In Vivo Gene Delivery into Mouse Mammary Epithelial Cells Through Mammary Intraductal Injection
Summary
The present protocol describes intraductal injection of viral vectors via the teat to deliver genes of interest into the mammary epithelial cells.
Abstract
Mouse mammary glands comprise ductal trees, which are lined by epithelial cells and have one opening at the tip of each nipple. The epithelial cells play a major role in mammary gland function and are the origin of most mammary tumors. Introducing genes of interest into mouse mammary epithelial cells is a critical step in evaluating gene function in epithelial cells and generating mouse mammary tumor models. This goal can be accomplished through the intraductal injection of a viral vector carrying the genes of interest into the mouse mammary ductal tree. The injected virus subsequently infects mammary epithelial cells, bringing in the genes of interest. The viral vector can be lentiviral, retroviral, adenoviral, or adenovirus-associated viral (AAV). This study demonstrates how a gene of interest is delivered into mammary epithelial cells through mouse mammary intraductal injection of a viral vector. A lentivirus carrying GFP is used to show stable expression of a delivered gene, and a retrovirus carrying Erbb2 (HER2/Neu) is used to demonstrate oncogene-induced atypical hyperplastic lesions and mammary tumors.
Introduction
Epithelial cells of mammary glands play a major role in the function of these glands and are the major cell of origin of breast cancer. Studies of mammary gland biology and tumorigenesis frequently need the delivery of gene(s) of interest into these cells. Each mouse mammary gland comprises a ductal tree lined by epithelial cells with a single opening at the tip of the nipple. This structure makes the mammary epithelial cells easily accessible to viral vectors, which can be delivered into the lumen of a ductal tree via intraductal injection1.
The technique of mammary intraductal injection was originally used for much larger animals such as goats, rabbits, and rats1. For a much smaller animal such as mice, intraductal injection needs many delicate tools and more practices of the operators. There are two approaches for mouse intraductal injection. One is up-the-teat injection1. Another one is the direct injection of the primary duct of #3 or #4 mammary gland after surgical exposure1. Since the first one is non-invasive and faster once the operator has been well-trained, this technique is more commonly used and will be described in detail in this article.
Compared to the widely used traditional transgenic mouse models, in which the gene of interest is introduced at the stage of fertilized eggs through microinjection2,3,4, gene delivery through the intraductal virus injection method has many advantages, including: (1) it avoids the time-consuming process of making a transgenic mouse line for each gene of interest; (2) it avoids potential impairment on the normal development of mammary glands imposed by the gene of interest; (3) it introduces the gene of interest at any desired time after birth; (4) it can easily co-introduce more than one gene of interest; (5) it better mimics the natural tumorigenic process because the infected and thus oncogene-carrying cells are surrounded by normal cells; and (6) in combination with the TVA (tumor virus A, an avian cell surface protein and the receptor for retrovirus RCAS vector) technology5, the gene of interest can be introduced into a specific cell population to study the cell origin of tumorigenesis and to conduct cell lineage-tracing assays in the mammary glands6,7,8,9.
Any vectors derived from retrovirus10, lentivirus11,12, adenovirus13, and adenovirus-associated virus (AAV)14 may be used for intraductal delivery of genetic materials. Retrovirus and lentivirus vectors integrate into the host genome permanently; thus, they introduce genes of interest stably into mammary epithelial cells. While lentivirus can integrate into the genome of any cell it encounters15, the efficient genomic integration of retrovirus needs the proliferation of the target cells16. The adenoviral and AAV vectors do not integrate into the genome of infected cells and, therefore, only transiently express the gene of interest17,18. This feature can be an advantage when the gene of interest needs to be expressed for only a short amount of time, such as Cre, for deleting a floxed tumor suppressor gene.
Lentivirus, adenovirus, and AAV infect any mouse cells they encounter. But since luminal epithelium is largely insulated from the underlying basal layer, which is further separated from the stroma by the basement membrane, intraductal injection limits the infection largely to luminal epithelial cells, the primary cell of origin of breast cancer. Within this luminal epithelial layer, there are also distinct cell subtypes, including stem cells, progenitor cells, and several groups of differentiated cells. To infect specific cell subsets within the luminal cell population, the TVA technology may be used, with which avian leukosis virus-derived RCAS vectors5,10 or pseudotyped lentiviral vectors11 selectively infect the cells that express TVA in mice that carry a tva transgene under the control of a cell type-specific promoter, such as a promoter that is active only in stem cells6 or certain progenitors6,7 or alveolar cells8 or Wnt-pathway active cells9.
This protocol presents the technique of introducing genes of interest into mammary epithelial cells through intraductal injection of a viral vector. The detection of expression of the introduced genes and the resulting hyperplastic lesions and tumors are then demonstrated.
Protocol
All procedures using mice were performed in compliance with the Institutional Animal Care and Use Committee-approved animal protocol. For the present study, 9-12-week-old FVB/N or MMTV-tva female mice were used. The mice were obtained commercially or self-made (see Table of Materials). The Lenti-EGFP (FUCGW) and RCAS-Erbb2 (Neu) viruses were used. Virus preparation and titer determination were performed following the previously published reports10,12.
1. Syringe preparation
- Cut the 33 G metal hub needles (see Table of Materials) to approximately 1 cm in length. Store the needles and the 50 µL syringe in 70% alcohol after autoclaving.
- Take out syringes and needles from the alcohol. Propel the remaining alcohol out of the syringe and needle. Disassemble the syringe for air drying on an autoclaved absorbent bench pad.
- Assemble the syringe after drying.
2. Virus preparation
- Take out one or several viral stock tubes as needed from the -80 ˚C freezer and thaw the virus on ice.
NOTE: Depending on the number of cells to be infected, the virus may need to be diluted into intended titers using 1x PBS at this time. - Add bromophenol blue by dipping the pipette tip to a depth of 1 cm into the bromophenol blue powder (see Table of Materials). Then, bring the attached trace amount of bromophenol blue into the virus suspension.
NOTE: For the present study, the viral stock is usually 200 µL per tube, so the final dye concentration is approximately 0.2% (0.2 µg/100 µL). Bromophenol blue should be sterilized with microwave radiation for 45 seconds at high power of 1250 W (see Table of Materials). Ensure to carry whole procedure in a sterile environment. - Mix the bromophenol blue with the virus solution by pipetting up and down 10 times.
- Place the virus on ice and bring the ice bucket to the vivarium.
3. Animal preparation
- Anesthetize a female mouse by intraperitoneal injection of 2 µL/g of anesthetic (37.6 mg/mL ketamine, 1.92 mg/mL xylazine, and 0.38 mg/mL acepromazine, see Table of Materials). Check the depth of anesthesia with a toe pinch. Apply ointment on the eyes to prevent dryness while under anesthesia.
NOTE: The mouse must be non-responsive to toe pinch under good anesthesia. Isoflurane may also be used to anesthetize the mice. - Put the mouse in a supine position on a warm pad and attach all four limbs to the bench using adhesive tape.
- Identify one nipple (or more) to be injected (number 4 is preferred for the present study). Expose it by trimming the surrounding hair using a pair of scissors.
- Apply 70% alcohol and iodophor swabs to the nipple area in three rounds to clean and expose the nipple.
4. Intraductal injection of virus
NOTE: A magnifying lamp may be used to help visualize the nipple opening.
- Transect the distal tip of a nipple using a pair of sterile microdissection spring scissors, until a small central ductal opening can be seen under a magnifier lamp (see Table of Materials).
- Load 10 µL of virus/bromophenol blue mixture into the syringe.
NOTE: Lenti-EGFP (FUCGW) and RCAS-Erbb2 (Neu) are used in this demonstration. - Carefully insert the needle into the nipple opening with the help of the magnifier lamp. The orientation of the needle is adjusted slightly from medial to lateral to align with the main duct.
- Inject the entire 10 µL of the virus into the duct tree.
NOTE: The ducts under the skin should turn blue, if the injection is successful. Any resistance or the appearance of a localized color change indicates the failure of the injection. - Put the mouse on a slide warmer set at 45 °C until the mouse fully wakes up(~30-60 min).
5. Detection of infected cells by a fluorescent stereomicroscope
- Three to five days after injection of the virus carrying GFP or other fluorescent genes, euthanize the mouse by over-dosing it with 4 uL/g of anesthetic (37.6 mg/mL ketamine, 1.92 mg/mL xylazine, and 0.38 mg/mL acepromazine).
- Open the thoracic cavity. Cut the skin along the ventral middle line and along the upper and lower limbs using a pair of scissors. Lift the skin and expose the mammary glands.
- Remove the injected mammary gland from the skin using a pair of forceps and scissors. Also, remove an un-injected gland as a control.
- Place the mammary glands on glass slides and spread the glands to their original shape.
- Observe and image the glands under a fluorescent stereomicroscope.
Representative Results
Representative data are presented here to demonstrate successful intraductal injection, successful viral infection, and the impact of the delivered genes on mammary tumorigenesis. The amount of virus injected must be tailored to the purpose of each experiment. To illustrate how extensively the mammary duct tree can be infected, a large amount of virus carrying genes that can be imaged, such as GFP, needs to be used. On the other hand, to mimic the natural spontaneous tumorigenesis, a small amount of virus carrying an oncogene must be used so that only a few cells are infected and will evolve to precancerous lesions, and eventually invasive cancer, in a field of the otherwise completely normal mammary gland.
The success of intraductal injection can be immediately confirmed by exposing the mammary gland and observing a blue ductal tree (Figure 1). Two to five days after injection of the Lenti-EGFP (FUCGW) virus (~106 IUs)12, mammary epithelial cell infection can be assessed by whole mount preparation followed by observing under a fluorescent stereomicroscope (Figure 2). Alternatively, for flow cytometry analysis of the fluorescent proteins or cell surface markers produced by the virus6,7,19, the infected glands and non-infected glands (as negative controls) may be collected and processed into a single-cell suspension so that the rate of viral infection can be estimated (Figure 3). Another method to test/quantify virus infection is to fix the infected and non-infected control glands using 4% paraformaldehyde (or formalin), process them into paraffin-embedded blocks, and stain the resulting sections for the virally produced gene products and epitope tags such as HA and FLAG20,21.
Whether the virally infected cells will expand and form precancerous lesions, and then tumors, depends on the potency of the oncogene(s) delivered and the amount of virus injected. For a potent oncogene such as PyMT and activated RAS, early lesions form in a few days, and tumors appear in a few weeks10 (Bu et al., unpublished observations). Activated ERBB2 leads to precancerous lesions in a few weeks and tumors in a few months10,22,23 (Figure 4), while activated PIK3CA leads to tumors with a median latency of approximately 5 months24. On the other hand, Wnt1 causes tumors rather slowly: only about 20% of the infected mice developed tumors after 20 months21.
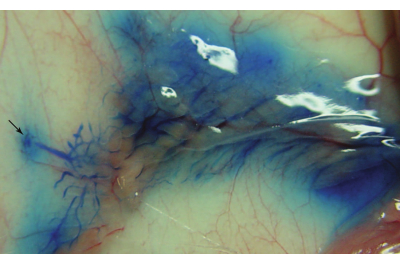
Figure 1: A successfully injected mammary ductal tree. The image was captured immediately after the intraductal injection of the number 4 mammary gland of a 9-week-old FVB/N female mouse. The arrow indicates the location of the number 4 nipple. Please click here to view a larger version of this figure.
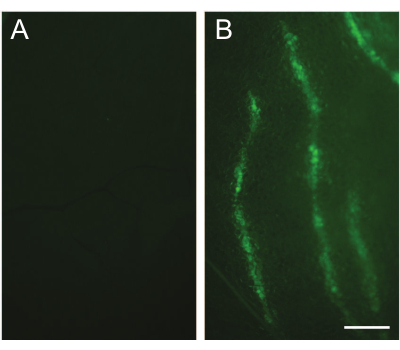
Figure 2: Detection of infected cells by fluorescent stereomicroscopy. (A) An un-injected contralateral gland is used as a control. (B) An image captured under a fluorescent stereomicroscope shows the infected mammary duct tree. The number 3 mammary gland of a 10-week-old FVB/N mouse was intraductally injected with the Lenti-EGFP (FUCGW) virus (~106 IUs). The injected mammary gland was collected 5 days after the injection. Scale bar: 1 mm. Please click here to view a larger version of this figure.
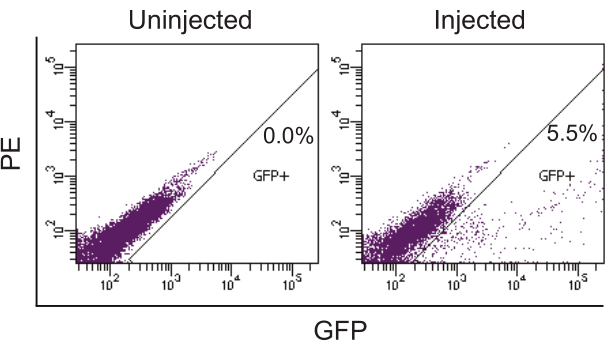
Figure 3: Quantifying infected cells by flow cytometry analysis for EGFP produced by lentivirus. The phycoerythrin (PE) channel was used to reveal the auto-fluorescent signal. The contralateral uninjected mammary glands were used as the negative control. The injected mammary glands from a 12-week-old FVB/N female mouse were collected 2.5 days after intraductal injection of Lenti-EGFP (~106 IUs/gland) and processed into a single-cell suspension. The single-cell suspension was then analyzed by flow cytometry to detect the GFP-positive cells. Please click here to view a larger version of this figure.
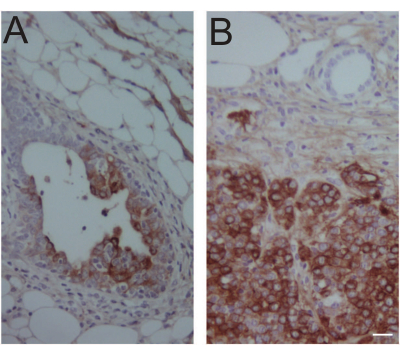
Figure 4: Immunohistochemical confirmation of virus-expressed oncogene product in an early lesion and a tumor. (A) An early lesion-containing #4 mammary gland was collected 14 days after intraductal injection of 106 IUs of RCAS-Neu (HA) into MMTV-tva mice. Immunohistochemical staining was used to detect the HA tag. (B) A tumor was collected 1 year after intraductal injection of 104 IUs of RCAS-Neu (HA) into a #4 gland of MMTV-tva mice. Mouse age at injection: 12 weeks. Scale bar: 20 µm. Please click here to view a larger version of this figure.
Discussion
This article demonstrates the viral intraductal injection technique for introducing genes into mouse mammary epithelial cells for modeling sporadic breast cancer. Usually, mice of at least 5 weeks or older are injected so that the oncogenic process starts after the mammary gland is developed. Besides, the nipple opening of mice younger than 5 weeks old is often too small for injection. On the other hand, the nipples of very old mice are sometimes degenerated, and transection may fail to reveal a ductal opening. It is also important to note that the nipples of some transgenic or knockout tumor models may also be difficult to inject due to abnormal mammary development caused by germline genetic mutations.
Besides practicing the use of standard personal protective equipment (PPE) in handling viruses, caution must be taken to avoid accidental needle stings in the experimenter's hands. While there is no evidence of avian leukosis virus infecting humans, lentiviruses used for cancer modeling in rodents can infect humans as well. This protection from accidental infection is especially important when the virus carries a potent oncogene25.
When multiple genes of interest need to be delivered into epithelial cells, they can be delivered by a mixture of different vectors carrying each individual gene or by a vector designed to carry all the genes to be tested. The former method can take advantage of previously produced viruses, but co-infection only occurs in a small subset of the infected population. On the other hand, the latter approach often requires constructing new viruses, but co-infection is guaranteed.
Compared to the genetically engineered mouse models (GEMMs), the intraductal injection technique provides better spatiotemporal flexibility to deliver the gene of interest into mammary epithelial cells. This flexibility facilitates better mimicking tumorigenesis in patients since most breast cancers originate from somatic cells that suffer genetic changes during adult stages5. Spatiotemporal control can also help to study the contribution of cell sub-types to breast tumorigenesis6,7,9,26,27,28.
The intraductal injection technique has been used mostly to deliver exogenous genes driven by artificial promoters with a viral vector. When an oncogene is delivered this way, its transcription differs from that of a naturally mutated endogenous proto-oncogene. And this difference may subsequently impact cancer formation, progression, and response to therapy. To overcome this concern, vectors carrying CRISPR/Cas9-based gene-editing components can be used to edit endogenous genes of interest29,30. We have recently improved this strategy and made it very flexible and efficient (Bu et al., unpublished results). This progress in gene editing makes the intraductal injection technique an even more powerful tool for cancer modeling.
In conclusion, intraductal injection of viral vectors is a powerful technique for generating mouse models of breast cancer that closely mimic human breast cancer formation. The combination of this technique with the TVA technology and CRISPR editing unleashes even more potential for this versatile method in understanding breast cancer formation. These models also provide valuable resources for testing new strategies in breast cancer prevention.
Disclosures
The authors have nothing to disclose.
Acknowledgements
We thank Dr. Gary Chamness for his helpful comments on this manuscript. This work was supported by the Department of Defense (DOD) CDMRP BC191649 (YL) and BC191646 (YL) as well as the National Institutes of Health (NIH) CA271498 (YL). The authors would like to thank the Breast Center Pathology Core Facility supported by SPORE P50CA186784, and the Cytometry and Cell Sorting Core supported by CPRIT-RP180672, NIH CA125123, and RR024574 with the assistance of Joel M. Sederstrom.
Materials
| Anti-HA antibody | Covance | MMS-101P | Dilution: 1 : 1000 |
| Artificial Tears | Covetrus | NDC 11695-0832-1 | |
| Bromophenol blue | Sigma | B5525 | microwave radiation for 45 seconds at power high of 1250W microwave oven |
| FACSCantoII | BD Biosciences | V96100899 | |
| Fluorescent stereomicroscope | Leica | MZ16 FA | |
| FUCGW lenti-virus | Self-made | N/A | See reference # 12 |
| FVB/N | The Jackson Laboratory | JAX:001800 | |
| Hamilton needle | Hamilton | 91033 | autoclaved |
| Hamilton syringe | Hamilton | 201000 | autoclaved |
| LED magnifying lamp | Intertek | 3165273 | |
| Micro dissection spring scissor | Roboz | RS-5621 | autoclaved |
| MMTV-tva | Self-made | See reference # 10 | |
| RCAS-Neu (HA) | Self-made | N/A | See reference # 10 |
| Rodent Comboanesthetic III | Veterinary Pharmacy | Veterinary prescription | 37.6 mg/mL ketamine, 1.92 mg/mL xylazine, and 0.38 mg/mL acepromazine |
References
- Nguyen, D. -. A., Beeman, N., Lewis, M., Schaack, J., Neville, M. C., Ip, M. M., Asch, B. B. . Methods in Mammary Gland Biology and Breast Cancer Research. Eds Margot. , 259-270 (2000).
- Gordon, J. W., Ruddle, F. H. Integration and stable germ line transmission of genes injected into mouse pronuclei. Science. 214 (4526), 1244-1246 (1981).
- Costantini, F., Lacy, E. Introduction of a rabbit beta-globin gene into the mouse germ line. Nature. 294 (5836), 92-94 (1981).
- Brinster, R. L., et al. Somatic expression of herpes thymidine kinase in mice following injection of a fusion gene into eggs. Cell. 27 (1), 223-231 (1981).
- Du, Z., Li, Y. RCAS-TVA in the mammary gland: an in vivo oncogene screen and a high fidelity model for breast transformation. Cell Cycle. 6 (7), 823-826 (2007).
- Bu, W., et al. Mammary precancerous stem and non-stem cells evolve into cancers of distinct subtypes. Cancer Research. 79 (1), 61-71 (2019).
- Bu, W., et al. Keratin 6a marks mammary bipotential progenitor cells that can give rise to a unique tumor model resembling human normal-like breast cancer. Oncogene. 30 (43), 4399-4409 (2011).
- Haricharan, S., et al. Contribution of an alveolar cell of origin to the high-grade malignant phenotype of pregnancy-associated breast cancer. Oncogene. 33 (50), 5729-5739 (2014).
- Bu, W., Zhang, X., Dai, H., Huang, S., Li, Y. Mammary cells with active Wnt signaling resist ErbB2-induced tumorigenesis. PLoS One. 8 (11), 78720 (2013).
- Du, Z., et al. Introduction of oncogenes into mammary glands in vivo with an avian retroviral vector initiates and promotes carcinogenesis in mouse models. Proceedings of the National Academy of Sciences of the United States of America. 103 (46), 17396-17401 (2006).
- Siwko, S. K., et al. Lentivirus-mediated oncogene introduction into mammary cells in vivo induces tumors. Neoplasia. 10 (7), 653-662 (2008).
- Bu, W., Xin, L., Toneff, M., Li, L., Li, Y. Lentivirus vectors for stably introducing genes into mammary epithelial cells in vivo. Journal of Mammary Gland Biology and Neoplasia. 14 (4), 401-404 (2009).
- Russell, T. D., et al. Transduction of the mammary epithelium with adenovirus vectors in vivo. Journal of Virology. 77 (10), 5801-5809 (2003).
- Wagner, S., Thresher, R., Bland, R., Laible, G. Adeno-associated-virus-mediated transduction of the mammary gland enables sustained production of recombinant proteins in milk. Scientific Reports. 5, 15115 (2015).
- Naldini, L., et al. In vivo gene delivery and stable transduction of nondividing cells by a lentiviral vector. Science. 272 (5259), 263-267 (1996).
- Coffin, J. M., Hughes, S. H., Varmus, H. E. . Retroviruses. , (1997).
- Mitani, K., Kubo, S. Adenovirus as an integrating vector. Current Gene Therapy. 2 (2), 135-144 (2002).
- McCarty, D. M., Young, S. M., Samulski, R. J. Integration of adeno-associated virus (AAV) and recombinant AAV vectors. Annual Review of Genetics. 38, 819-845 (2004).
- Bu, W., Li, Y. Intraductal injection of lentivirus vectors for stably introducing genes into rat mammary epithelial cells in vivo. Journal of Mammary Gland Biology and Neoplasia. 25 (4), 389-396 (2020).
- Dong, J., et al. Genetic manipulation of individual somatic mammary cells in vivo reveals a master role of STAT5a in inducing alveolar fate commitment and lactogenesis even in the absence of ovarian hormones. Developmental Biology. 346 (2), 196-203 (2010).
- Haricharan, S., et al. Mechanism and preclinical prevention of increased breast cancer risk caused by pregnancy. eLife. 2, 00996 (2013).
- Reddy, J. P., et al. Defining the ATM-mediated barrier to tumorigenesis in somatic mammary cells following ErbB2 activation. Proceedings of the National Academy of Sciences of the United States of America. 107 (8), 3728-3733 (2010).
- Dong, J., et al. The PR status of the originating cell of ER/PR-negative mouse mammary tumors. Oncogene. 35 (31), 4149-4154 (2016).
- Young, A., et al. Targeting the pro-survival protein BCL-2 to prevent breast cancer. Cancer Prevention Research. 15 (1), 3-10 (2022).
- Schlimgen, R., et al. Risks associated with lentiviral vector exposures and prevention strategies. Journal of Occupational and Environmental Medicine. 58 (12), 1159-1166 (2016).
- Holloway, K. R., et al. Krt6a-positive mammary epithelial progenitors are not at increased vulnerability to tumorigenesis initiated by ErbB2. PLoS One. 10 (1), 0117239 (2015).
- Holloway, K. R., et al. Targeting oncogenes into a defined subset of mammary cells demonstrates that the initiating oncogenic mutation defines the resulting tumor phenotype. International Journal of Biological Sciences. 12 (4), 381-388 (2016).
- Hein, S. M., et al. Luminal epithelial cells within the mammary gland can produce basal cells upon oncogenic stress. Oncogene. 35 (11), 1461-1467 (2015).
- Annunziato, S., et al. In situ CRISPR-Cas9 base editing for the development of genetically engineered mouse models of breast cancer. EMBO Journal. 39 (5), 102169 (2020).
- Annunziato, S., et al. Modeling invasive lobular breast carcinoma by CRISPR/Cas9-mediated somatic genome editing of the mammary gland. Genes & Development. 30 (12), 1470-1480 (2016).

