Barrier Functional Integrity Recording on bEnd.3 Vascular Endothelial Cells via Transendothelial Electrical Resistance Detection
Summary
This protocol describes a dependable and efficient in vitro model of the brain blood barrier. The method uses mouse cerebral vascular endothelial cells bEnd.3 and measures transmembrane electrical resistance.
Abstract
The blood-brain barrier (BBB) is a dynamic physiological structure composed of microvascular endothelial cells, astrocytes, and pericytes. By coordinating the interaction between restricted transit of harmful substances, nutrient absorption, and metabolite clearance in the brain, the BBB is essential in preserving central nervous system homeostasis. Building in vitro models of the BBB is a valuable tool for exploring the pathophysiology of neurological disorders and creating pharmacological treatments. This study describes a procedure for creating an in vitro monolayer BBB cell model by seeding bEnd.3 cells into the upper chamber of a 24-well plate. To assess the integrity of cell barrier function, the conventional epithelial cell voltmeter was used to record the transmembrane electrical resistance of normal cells and CoCl2-induced hypoxic cells in real-time. We anticipate that the above experiments will provide effective ideas for the creation of in vitro models of BBB and drugs to treat disorders of central nervous system diseases.
Introduction
BBB is a unique biological interface between blood circulation and nerve tissue, which is composed of vascular endothelial cells, pericytes, astrocytes, neurons, and other cellular structures1. The flow of ions, chemicals, and cells between the blood and the brain is strictly regulated by this barrier. This homeostasis safeguards the nervous tissues against toxins and pathogens while also enabling the appropriate operation of the brain's nerves2,3. Maintaining the integrity of the BBB can effectively prevent the development and progression of disorders affecting the central nervous system, such as neuronal dysfunction, edema, and neuroinflammation4. However, the unique physiological properties of the BBB prevent more than 98% of small molecule medications and 100% of macromolecular pharmaceuticals from entering the central nervous system5. Therefore, increasing the penetration of medications through the BBB during the development of drugs for the central nervous system is essential for achieving therapeutic efficacy6,7. Even though computer simulation screening of substrates has significantly raised the probability of drug candidates crossing the BBB, reliable and affordable in vitro/in vivo BBB models are still needed to meet the needs of scientific research8.
A quick and affordable technique for high-throughput drug screening is the in vitro model9. To shed light on the fundamental processes of medicines' effects on BBB function and their part in the development and progression of disease, a series of simplified in vitro BBB models has been created. At present, the common in vitro BBB models are the monolayer, co-culture, dynamic, and microfluidic models10,11,12, constructed by vascular endothelial cells and astrocytes, pericytes, or microglia13,14. Although 3D cell cultures are morein line with the physiological structure of BBB15, their application as a means of drug screening for BBB is still constrained by their intricate design and subpar reproducibility. In contrast, the monolayer in vitro model is the one most frequently used to research the BBB and is applicable for determining the expression of membrane transporters and tight junction proteins in particular cells.
Transmembrane electrical resistance (TEER) measurement is a technique to evaluate and monitor the layer of cells across the resistance and evaluate the cell integrity and permeability of the barrier. By simultaneously inserting two electrodes into the growth medium or buffer solution on either side of the monolayer, it is possible to measure the alternating current or electrical impedance through the cell's compact layer16,17. In order to determine whether the in vitro BBB model has been properly created, the measurement of TEER will usually be employed as the gold standard18. On the other hand, the trend of medication action on BBB permeability can be accurately predicted by measuring the change in electrical resistance of the cell layer after drug involvement19. For example, Feng et al. discovered that catalpol (the primary active monomer of rehmanniae) could effectively reverse the lipopolysaccharide-induced down-regulation of tight junction proteins in the BBB and raise the TEER value of the mouse brain endothelial cell layer20.
The neuroinflammatory response is usually the main cause of BBB homeostasis imbalance21. Hypoxic treatment to induce neuroinflammatory injury is the main method to destroy the blood-brain barrier, mainly including physical methods and chemical reagent methods. The former primarily utilizes a three-gas incubator to vary the oxygen content in the cell growth environment to simulate hypoxic conditions22,while the latter is achieved by artificially introducing deoxy reagents such as CoCl2 to the cell culture medium23. The cells will remain in a deoxygenated condition if Fe2+ is substituted for Co2+ in the heme. If Fe2+ is substituted for Co2+ in the catalytic group, proline hydroxylase and aspartate hydroxylase activity will be inhibited, resulting in an accumulation of hypoxia-inducible factor-1α (HIF-1α)24. Under persistent hypoxia, the dephosphorylation of HIF-1α in the cytoplasm triggers cell death and activates vascular endothelial growth factor, which ultimately raises vascular permeability. In previous studies25,26, it has been well demonstrated that hypoxia can significantly reduce the expression of endothelial tight junction proteins to increase the permeability of BBB. In this study, the time-resistance curve of bEnd.3 cells seeded in 24-well plates were measured in order to create a straightforward BBB model. Using this model, we characterized the changes in cell TEER after CoCl2 intervention in order to construct a cell model that can be used to screen drugs for BBB protection.
Protocol
NOTE: Mouse brain-derived Endothelial cells.3 (bEnd.3) were inoculated into the chambers of a 24-well plate to construct a simple in vitro model of BBB under specific medium conditions. The TEER of normal cells and hypoxic cells were measured by TEER meter (Figure 1 and Figure 2).
1. Solution preparation
- Prepare the DMEM cell culture medium containing FBS (10%, v/v), 100 U/mL penicillin, and 10 mg/mL streptomycin (see Table of Materials).
- Prepare 100 mM CoCl2 stock solution by adding 1.30 mg CoCl2 to 100 µL DMSO solution.
NOTE: All the above solutions were stored at 4 °C condition, and the stock solution was diluted according to the desired concentration before use. - Prepare 5% sodium hypochlorite solution (v/v) by adding 2 mL of sodium hypochlorite solution to 38 mL of double distilled water.
2. Cell culture and cell viability
- Seed 1 mL of bEnd.3 cells in culture dish (100 mm) containing DMEM medium at a density of 1 x 106 cells/mL and culture at 37 °C in a humidified atmosphere of 5% CO2. Change the medium every 2 to 3 days and subculture the cells 2x a week.
- After bEnd.3 cells grow to 80 % confluence, digest the cells with 0.25% trypsin for 30 s.
- Make a suspension of bEnd.3 cells at density of 7 x 104 cells/mL using DMEM medium through a cell counter. Then, seed 100 µL of bEnd.3 cell suspension in a 96-well plate.
- After cell adhesion, clean the cells with PBS and culture the cells with 100 µL of culture medium or drug-containing medium (100 µM, 200 µM, 300 µM, 400 µM, 500 µM CoCl2) for 24 h under the same conditions. After removing the medium inside the well plate and cleaning it with PBS, add 100 µL of CCK-8 solution.
NOTE: Do not generate bubbles in the well, which will affect the values of optical density (OD). - Put 96-well plates at 37 °C environment and incubate for 1 h. Measure the absorbance of the 96-well plates at 450 nm using a microplate reader.
NOTE: To avoid intra-group differences, the well plates were cooled to room temperature before detection. - Calculate the cell viability induced by different concentrations of CoCl2 according to the formula [ODDrug – ODBlank] / [ODControl-ODBlank] x 100%. Select the CoCl2 concentration with a significant difference in cell viability reduction compared with the control group for the next experiment.
3. Model assembly
- Rinse the upper chamber of the 24-well plates with PBS.
NOTE: Cells grew and fused at the bottom of the upper chamber of the 24-well plate, and tight junctions between cells gradually formed to play a barrier role. If the endothelial cells used in some studies are not able to form a complete barrier on PET membranes independently, coating the membranes with collagen IV solution is required prior to cell inoculation. - Mix the bEnd.3 cells with DMEM medium to make a suspension at a density of 5 x 105 cells/mL using a vortex mixer. Then, seed 200 µL of bEnd.3 cell suspension on the PET membrane in the upper chamber of a 24-well plate (0.33 cm2, 0.4 µm membrane pore size).
NOTE: The pilot study of this protocol found no difference in results when using 5 to 10 passages of bEnd.3 cells for experiments. To ensure the probability of successful modeling, please refer to the cell number interval of this protocol. - Add 1200 µL of complete medium to the lower chamber of the plate to ensure that the osmotic pressure of the upper and lower chambers tends to stabilize. There are differences in the volume of medium added depending on the type; ensure that the liquid level of the upper and lower chambers is flush.
- Change the medium of the upper chamber and the lower chamber at a fixed time every day and monitor the resistance value at the same time.
- When changing the medium, the integrity of the cell layer will be damaged by artificial touch or excessive movement. To avoid the above situation, slowly remove the old medium from one side with a negative pressure pipette and slowly add a new medium along the wall during fluid exchange.
4. Measurement of TEER
- Before work begins, place the resistor, 5% sodium hypochlorite solution, 75% ethanol, and double distilled water solution in an ultra-clean table. Turn on the UV irradiation for 30 min to eliminate residual bacteria and pathogens.
- Place the electrodes in 5% sodium hypochlorite solution with slow shaking for 3 s to 5 s, and then immerse in 75% ethanol for 15 min. Finally, transfer to PBS or double distilled water solution until use.
- Turn ON the switch on the back of the cell resistor meter, click Select Plate according to the parameters in Table 1, and select 24-Well Plate.
- According to the operation needs, select the appropriate detection sequence. We selected A1 procedure in this study.
- Insert a kΩ resistor into the right plug to calibrate the instrument. If the calibration result is 1000 ± 5 Ω, consider the accuracy of the instrument to be normal.
- If the calibration result is not 1000 Ω, click on Mode Units on the main interface to select OHMS, and then click Calibrate on the main screen to re-calibrate the instrument.
- Pull out the kΩ resistor on the right side and replace the measuring electrode with a connecting wire.
- Place the electrode into the 24-well plate without seeding cells vertically and click Blank Handling on the main screen of the instrument. The background value of the plate resistance without seeded cells is about 134.4 Ω.
- Insert the two electrodes into the upper and lower chambers of the seeded plate with cells so that the cell layer is between them, and then record the resistance value by gently stepping on the Pedal.
- Make sure that the electrode does not touch the cells in the upper chamber and the bottom of the lower chamber. The soaking time of the electrode in the solution has no effect on the resistance value, and it is only necessary to make sure that the electrode is in the correct position.
- Obtain TEER values (Ωcm2) by multiplying electrical resistance values (ohms) with the bottom area (cm2) of the upper chamber, as in the equation:
TEER (Ωcm2) = Resistance (Ω) x Sinsert (cm2) - Draw a line plot of TEER-Time (in days). When the resistance value does not increase further with time (measured over days), consider the cell formed a barrier.
NOTW: The monolayer BBB model of bEnd.3 cells will be successfully constructed by culturing bEND.3 cells with the parameters in this study for about 6 days. The TEER of bEnd.3 cell monolayer model ranged from 16.49 ± 2.12 Ωcm2 to 27.59 ± 1.50 Ωcm2 within 6 days (n=8, mean ± SD).
5. Barrier destruction and statistical analysis
- According to the TEER – time curve, select the wells with barrier function and divide them into the control group and CoCl2 group (n = 4).
- Add the culture medium and culture medium containing 300 µM CoCl2 (200 µL) into the control group and CoCl2 group upper chamber, respectively.
- Detect the resistance values of the control and CoCl2 groups at 12 h and 24 h of incubation at 37 °C using the procedure described in step 4.
- Use commercial software to map the trend of TEER values of the barrier of cells cultured with or without 300 µM CoCl2.
- Use statistical analysis software to analyze the difference in resistance values between CoCl2-treated cells and normal cells (n=4, *p<0.05, **p<0.01, ***p<0.001).
Representative Results
This protocol allowed the recording of changes in the resistance values of cells according to the parameters set in the transendothelial resistor meter. The viability of bEnd.3 cells (number of live cells) treated with different concentrations of CoCl2 were screened by CCK-8 assay. Greater cell damage produced by CoCl2 was represented by lower cell viability. We found that 300 µM of CoCl2 was significantly cytotoxic in vitro, and this concentration was used for the next experiments (Figure 3A). By monitoring the growth resistance changes in bEnd.3, we found that the cell TEER values began to stabilize on the 5th day. Hypoxic injury induced by the addition of 300 µM CoCl2 to the upper chamber of the plate on the 6th day resulted in a significant decrease in TEER values compared to the control at both the 12 h and 24 h time points (Figure 3B). The function of the cell barrier can be indirectly assessed by the TEER value, and a decline in the TEER value indicates the breakdown of the cell barrier. The TEER value of 300 µM CoCl2 group dropped in comparison to the control group after incubation for 24 h. (Figure 3C).The aforementioned research demonstrated that damage to the BBB in vitro model can be caused by a hypoxic environment caused by CoCl2.
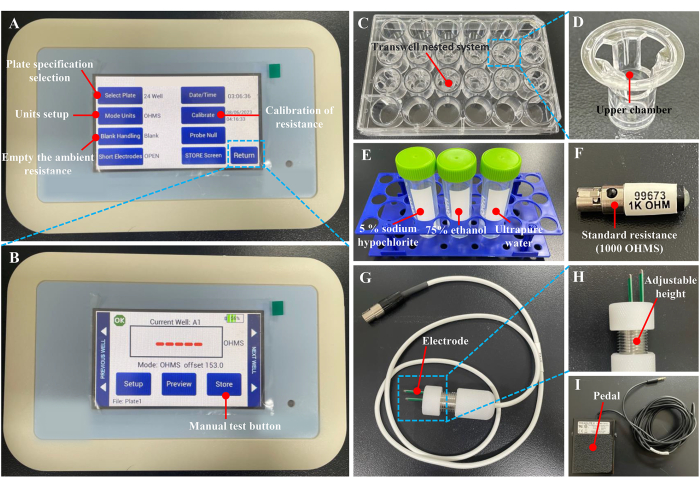
Figure 1: Instruments and accessories for measuring TEER. (A-B) Operation main interface of the TEER meter. (C-D) A 24-well plate. (E) The solution required for electrode cleaning and disinfection. (F) Standard resistance is required for the calibration of the TEER meter. (G-H) The electrode and local magnification. (I) Foot pedal was used to collect data. Please click here to view a larger version of this figure.
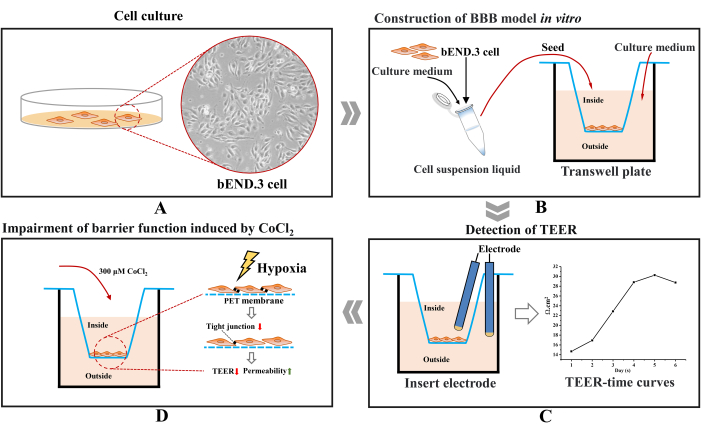
Figure 2: Flow charts of the transmembrane resistance of bEnd.3 cells recorded using a transendothelial resistor meter. (A) Cell culture. (B) The bEnd.3 cells were seeded in the upper chamber of the plates, and a dense cell barrier was formed by filling the well plates with medium to support their growth and differentiation. (C) The barrier functional integrity of the cells was assessed by monitoring TEER. (D) CoCl2 was used to mimic the hypoxic environment to induce impaired cell barrier function. Please click here to view a larger version of this figure.
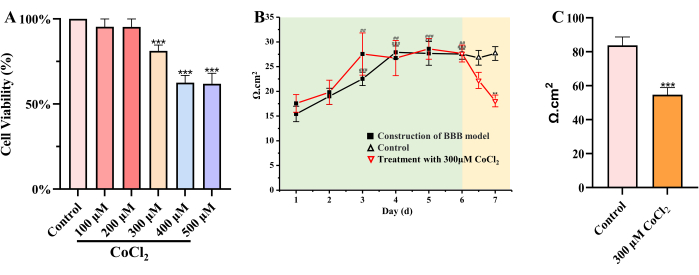
Figure 3: Salidroside maintains the integrity of the barrier function of bEnd.3 cells by alleviating CoCl2-induced hypoxic injury. (A) Effect of CoCl2 (100 µM, 200 µM, 300 µM, 400 µM, 500 µM) on the viability of bEnd.3 cells (n=6, CoCl2 group vs control group ***p<0.001, mean ± SD). (B) Plot of changes in TEER values of bEnd.3 cells treated with normal medium or 300 µM CoCl2(n=4, Day 1 vs Day 2-6: ##p<0.01, ###p<0.001, Day 6 vs Day 6.5 – 7: **p<0.01, mean ± SD). (C) TEER changes of cells after 24 h hypoxic injury (n=4, CoCl2 group vs control group ***p<0.001, mean ± SD). One-way ANOVA and Tukey's test were performed, and p<0.05 was considered significant. Please click here to view a larger version of this figure.
| Parameters | Option |
| Select plate | 24-Well |
| Detection ordering | A1 |
| Mode Units | Ω |
| Standard resistance | 1 kΩ |
Table 1: Set parameters of TEER meter. The parameter settings and program selection of the instrument are required for the detection of cell resistance.
Discussion
One of the most developed bodily organs, the brain controls a wide range of intricate physiological processes, including memory, cognition, hearing, smell, and movement27. The brain is one of the human body's most complicated and diseased organs at the same time. The occurrence of many central nervous system disorders shows a growing tendency year over year due to factors including air pollution, irregular eating patterns, and other factors27,28,29. It is interesting that the beginning and progression of some central nervous system diseases, such as stroke, epilepsy, and Alzheimer's disease (AD), are closely correlated with the growth of BBB30,31,32. The basic concept for the treatment of the majority of disorders with brain dysfunction may be the creation of new therapies or medications to maintain BBB functional homeostasis. Unfortunately, most medicines cannot enter the brain parenchyma to perform their vital functions due to the BBB's hydrophobicity and its unique solute transport method14,33. To increase the likelihood that a medicine will be successful, it is a good strategy to create new BBB models that can be utilized for high-throughput molecular screening.
Due to the intricate structure of the neurovascular unit, the in vivo model theoretically has a higher degree of modeling of the BBB structure. However, due to the restriction of homology between animals and humans, the variances in BBB transporters may lead to medication screening not having the expected outcome34. On the contrary, in vitro models offer the advantages of being inexpensive, having a quick detection cycle, and being able to be utilized for high-throughput screening, which can better serve the objectives of neurological disease research. With the development of science and technology, more and more in vitro models that closely resemble the physiological structure of the BBB are being created and enhanced. In addition to the distinction between simulation techniques for static and dynamic platforms, there are significant differences in the cell types and numbers used35. Seeding endothelial cells at the bottom of the upper chamber is the simplest BBB cell model and an excellent approach for transport kinetics and cell signaling pathway36. Co-culture models add interactions with pericytes or glial cells on the foundation of monolayer cells, but these models are frequently constrained by the inability to obtain accurate cell positioning and directed control12. The dynamic model with 2D and 3D structure is currently the most accurate representation of the dynamic microenvironment of BBB in vitro; however, it is important to note that the development of this model involves extensive prior design and validation effort. Selecting the proper BBB model in accordance with the real needs of the research can obtain more accurate experimental results.
The evaluation methods of the functional integrity of BBB in vitro model usually include a permeability test and transmembrane resistance value test. The former is mainly accomplished by assessing the permeability of fluorescein-labeled macromolecular substances. The method is straightforward and precise, but the structure of the cell layer changes after the fluorescent substance passes through, resulting in low sample utilization37. This deficiency is effectively made up for by the development of the TEER detection method. The two electrodes were placed on both sides of the cell layer, and the integrity of the barrier function was assessed by measuring the ion current resistance across the cell barrier38. The total resistance was subtracted from the environmental resistance, such as culture membrane resistance and medium resistance, and multiplied by the area of the culture membrane to obtain the final BBB resistance (TEER, Ωcm2)39. A higher value of TEER values represents a higher degree of tight junctions between cells. TEER measuring the operation is simple and noninvasive, cell barrier function once formed resistance would be in a stable range. This feature enables the operator to maintain similar TEER values even when using different instruments under standard operating conditions. Only the temperature and the placement of the electrode insertion require extra attention from the operator. The increase of temperature and the electrode touching the bottom will decrease cell resistance.
In this study, a straightforward BBB monolayer cell model in vitro was successfully constructed by evaluating the temporal resistance of bEnd.3 cells in the upper chamber of the plate. The hypoxic environment induced by CoCl2disrupted the tight junction between endothelial cells, which significantly reduced TEER in comparison to normal cells. According to this experiment protocol described in the standard process to create an in vitro BBB model has a high success rate and repeatability. Only the seeding density needs to be altered if this experiment is run with different well plate specifications and the liquid levels in the upper and lower chambers of the plates are flush. However, The TEER value will be somewhat impacted by the electrode's incorrect location and the electric field's heterogeneity throughout the cell layer12. In most cases, TEER will be confirmed simultaneously by immunofluorescence and permeability detection depending on the study requirements of various BBB models. This cell model will be improved in the future in order to screen out medications that may sustain the BBB damage brought on by hypoxia. In conclusion, the use of TEER detection technology will likely have a significant impact on the creation of medications and therapy strategies for neurological illnesses.
Divulgaciones
The authors have nothing to disclose.
Acknowledgements
We appreciate the financial support from the National Natural Science Foundation of China (82274207 and 82104533), the Key Research and Development Program of Ningxia (2023BEG02012), and Xinglin Scholar Research Promotion Project of Chengdu University of TCM (XKTD2022013).
Materials
| 24-well transwell plate | Corning (Corning 3470, 0.33 cm2, 0.4 µm) | 10522023 | |
| 75 % ethanol | ChengDu Chron Chemicals Co,.Ltd | 2023052901 | |
| 96-well plate | Guangzhou Jet Bio-Filtration Co., Ltd | 220412-078-B | |
| bEnd.3 cells | Hunan Fenghui Biotechnology Co., Ltd | CL0049 | |
| Cell counting kit-8 (CCK-8) | Boster Biological Technology Co., Ltd | BG0025 | |
| Cell culture dish (100mm) | Zhejiang Sorfa Life Science Research Co., Ltd | 1192022 | |
| Cobalt Chloride (CoCl2) | Sigma | 15862 | |
| DMSO | Boster Biological Technology Co., Ltd | PYG0040 | |
| Dulbecco's modified eagle medium (1x) | Gibco ThermoFisher Scientific | 8121587 | |
| Fetal bovine serum | Gibco ThermoFisher Scientific | 2166090RP | |
| GraphPad Prism software | GraphPad Software | 9.0.0(121) | |
| Matrigel (Contains collagen IV) | MedChemexpress | HY-K6002 | |
| Microplate reader | Molecular Devices | SpectraMax iD5 | |
| OriginPro 8 software | OriginLab Corporation | v8.0724(B724) | |
| Penicillin-Streptomycin (100x) | Boster Biological Technology Co., Ltd | 17C18B16 | |
| Phosphate buffered saline (PBS, 1x) | Gibco ThermoFisher Scientific | 8120485 | |
| Sodium hypochlorite | ChengDu Chron Chemicals Co,.Ltd | 2022091501 | |
| Transmembrane resistance meter | World Precision Instruments LLC | VOM3 (verison 1.6) | |
| Trypsin 0.25% (1x) | HyClone | J210045 |
Referencias
- Kim, Y., et al. CLEC14A deficiency exacerbates neuronal loss by increasing blood-brain barrier permeability and inflammation. J Neuroinflammation. 17 (1), 48 (2020).
- Bagchi, S., et al. In-vitro blood-brain barrier models for drug screening and permeation studies: an overview. Drug Des Devel Ther. 13, 3591-3605 (2019).
- Daneman, R., Prat, A. The blood-brain barrier. Cold Spring Harb perspect Biol. 7 (1), 020412 (2015).
- Profaci, C. P., Munji, R. N., Pulido, R. S., Daneman, R. The blood-brain barrier in health and disease: Important unanswered questions. J Exp Med. 217 (4), 20190062 (2020).
- Pardridge, W. M. Blood-brain barrier delivery. Drug Discov Today. 12 (1-2), 54-56 (2007).
- Eigenmann, D. E., et al. Comparative study of four immortalized human brain capillary endothelial cell lines, hCMEC/D3, hBMEC, TY10, and BB19, and optimization of culture conditions, for an in vitro blood-brain barrier model for drug permeability studies. Fluids Barriers CNS. 10 (1), 33 (2013).
- Gajdács, M. The concept of an ideal antibiotic: Implications for drug design. Molecule. 24 (5), 892 (2019).
- Stanimirovic, D. B., Bani-Yaghoub, M., Perkins, M., Haqqani, A. S. Blood-brain barrier models: in vitro to in vivo translation in preclinical development of CNS-targeting biotherapeutics. Expert Opin Drug Discov. 10 (2), 141-155 (2015).
- Helms, H. C., et al. In vitro models of the blood-brain barrier: An overview of commonly used brain endothelial cell culture models and guidelines for their use. J Cereb Blood Flow Metab. 36 (5), 862-890 (2016).
- Özyurt, M. G., Bayir, E., DoĞan, &. #. 3. 5. 0. ;., ÖztÜrk, &. #. 3. 5. 0. ;., Şendemİr, A. Coculture model of blood-brain barrier on electrospun nanofibers. Turk J Biol. 44 (4), 121-132 (2020).
- Kim, W., et al. Functional validation of the simplified in vitro 3D Co-culture based BBB model. Biochem Biophys Res Commun. 625, 128-133 (2022).
- Aazmi, A., et al. Vascularizing the brain in vitro. iScience. 25 (4), 104110 (2022).
- Burkhart, A., et al. Transfection of brain capillary endothelial cells in primary culture with defined blood-brain barrier properties. Fluids Barriers CNS. 12, 19 (2015).
- Campisi, M., et al. 3D self-organized microvascular model of the human blood-brain barrier with endothelial cells, pericytes and astrocytes. Biomaterials. 180, 117-129 (2018).
- Peng, Y., et al. Neuroinflammatory in vitro cell culture models and the potential applications for neurological disorders. Front Pharmacol. 12, 671734 (2021).
- Secker, P. F., Schlichenmaier, N., Beilmann, M., Deschl, U., Dietrich, D. R. Functional transepithelial transport measurements to detect nephrotoxicity in vitro using the RPTEC/TERT1 cell line. Arch Toxicol. 93 (7), 1965-1978 (2019).
- Nazari, H., et al. Advances in TEER measurements of biological barriers in microphysiological systems. Biosens Bioelectron. 234, 115355 (2023).
- Nicolas, A., et al. High throughput transepithelial electrical resistance (TEER) measurements on perfused membrane-free epithelia. Lab Chip. 21 (9), 1676-1685 (2021).
- Yang, Z., et al. Autophagy alleviates hypoxia-induced blood-brain barrier injury via regulation of CLDN5 (claudin 5). Autophagy. 17 (10), 3048-3067 (2021).
- Feng, S., et al. RhoA/ROCK-2 pathway inhibition and tight junction protein upregulation by catalpol suppresses lipopolysaccaride-induced disruption of blood-brain barrier permeability. Molecules. 23 (9), (2018).
- Sulhan, S., Lyon, K. A., Shapiro, L. A., Huang, J. H. Neuroinflammation and blood-brain barrier disruption following traumatic brain injury: Pathophysiology and potential therapeutic targets. J Neurosci Res. 98 (1), 19-28 (2020).
- Liu, B., et al. Notoginsenoside R1 intervenes degradation and redistribution of tight junctions to ameliorate blood-brain barrier permeability by Caveolin-1/MMP2/9 pathway after acute ischemic stroke. Phytomedicine. 90, 153660 (2021).
- Hou, Y., et al. Salidroside intensifies mitochondrial function of CoCl2-damaged HT22 cells by stimulating PI3K-AKT-MAPK signaling pathway. Phytomedicine. 109, 154568 (2023).
- Muñoz-Sánchez, J., Chánez-Cárdenas, M. E. The use of cobalt chloride as a chemical hypoxia model. J Appl Toxicol. 39 (4), 556-570 (2019).
- Jiang, S., et al. Salidroside attenuates high altitude hypobaric hypoxia-induced brain injury in mice via inhibiting NF-κB/NLRP3 pathway. Eur J Pharmacol. 925, 175015 (2022).
- Xie, N., et al. Rhodiola crenulate alleviates hypobaric hypoxia-induced brain injury via adjusting NF-κB/NLRP3-mediated inflammation. Phytomedicine. 103, 154240 (2022).
- Thiebaut de Schotten, M., Forkel, S. J. The emergent properties of the connected brain. Science. 378 (6619), 505-510 (2022).
- Tu, W. J., et al. Estimated burden of stroke in China in 2020. JAMA Netw Open. 6 (3), 231455 (2023).
- Alzheimers Dement. Alzheimer’s disease facts and figures. Alzheimers Dement. 17 (3), 327-406 (2021).
- Wang, R., et al. Neutrophil extracellular traps promote tPA-induced brain hemorrhage via cGAS in mice with stroke. Blood. 138 (1), 91-103 (2021).
- Liu, X. X., et al. Endothelial Cdk5 deficit leads to the development of spontaneous epilepsy through CXCL1/CXCR2-mediated reactive astrogliosis. J Exp Med. 217 (1), 20180992 (2020).
- Chen, X., et al. Modeling Sporadic Alzheimer’s Disease in Human Brain Organoids under Serum Exposure. Adv Sci (Weinh). 8 (18), 2101462 (2021).
- Qi, D., Lin, H., Hu, B., Wei, Y. A review on in vitro model of the blood-brain barrier (BBB) based on hCMEC/D3 cells. J Control Release. 358, 78-97 (2023).
- Artus, C., et al. The Wnt/planar cell polarity signaling pathway contributes to the integrity of tight junctions in brain endothelial cells. J Cereb Blood Flow Metab. 34 (3), 433-440 (2014).
- Sivandzade, F., Cucullo, L. In-vitro blood-brain barrier modeling: A review of modern and fast-advancing technologies. J Cereb Blood Flow Metab. 38 (10), 1667-1681 (2018).
- Galla, H. J. Monocultures of primary porcine brain capillary endothelial cells: Still a functional in vitro model for the blood-brain-barrier. J Control Release. 285, 172-177 (2018).
- Srinivasan, B., Kolli, A. R. Transepithelial/transendothelial electrical resistance (TEER) to measure the integrity of blood-brain barrier. Blood-Brain Barrier. 142, 99-114 (2019).
- Liang, Y., Yoon, J. Y. In situ sensors for blood-brain barrier (BBB) on a chip. Sens Actuators Rep. 3, 100031 (2021).
- Ozgür, B., Helms, H. C. C., Tornabene, E., Brodin, B. Hypoxia increases expression of selected blood-brain barrier transporters GLUT-1, P-gp, SLC7A5 and TFRC, while maintaining barrier integrity, in brain capillary endothelial monolayers. Fluids Barriers CNS. 19 (1), (2022).

