group. A longer follow-up period might have yielded more accurate results.
There are some limitations of this technique. The first one is that some patients may be initially uncomfortable with the idea of ESWT. Therefore, ramping the intensity serves to acclimate the patient to the pressure of the output. Another limitation is the risk associated with high doses. Many researchers have proved that high-energy ESWT has adverse effects on tendon recovery and can cause tissue damage30,33,34.
In conclusion, ESWT is a promising treatment option for patients with Achilles tendinopathy, but its energy level and application way should be carefully considered to avoid negative effects. Combining ESWT with other therapies, especially with eccentric exercises, may further enhance its effectiveness in improving patient outcomes and pain relief. Carrying out a critical physical assessment before treatment and closely monitoring the patient's response throughout the treatment process is essential to guarantee safety as well as efficacy.
Disclosures
The authors have nothing to disclose.
Acknowledgements
None
Materials
| ESWT device | Chattanooga | Intelect RPW 2074-INT | incorporate touch screen technology to ensure a high degree of simplicity. The easy-to-use menu-drive user interface guarantees reliable selection of all necessary parameters for treatment set-up as well as during patient treatment. |
| Gel | KeppLer | KL-250 type II | In order to obtain the best treatment results, it is necessary to ensure good contact between shock wave transducers and the patient's skin during treatment. |
| Handpiece | Chattanooga | D-ACTOR Apllicator | The handle of the therapeutic apparatus can be used with a variety of transmitters, each of which is specially designed to achieve optimal efficacy. |
| Mark pen | general | ||
| Tissue | general | ||
| transmitters | Chattanooga | R15,D20 | Each type of transmitter has its own unique therapeutic effect and scope of application.In our study, we use R15 and D20. |
References
- Wang, J. H., Guo, Q., Li, B. Tendon biomechanics and mechanobiology-a minireview of basic concepts and recent advancements. Journal of Hand Therapy. 25 (2), 133-141 (2012).
- Li, H. Y., Hua, Y. H. Achilles tendinopathy: current concepts about the basic science and clinical treatments. BioMed Research International. 2016, 6492597 (2016).
- Del Buono, A., Chan, O., Maffulli, N. Achilles tendon: functional anatomy and novel emerging models of imaging classification. International Orthopedics. 37, 715-721 (2013).
- Paavola, M., Kannus, P., Paakkala, T., Pasanen, M., Järvinen, M. Long-term prognosis of patients with Achilles tendinopathy. The American Journal of Sports Medicine. 28 (5), 634-642 (2000).
- Cardoso, T. B., Pizzari, T., Kinsella, R., Hope, D., Cook, J. L. Current trends in tendinopathy management. Best Practice & Research Clinical Rheumatology. 33 (1), 122-140 (2019).
- Maffulli, N., Longo, U. G., Maffulli, G. D., Khanna, A., Denaro, V. Achilles tendon ruptures in elite athletes. Foot & Ankle International. 32 (1), 9-15 (2011).
- van der Plas, A., et al. A 5-year follow-up study of Alfredson’s heel-drop exercise programme in chronic midportion Achilles tendinopathy. British Journal of Sports Medicine. 46 (3), 214-218 (2012).
- Louwerens, J. K., Sierevelt, I. N., van Noort, A., van den Bekerom, M. P. Evidence for minimally invasive therapies in the management of chronic calcific tendinopathy of the rotator cuff: a systematic review and meta-analysis. Journal of Shoulder and Elbow Surgery. 23 (8), 1240-1249 (2014).
- Liao, C. D., Tsauo, J. Y., Chen, H. C., Liou, T. H. Efficacy of extracorporeal shock wave therapy for lower-limb tendinopathy: a meta-analysis of randomized controlled trials. American Journal of Physical Medicine & Rehabilitation. 97 (9), 605-619 (2018).
- Ioppolo, F., Rompe, J. D., Furia, J. P., Cacchio, A. Clinical application of shock wave therapy (SWT) in musculoskeletal disorders. European Journal of Physical and Rehabilitation Medicine. 50 (2), 217-230 (2014).
- d’Agostino, M. C., Craig, K., Tibalt, E., Respizzi, S. Shock wave as biological therapeutic tool: From mechanical stimulation to recovery and healing, through mechanotransduction. International Journal of Surgery. 24, 147-153 (2015).
- Foldager, C. B., Kearney, C., Spector, M. Clinical application of extracorporeal shock wave therapy in orthopedics: focused versus unfocused shock waves. Ultrasound in Medicine & Biology. 38 (10), 1673-1680 (2012).
- Moya, D., et al. The role of extracorporeal shockwave treatment in musculoskeletal disorders. The Journal of Bone and Joint Surgery. 100 (3), 251-263 (2018).
- Wang, C. J., et al. Changes of articular cartilage and subchondral bone after extracorporeal shockwave therapy in osteoarthritis of the knee. International Journal of Medical Sciences. 14 (3), 213-223 (2017).
- Holfeld, J., et al. Low energy shock wave therapy induces angiogenesis in acute hind-limb ischemia via VEGF receptor 2 phosphorylation. PLoS One. 9 (8), e103982 (2014).
- Tara, S., et al. Low-energy extracorporeal shock wave therapy improves microcirculation blood flow of ischemic limbs in patients with peripheral arterial disease: pilot study. Journal of Nippon Medical School. 81 (1), 19-27 (2014).
- Abe, Y., et al. Extracorporeal low-energy shock-wave therapy exerts anti-inflammatory effects in a rat model of acute myocardial infarction. Circulation Journal. 78 (12), 2915-2925 (2014).
- Chen, Y. L., et al. Extracorporeal shock wave therapy effectively prevented diabetic neuropathy. American Journal of Translational Research. 7 (12), 2543-2560 (2015).
- Davis, T. A., et al. Extracorporeal shock wave therapy suppresses the early proinflammatory immune response to a severe cutaneous burn injury. International Wound Journal. 6 (1), 11-21 (2009).
- Wess, O. J., et al. A neural model for chronic pain and pain relief by extracorporeal shock wave treatment. Urological Research. 36, 327-334 (2008).
- Waugh, C., et al. In vivo biological response to extracorporeal shockwave therapy in human tendinopathy: Response of tendinopathy to shockwave therapy. European Cells and Materials. 29, 268-280 (2015).
- Chen, Y., et al. Biological response of extracorporeal shock wave therapy to tendinopathy in vivo(review). Frontiers in Veterinary Science. 9, 851894 (2022).
- Stania, M., et al. Extracorporeal shock wave therapy for Achilles tendinopathy. BioMed Research International. 2019, 3086910 (2019).
- Rompe, J. D., Furia, J., Maffulli, N. Eccentric loading versus eccentric loading plus shock-wave treatment for midportion Achilles tendinopathy: a randomized controlled trial. American Journal of Sports Medicine. 37 (3), 463-470 (2009).
- Vo, T. P., Ho, G. W., Andrea, J. Achilles tendinopathy, a brief review and update of current literature. Current Sports Medicine Reports. 20 (9), 453-461 (2021).
- Pavone, V., et al. Low-energy extracorporeal shock-wave therapy in the treatment of chronic insertional Achilles tendinopathy: a case series. BioMed Research International. 2016, 7123769 (2016).
- Saxena, A., Ramdath, S., O’Halloran, P., Gerdesmeyer, L., Gollwitzer, H. Extra-corporeal pulsed-activated therapy ("EPAT" sound wave) for Achilles tendinopathy: a prospective study. The Journal of Foot and Ankle Surgery. 50 (3), 315-319 (2011).
- Vahdatpour, B., Forouzan, H., Momeni, F., Ahmadi, M., Taheri, P. Effectiveness of extracorporeal shockwave therapy for chronic Achilles tendinopathy: a randomized clinical trial. Journal of Research in Medical Sciences. 23, 37 (2018).
- Wheeler, P. C., et al. Extracorporeal shock wave therapy plus rehabilitation for insertional and noninsertional Achilles tendinopathy shows good results across a range of domains of function. The Journal of Foot and Ankle Surgery. 58 (4), 617-622 (2019).
- Taylor, J., et al. Extracorporeal shockwave therapy (ESWT) for refractory Achilles tendinopathy: a prospective audit with 2-year follow-up. The Foot. 26, 23-29 (2016).
- Wheeler, P. C., Tattersall, C. Novel interventions for recalcitrant Achilles tendinopathy: benefits seen following high-volume image-guided injection or extracorporeal shockwave therapy-a prospective cohort study. Clinical Journal of Sports Medicine. 30 (1), 14-19 (2020).
- Murphy, M., Travers, M., Gibson, W. Is heavy eccentric calf training superior to wait-and-see, sham rehabilitation, traditional physiotherapy and other exercise interventions for pain and function in mid-portion Achilles tendinopathy. Systematic Reviews. 7 (1), 1-7 (2018).
- Furia, J. P. High-energy extracorporeal shock wave therapy as a treatment for insertional Achilles tendinopathy. The American Journal of Sports Medicine. 34 (5), 733-740 (2006).
- Chao, Y. H., et al. Effects of shock waves on tenocyte proliferation and extracellular matrix metabolism. Ultrasound in Medicine & Biology. 34 (5), 841-852 (2008).
- Rasmussen, S., Christensen, M., Mathiesen, I., Simonson, O. Shockwave therapy for chronic Achilles tendinopathy: a double-blind, randomized clinical trial of efficacy. Acta Orthopaedical. 79 (2), 249-256 (2008).
Tags

.
