Rose Bengal-Mediated Photodynamic Therapy to Inhibit Candida albicans
Summary
The growing incidence of drug-resistant Candida albicans is a serious health issue worldwide. Antimicrobial photodynamic therapy (aPDT) may offer a strategy to fight against drug-resistant fungal infections. The present protocol describes Rose bengal-mediated aPDT efficacy on a multidrug-resistant C. albicans strain in vitro.
Abstract
Invasive Candida albicans infection is a significant opportunistic fungal infection in humans because it is one of the most common colonizers of the gut, mouth, vagina, and skin. Despite the availability of antifungal medication, the mortality rate of invasive candidiasis remains ~50%. Unfortunately, the incidence of drug-resistant C. albicans is increasing globally. Antimicrobial photodynamic therapy (aPDT) may offer an alternative or adjuvant treatment to inhibit C. albicans biofilm formation and overcome drug resistance. Rose bengal (RB)-mediated aPDT has shown effective cell killing of bacteria and C. albicans. In this study, the efficacy of RB-aPDT on multidrug-resistant C. albicans is described. A homemade green light-emitting diode (LED) light source is designed to align with the center of a well of a 96-well plate. The yeasts were incubated in the wells with different concentrations of RB and illuminated with varying fluences of green light. The killing effects were analyzed by the plate dilution method. With an optimal combination of light and RB, 3-log growth inhibition was achieved. It was concluded that RB-aPDT might potentially inhibit drug-resistant C. albicans.
Introduction
C. albicans colonizes in the gastrointestinal and genitourinary tracts of healthy individuals and can be detected as normal microbiota in about 50 percent of individuals1. If an imbalance is created between the host and the pathogen, C. albicans is capable of invading and causing disease. The infection can range from local mucous membrane infections to multiple organ failure2. In a multicenter surveillance study in the US, around half of the isolates from patients with invasive candidiasis between 2009 and 2017 is C. albicans3. Candidemia can be associated with high morbidity rates, mortality, prolonged hospital stay4. US Centers of Disease Control and Prevention reported that about 7% of all Candida blood samples tested are resistant to the antifungal drug fluconazole5. The emergence of drug-resistant Candida species raises the concern to develop an alternative or adjuvant therapy to antimycotic agents.
Antimicrobial photodynamic therapy (aPDT) involves activating a specific photosensitizer (PS) with light at the peak absorption wavelength of the PS6. After excitation, the excited PS transfers its energy or electrons to the nearby oxygen molecules and returns to the ground state. During this process, reactive oxygen species and singlet oxygen are formed and cause cell damage. aPDT has been widely used to kill microorganisms since the 1990s7. One of the benefits of aPDT is that multiple organelles are damaged in a cell by singlet oxygen and/or reactive oxygen species (ROS) during irradiation; thus, resistance to aPDT has not been found till today. Moreover, a recent study reported that the bacteria that survived after aPDT became more sensitive to antibiotics8.
The light sources used in aPDT include lasers, metal halogen lamps with filters, near-infrared light, and light-emitting diode (LED)9,10,11,12. The laser provides a high light power, usually larger than 0.5 W/cm2, that allows for the delivery of a high light dose in a very short time. It has been widely used in cases where a longer treatment time is inconvenient such as aPDT for oral infections. The drawback of a laser is that its spot size of illumination is small, ranging from a few hundred micrometers to 10 mm with a diffuser. Moreover, laser equipment is expensive and needs specific training to operate. On the other hand, the irradiation area of a metal halogen lamp with filters is relatively larger13. However, the lamp is too hefty and expensive. LED light sources have become mainstream of aPDT in the dermatologic field because it is small and less expensive. The irradiation area can be relatively large with an array arrangement of the LED light bulb. The whole face can be illuminated at the same time9. Nevertheless, most, if not all, LED light sources available today are designed for clinical use. It may not be suitable for experiments in a lab because it is space-occupying and expensive. We developed an inexpensive LED array that is very small and can be cut and assembled from a LED strip. The LEDs can be fitted into different arrangements for different experimental designs. Different conditions of aPDT can be completed in a 96-well plate or even a 384-well plate in one experiment.
Rose bengal (RB) is a colored dye widely used to enhance visualization of corneal damages in human eyes14. RB-mediated aPDT has shown killing effects on Staphylococcus aureus, Escherichia coli, and C. albicans with roughly comparable efficiency to that of Toluidine blue O15. This study demonstrates a method to validate the effect of RB-aPDT on multidrug-resistant C. albicans.
Protocol
1. aPDT system preparation
- Cut four green light-emitting diodes (LEDs) from a LED strip (see Table of Materials) and align them with four wells of a 96-well plate (Figure 1).
NOTE: The LEDs were arranged into a 4 x 3 array. The back of the LED was adhered to a heat sink to disperse heat during irradiation. - Measure the fluence rate11 of the LED at 540 nm with a light power meter (see Table of Materials). See Supplementary Figure 1 to ensure that the fluence rate of the LED is between 510-560 nm.
- Put an electric fan alongside the plate during irradiation to maintain the constant temperature (25 ± 1 °C)11. See Supplementary Figure 2 to ensure that the constant temperature of the medium is maintained during irradiation.
2. Culturing of the yeast form of C. albicans
NOTE: A multidrug-resistant C. albicans (BCRC 21538/ATCC 10231), resistant to most antifungals, including fluconazole, is used for the experiments16.
- Determine the antimycotic drug sensitivity with a disk diffusion method following previously published report17.
- Grow C. albicans in yeast, hyphae, and pseudohyphae forms depending on the micro-ecological environments18.
NOTE: The hyphae and pseudohyphae forms are difficult for an accurate calculation. The yeast form can be calculated precisely under a microscope or with flow cytometry. The temperature during cell growth determines its morphology. At room temperature (25 °C), nearly all cells are yeast form. A 4 h short incubation of C. albicans at 30 °C did not affect its yeast morphology.
3. aPDT on planktonic C. albicans
- Isolate a single colony of C. albicans from an agar plate with a sterile loop and add it to a 3 mL yeast extract peptone dextrose (YPD) medium (see Table of Materials) in a sterilized glass tube.
- Incubate the tube at 25 ± 1 °C overnight (14-16 h) in an incubator with a rotation speed of 155 rpm to expand C. albicans and maintain the fungus in yeast form for accurate quantification.
- Dilute the overnight culture with medium to an OD600 value of around 0.5 at 30° C and rotate at a speed of 155 rpm for 4 h to achieve a log growth phase of C. albicans.
- Dilute the log phase culture again with fresh YPD medium to an OD600 value of 0.65 (around 1 x 107 colony forming units, CFU/mL). Confirm the final concentration by serial dilution method on an agar plate8.
- Prepare a stock solution (4%) of Rose bengal (RB) by dissolving the powder in 1x PBS. Filter and sterilize it with a 0.22 µm filter and store it at 4 °C in the dark. The final working concentration of RB is 0.2%.
- Add 111 µL of 2% RB to 1 mL of log-phase C. albicans in a 1.5 mL microcentrifuge tube and co-culture at different time points (0, 15, and 30 min) at room temperature to understand the absorption of RB in the cells (Figure 2).
- Wash the co-culture three times with 1 mL of 1x PBS with centrifugation at 16,100 x g for 2.5 min at room temperature.
NOTE: aPDT contains four different conditions: absolute control (no light exposure, no RB), dark control (no light but incubates with RB), light control (exposes to light without RB), aPDT (exposes to light in the presence of RB). - Resuspend the C. albicans in 1 mL of 1x PBS and allocate them into three different wells in a 96 well plate for each condition. Align the wells with the LED array after washing.
- In light exposed groups, turn on the electric fan and light.
NOTE: A different fluence (J/cm2) can be achieved by exposing the wells to varying time periods. For example, a 16.7 min light exposure comes to 10 J/cm2 with a 10 mW/cm2 LED light bulb. - After irradiation, add 20 µL of the co-culture solution from one well to a 1.5 mL centrifuge tube containing 180 µL of 1x PBS to prepare a 10x dilution. Further, dilute ten times, subsequently following the same method.
- Drop three drops of 20 µL of each serial dilution onto one quadrant of a YPD agar plate to achieve countable colonies the plate. Calculate the CFU/mL by multiplying the colonies with the dilution factors3.
4. Statistical analysis
- Analyze the collected data using a graphing and statistics software (see Table of Materials).
- Depict data by mean ± standard error of the mean. Perform a two-way ANOVA analysis of variance8 to evaluate significant differences between the different test conditions.
- Perform Tukey's multiple comparison tests for pairwise comparisons8. For each different treatment, perform at least three independent experiments. Consider p-value < 0.05 statistically significant.
Representative Results
Figure 1 shows the aPDT system being used in the present study. Since high temperatures may cause significant cell death, the LED array is cooled by an electric fan, and a heat sink is used during irradiation to maintain a constant temperature at 25 ± 1 °C. The heat effect can be discounted. Having an even light distribution is also an important determining factor for a successful aPDT; therefore, it is critical to align the LED light bulb to the well precisely during illumination. Due to the brightness of the LED, sunglasses need to be equipped before turning on the light.
C. albicans is stained immediately with RB as visualized by red fluorescence under fluorescent microscopy (0 min in Figure 2). It can be seen that the RB enters the cells in a time-dependent manner (Figure 2). The study used a 15 min RB incubation at which, after 15 min, most of the cells were stained with RB. A higher concentration of RB leads to a stronger fluorescence, producing more free radicals to kill fungi. Yet, it may also cause significant cell death in normal cells; therefore, 0.2% RB concentration is commonly used in clinics. Thus, that exact concentration was chosen in this study.
PDT involves the activation of RB with light. When the activated RB returns to its ground state, it transfers the energy and electrons to the nearby oxygen to generate free radicals and singlet oxygen, resulting in cell death. Figure 3 shows no cell death under the condition of no irradiation or absence of RB. C. albicans was inhibited in a light dose-dependent manner after green light irradiation in the presence of 0.2% RB (Figure 3). Exposing the fungi to green light with 30 J/cm2 resulted in a 4-log (99.99%) inhibition of cell growth.
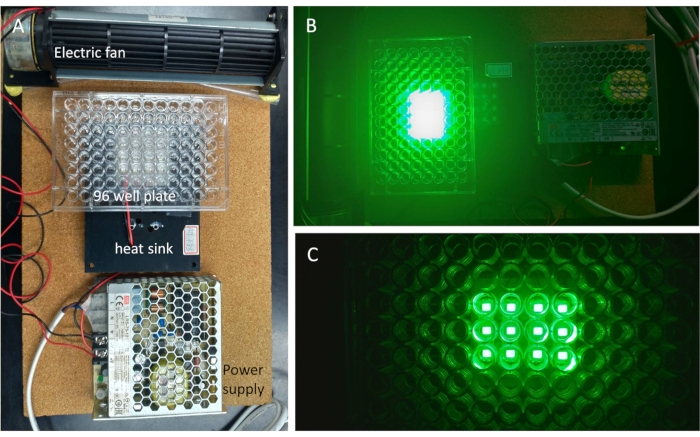
Figure 1: The photodynamic system. (A) A green LED array was adhered to a metal heat sink to disperse heat during irradiation. An electric fan was put alongside the light source to keep the temperature constant at 25 ± 1 °C. (B) The light was turned on. (C) The wells of a 96 well plate were aligned with the center of the LED. Please click here to view a larger version of this figure.
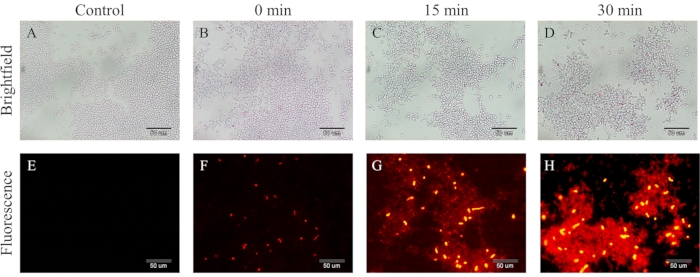
Figure 2: The time-dependent study of Rose bengal entering C. albicans. Bright-field (A–D) and fluorescence images (E–H) of the C. albicans after 0-30 min co-cultured with 0.2% Rose bengal (RB). (A) and (E) Control without RB co-cultured. (B) and (F) The cells were immediately stained with 0.2% RB. (C) and (G) After 15 min of culture, most cells showed red fluorescence, indicating RB inside the cells. (D) and (H) Stronger fluorescence of the RB was noted with a 30 min incubation. Scale bar = 50 µm. Please click here to view a larger version of this figure.
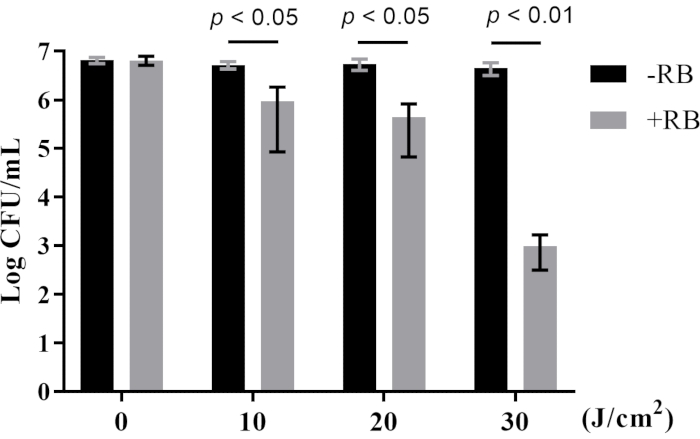
Figure 3: Antimicrobial photodynamic therapy effects on multidrug-resistant C. albicans. The growth inhibition of cells depends on the light fluence. Exposing C. albicans to a fluence of 10 J/cm2 inhibited cell growth by 1.5 logs, by 2 logs with 20 J/cm2, and 4 logs with 30 J/cm2 respectively in the presence of 0.2% Rose bengal. -RB, without Rose bengal incubation; +RB, co-cultured with Rose bengal for 15 min. Data are means ± SEM of three separate experiments performed in duplicate. p values are indicated in the figure (Tukey's multiple comparison tests, two-way ANOVA). Please click here to view a larger version of this figure.
Supplementary Figure 1: The LED output spectrum. The fluence rate was measured every 2 nm from 510-560 nm with a power meter. Data are pooled from two independent experiments with triplicate measurements. Please click here to download this File.
Supplementary Figure 2: The temperature of the medium during irradiation. A thermocouple was inserted into each well of a 96-well plate filled with 100 µL broth to measure the temperature. The temperature was constant at 25 ± 1 °C. Data are pooled from duplicated experiments with triplicate wells. Please click here to download this File.
Discussion
Encouraging results of clinical applications of RB-PDT for fungal keratitis have been reported recently19. The absorption peak of RB is at 450-650 nm. It is essential to determine the fluence rate of the light source for a successful aPDT. A high fluence (usually >100 J/cm2) is required to treat cancer cells, while a lower fluence is expected to treat infected lesions6. A high fluence means a long exposure time which may not be practical in a clinical setting. For treating mycotic keratitis, a 5.4 J/cm2 is agreed in the ophthalmologic community20. A long incubation time of RB is also inconvenient for a patient to receive aPDT treatment. Thus, a 15 min incubation time was chosen for further experiments.
Some steps are critical for a successful experiment. The agar plates used for fungal culture were dried for 15-20 min in a lamellar flow cabin with the fan turned on to reduce moisture on the surface. A moist surface would allow for the flow of the fungi droplets to mix, preventing the formation of a single colony.
Executing all experiments in dim light is vital to keep RB from photobleaching. The electric circuit was in a parallel connection so that if a break happened in one of the circuits, the remaining appliances would not be affected. If there are results that out-range of others, the array can be checked first to ensure all LED light bulbs are in good function.
One limitation of utilizing a LED light source is its temperature dependence. In a LED, heat is not produced by the LED light bulb itself but generated at the semiconductor junction within the device9. Since overdriving LEDs above their rated current evokes the rising of the junction temperature, eventually leading to premature failure of the light bulb, it is necessary to equip the device with a metal heat sink to provide suitable cooling of the junction. Another limitation of the LED array's present design is the restricted area illuminated by each LED light bulb, which only accommodates one single well of a 96-well plate. If a larger illumination area is needed, a different arrangement of LED bulbs with proper corresponding distances above or below the plate is necessary to achieve even illumination.
The advantages of this study design are the ease and inexpensive setup of the photodynamic system for aPDT experiments. It can be used in experiments concerning fungal infections. Viruses and bacteria can also be tested in the same system. The LED light strip can be chosen from a different color of light to correlate with the absorption peaks of different photosensitizers, ranging from visible to near-infrared light spectrum. They can be easily purchased from the market. The strip can be cut and assembled into different arrays to align with a 96-well plate for a high throughput assay. The use of a 96-well plate allows different testing conditions at the same time to save time and space in the lab.
In conclusion, the established system in this study is simple, easy, and versatile to examine different photodynamic effects on various microorganisms and cells.
Divulgaciones
The authors have nothing to disclose.
Acknowledgements
This work has received funding from the Center of Applied Nanomedicine, National Cheng Kung University from the Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE), and Ministry of Science and Technology, Taiwan [MOST 109-2327-B-006-005] to TW Wong. J.H. Hung acknowledges funding from National Cheng Kung University Hospital, Taiwan [NCKUH-11006018], and [MOST 110-2314-B-006-086-MY3].
Materials
| 1.5 mL microfuge tube | Neptune, San Diego, USA | #3745.x | |
| 5 mL round-bottom tube with cell strainer cap | Falcon, USA | #352235 | |
| 96-well plate | Alpha plus, Taoyuan Hsien, Taiwan | #16196 | |
| Aluminum foil | sunmei, Tainan, Taiwan | ||
| Aluminum heat sink | Nanyi electronics Co., Ltd., Tainan, Taiwan | BK-T220-0051-01 | |
| Centrifuge | Eppendorf, UK | 5415R | disperses heat from the LED array |
| Graph pad prism software | GraphPad 8.0, San Diego, California, USA | graphing and statistics software | |
| Green light emitting diode (LED) strip | Nanyi electronics Co., Ltd., Tainan, Taiwan | 2835 | |
| Incubator | Yihder, Taipei, Taiwan | LM-570D (R) | Emission peak wavelength: 525 nm, Viewing angle: 150°; originated from https://www.aliva.com.tw/product.php?id=63 |
| Light power meter | Ophir, Jerusalem, Israel | PD300-3W-V1-SENSOR, | |
| Millex 0.22 μm filter | Merck, NJ, USA | SLGVR33RS | |
| Multidrug-resistant Candida albicans | Bioresource Collection and Research CenterBioresource, Hsinchu, Taiwan | BCRC 21538/ATCC 10231 | http://catalog.bcrc.firdi.org.tw/BcrcContent?bid=21538 |
| OD600 spectrophotometer | Biochrom, London, UK | Ultrospec 10 | |
| Rose Bengal | Sigma-Aldrich, MO, USA | 330000 | stock concentration 40 mg/mL = 4%, prepare in PBS, stored at 4 °C |
| Sterilized glass tube | Sunmei Co., Ltd., Tainan, Taiwan | AK45048-16100 | |
| Yeast Extract Peptone Dextrose Medium | HIMEDIA, India | M1363 |
Referencias
- Naglik, J. R., Challacombe, S. J., Hube, B. Candida albicans secreted aspartyl proteinases in virulence and pathogenesis. Microbiology and Molecular Biology Reviews. 67 (3), 400-428 (2003).
- Pappas, P. G., et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clinical Infectious Diseases. 62 (4), 1-50 (2016).
- Ricotta, E. E., et al. Invasive candidiasis species distribution and trends, United States, 2009-2017. Journal of Infectious Diseases. 223 (7), 1295-1302 (2021).
- Koehler, P., et al. Morbidity and mortality of candidaemia in Europe: an epidemiologic meta-analysis. Clinical Microbiology and Infection. 25 (10), 1200-1212 (2019).
- Toda, M., et al. Population-based active surveillance for culture-confirmed candidemia – four sites, United States, 2012-2016. Morbidity and Mortality Weekly Report Surveillance Summaries. 68 (8), 1-15 (2019).
- Lee, C. N., Hsu, R., Chen, H., Wong, T. W. Daylight photodynamic therapy: an update. Molecules. 25 (21), 5195 (2020).
- Wainwright, M. Photodynamic antimicrobial chemotherapy (PACT). Journal of Antimicrobial Chemotherapy. 42 (1), 13-28 (1998).
- Wong, T. W., et al. Indocyanine green-mediated photodynamic therapy reduces methicillin-resistant staphylococcus aureus drug resistance. Journal of Clinical Medicine. 8 (3), 411 (2019).
- Kim, M. M., Darafsheh, A. Light sources and dosimetry techniques for photodynamic therapy. Photochemistry and Photobiology. 96 (2), 280-294 (2020).
- Wong, T. W., Sheu, H. M., Lee, J. Y., Fletcher, R. J. Photodynamic therapy for Bowen’s disease (squamous cell carcinoma in situ) of the digit. Dermatologic Surgery. 27 (5), 452-456 (2001).
- Wong, T. W., et al. Photodynamic inactivation of methicillin-resistant Staphylococcus aureus by indocyanine green and near infrared light. Dermatologica Sinica. 36 (1), 8-15 (2018).
- Stasko, N., et al. Visible blue light inhibits infection and replication of SARS-CoV-2 at doses that are well-tolerated by human respiratory tissue. Scientific Reports. 11 (1), 20595 (2021).
- Crosbie, J., Winser, K., Collins, P. Mapping the light field of the Waldmann PDT 1200 lamp: potential for wide-field low light irradiance aminolevulinic acid photodynamic therapy. Photochemistry and Photobiology. 76 (2), 204-207 (2002).
- Feenstra, R. P., Tseng, S. C. Comparison of fluorescein and rose bengal staining. Ophthalmology. 99 (4), 605-617 (1992).
- Demidova, T. N., Hamblin, M. R. Effect of cell-photosensitizer binding and cell density on microbial photoinactivation. Antimicrobial Agents and Chemotherapy. 49 (6), 2329-2335 (2005).
- Shahid, H., et al. Duclauxin derivatives from fungi and their biological activities. Frontiers in Microbiology. 12, 766440 (2021).
- Arendrup, M. C., Park, S., Brown, S., Pfaller, M., Perlin, D. S. Evaluation of CLSI M44-A2 disk diffusion and associated breakpoint testing of caspofungin and micafungin using a well-characterized panel of wild-type and fks hot spot mutant Candida isolates. Antimicrobial Agents and Chemotherapy. 55 (5), 1891-1895 (2011).
- Mukaremera, L., Lee, K. K., Mora-Montes, H. M., Gow, N. A. R. Candida albicans yeast, pseudohyphal, and hyphal morphogenesis differentially affects immune recognition. Frontiers in Immunology. 8, 629 (2017).
- Hung, J. H., et al. Recent advances in photodynamic therapy against fungal keratitis. Pharmaceutics. 13 (12), 2011 (2021).
- Martinez, J. D., et al. Rose Bengal photodynamic antimicrobial therapy: a pilot safety study. Cornea. 40 (8), 1036-1043 (2021).

