Ex Vivo Infection of Human Lymphoid Tissue and Female Genital Mucosa with Human Immunodeficiency Virus 1 and Histoculture
Summary
Infection of human tissues with human immunodeficiency virus (HIV) ex vivo provides a valuable 3D model of virus pathogenesis. Here, we describe a protocol to process and infect tissue specimens from human tonsils and female genital mucosae with HIV-1 and maintain them in culture at the liquid-air interface.
Abstract
Histocultures allow studying intercellular interactions within human tissues, and they can be employed to model host-pathogen interactions under controlled laboratory conditions. Ex vivo infection of human tissues with human immunodeficiency virus (HIV), among other viruses, has been successfully used to investigate early disease pathogenesis, as well as a platform to test the efficacy and toxicity of antiviral drugs. In the present protocol, we explain how to process and infect with HIV-1 tissue explants from human tonsils and cervical mucosae, and maintain them in culture on top of gelatin sponges at the liquid-air interface for about two weeks. This non-polarized culture setting maximizes access to nutrients in culture medium and oxygen, although progressive loss of tissue integrity and functional architectures remains its main limitation. This method allows monitoring HIV-1 replication and pathogenesis using several techniques, including immunoassays, qPCR, and flow cytometry. Of importance, the physiologic variability between tissue donors, as well as between explants from different areas of the same specimen, may significantly affect experimental results. To ensure result reproducibility, it is critical to use an adequate number of explants, technical replicates, and donor-matched control conditions to normalize the results of the experimental treatments when compiling data from multiple experiments (i.e., conducted using tissue from different donors) for statistical analysis.
Introduction
Monotypic bi-dimensional cell cultures, here referred to as conventional, do not account for the spatial and functional communication between the large variety of cell types that compose tissues and organs. This aspect is of paramount importance for experimental models of disease, as interference with homeostatic intercellular interactions is the driving factor of all pathologies. Tissue explants offer major advantages for modeling health and disease in humans because they retain the cytoarchitecture and many important functional aspects of organs as they are in vivo, although for a limited amount of time1. For example, upon ex vivo challenge with recall antigens, such as diphtheria toxoid or tetanus toxoid, tonsillar tissue responds with a vigorous production of antigen-specific antibodies2. Like any other ex vivo model, histoculture has its own limitations: inter-donor variability, tissue polarization, limited tissue survival, and difficulty in monitoring cells beyond the depth of confocal microscopy1. Nevertheless, human tissue explants remain a model of choice to study homeostatic and pathogenic immunological processes in humans, including host-pathogen interactions and potential therapeutic interventions3.
The critical events of HIV-1 pathogenesis take place in tissues. Infection of the genital mucosa accounts for the majority of all HIV-1 transmission events worldwide4. Lymphoid tissue is the major site of virus replication during acute infection and harbors a significant pool of latently-infected cells5, and their persistence represents the main obstacle to achieve a cure6. The culture and ex vivo challenge of human lymphoid and mucosal tissues provide some advantages over conventional systems based on isolated cells for the study of HIV-1. For instance, tissue-resident cells can support HIV-1 infection in the absence of exogenous activation, as opposed to peripheral blood mononuclear cells1. The use of lymphoid tissue explants has allowed a better understanding of some key mechanisms underlying CD4 T cell depletion, i.e., the bystander effect7, which is the hallmark of acute infection. The preservation of structures like B cell follicles in lymphoid tissue8 and the epithelium in female genital mucosa explants9 offers the unique opportunity to integrate spatial and functional features of HIV-1 infection at these sites. Finally, histocultures were successfully used to model and study HIV-1 and herpesvirus co-infection10,11, as well as for preclinical testing of antiretrovirals and multitarget microbicides12,13,14,15.
Here, we describe a detailed protocol for the culture of human tissue explants obtained from tonsils and mucosal tissue from the lower female genital tract (cervix), covering tissue dissection to explant challenge with HIV-1 in a non-polarized way. The culture of tissue explants at the liquid-air interface, using gelatin sponges as a support, maximizes exposure to air oxygen while providing access to culture medium nutrients through the sponge capillaries, thus delaying their natural decay. The most immediate way of evaluating HIV-1 replication in our system is to measure the amount of virus released in the explant culture medium over time by immunoassay or qPCR. HIV-1 infection and pathogenesis (e.g., CD4 T cell depletion) can also be evaluated in tissue explants by bulk RNA/DNA extraction and qPCR, in situ staining, or single cell-analysis upon tissue digestion by flow cytometry.
Protocol
The protocol for collection of human tissues may require ethical approval by the local competent authorities. In case of indicated surgeries such as tonsillectomy and hysterectomy, the specimens are not collected specifically for research purpose and the study is not considered human subjects research (National Institutes of Health. Research on Human Subjects. https://humansubjects.nih.gov/walkthrough-investigator#tabpanel11). However, obtaining tissue donors' personal and medical data (e.g., sex, age, current drug use, history of infections, etc.) that may help interpret experimental results, poses concerns about informed consent and privacy that must be addressed in the protocol for tissue collection.
Caution: The entire procedure should be carried out in a biological safety cabinet. All human specimens, including those from 'healthy' individuals, may harbor infectious agents. The operator should receive training to work with blood-borne pathogens to safely handle tissue specimens, even if experiments do not involve the use of HIV. A risk assessment of the procedure of tissue dissection and infection with HIV should be carried out by trained staff to ensure the safety of the operator and coworkers. The use of infectious HIV requires dedicated biosafety level 2 or 3 environments depending on the country and institute-specific regulations on hazardous biologicals and blood-borne pathogens.
1. Preparation of Gelatin Sponges
NOTE: Although it is not strictly necessary to prepare gelatin sponges before tissue dissection, it is more convenient to follow the order outlined here, especially when handling a large amount of tissue and/or from many donors.
- Prepare culture medium (CM) and supplement it with antibiotic solution (Tircacillin-clavulanate mix) before use to make CMT (Table of Materials). Discard any leftover antibiotic solution.
NOTE: Ticarcillin and clavulanate in CMT are poorly stable. If needed, re-supplement CMT with antibiotic solution after about 24 h from preparation. It is not required to add antibiotic solution to explant medium every 24 h during culture. - Fill a 100 mm x 20 mm Petri dish with about 20–30 mL of CMT.
NOTE: This setting is optimal to prepare enough gelatin sponges for two 6-well plates or one 12-well plate at the time. If many plates are required, use a wider Petri dish and larger CMT volume to speed up the preparation. - Transfer the gelatin sponge(s) into the Petri dish using sterile forceps. Wet the sponges on both sides and allow the sponges to soak up medium for 1 min. Press the sponges against the bottom of the Petri dish for about 2 min using a sterile spatula.
NOTE: This step is of crucial importance because the presence of air bubbles in the sponge will block the capillaries through which culture medium nutrients reach the tissue. Gelatin sponges are extremely brittle when dehydrated. Gently push down on the sponge with the spatula, especially at the beginning, to avoid breaking the sponge. - Use sterile scissors to cut the rehydrated gelatin sponges into pieces of equal size of about 1 cm2. Transfer 1 sponge piece using forceps into each well of a culture plate. Add 3–4 mL of CMT into each well of a 6-well plate (tonsils) and 1 mL per well into a 12-well plate (cervix). Place the plates in the incubator, set at 37 °C, 5% CO2, ≥ 90% humidity, until the tissue explants are ready to be loaded on the sponges.
Note: The volume of CMT to add into the plate should be adjusted to the thickness of the sponge to keep the explants at the liquid-air interface.
2. Dissection of Human Tonsillar Tissue
NOTE: Tonsils should be processed as soon as possible after surgery, ideally the same day of surgery. Alternatively, specimens can be left overnight submerged in CMT at 4 °C.
- Allow the CM enough time to reach room temperature (RT) or put it in a water bath pre-warmed at 37 °C. Supplement the CM with antibiotic solution (CMT) before use. Discard any antibiotic solution left over. Pour 70% ethanol solution into a clean container to soak forceps and scalpel whenever needed during the dissection procedure. Clean the tools and change the scalpel blade between dissections of specimens from different donors.
- Transfer the tonsils from the transportation container into a 100 mm-Petri dish containing 10-20 mL of CMT using sterile forceps.
NOTE: Specimens with widespread areas of cauterized, bloody, or necrotic tissue should be discarded. - Use the lid of the Petri dish as a cutting surface to dissect tissue. Holding the tissue gently with forceps, cut each tonsil into several big pieces using sterile scalpel and blade.
Caution: Handling sharp tools to dissect human specimens increases the risk of injury and contamination. The operator should consider wearing metal, mesh, cut-resistant gloves as additional protection. - Remove cauterized, bloody, and fibroid tissue, and any parts containing tonsilloliths (calcified material) and/or with green-brownish color using forceps and scalpel.
NOTE: While working on one piece of tissue, it is important to keep the rest of the tissue submerged in medium to avoid tissue desiccation. - Cut each tissue piece into slices of about 2 mm in thickness. Remove any unwanted part as in the previous step. Cut the tissue slices into 2 mm-thick strips. Cut the tissue strips into 2 mm-thick blocks. This should result in tissue explants of roughly 8 mm3.
- Transfer the explants into a new 100 mm Petri dish containing 10–20 mL of CMT to avoid tissue desiccation while proceeding with the dissection. At the end of dissection, swirl the plate to randomize the explant distribution. Place 9 tissue explants on top of each gelatin sponge in a 6-well plate using forceps, allowing space between them. Return the plates to the incubator.
NOTE: Typically, explants are cultured overnight and inoculation of cultures with HIV-1 is performed the next day. This is to make sure that no bacterial or fungal contamination develops in the culture. In addition, cells tend to egress tonsillar tissue explants after dissection. This process is largely completed within the first 24 h of culture1. - Dispose of all biological waste in apposite containers according to the institute's regulations on handling hazardous biologicals and the specific risk assessment.
3. Infection of Tonsillar Tissue Explants with HIV-1
NOTE: To reduce result variability between independent experiments, the same virus preparation should be used for an entire study. Virus can be propagated in exogenously activated peripheral blood mononuclear cells and then the culture supernatant can be aliquoted for storage at -80 °C to avoid repeated freezing and thawing (Table of Materials).
- Put the CM in a water bath pre-warmed at 37 °C. Supplement the CM with antibiotic solution (CMT) before use. Discard any leftover antibiotic solution.
- Aspirate the medium in the 6-well plate(s) with a pipette and discard it in a container with disinfectant solution. Tilt the plate and gently push the gelatin sponges to the upper part of the well to allow the medium to gather at the bottom, and aspirate and discard it. Add 3-4 mL of CMT to each well.
- Thaw the HIV-1 virus preparation in the water bath at 37 °C. If necessary, dilute the virus stock with CM (Table 1).
NOTE: The virus stock should be diluted so that the selected inoculum is contained in a volume of 5–8 µL (Table 1). For an efficient infection, it is critical to use the minimum time required between thawing the HIV-1 preparation and infecting tissue explants. - Pipette the virus inoculum directly on top of each of the 9 explants on a gelatin sponge. Return the plate(s) to the incubator as soon as the infection is completed. Discard any residual virus preparation. Continue to Section 5.
NOTE: To accurately deliver the virus inoculum the operator should consider using a reverse pipetting technique and changing the tip for every well. This involves pushing the pipette piston down to the purge position (the second stop) to draw the virus inoculum up, and pushing to the first stop to deliver the inoculum, which helps minimizing bubble formation and the error associated with repeated sampling of small volumes, i.e., 5–8 µL.
4. Dissection and Infection of Uterine Cervical Mucosa
NOTE: For optimal results, explants of cervical mucosae should be processed and infected as soon as possible after surgery, ideally the same day of surgery. Alternatively, specimens can be stored submerged in CMT at 4 °C overnight, and infected immediately after dissection.
- Allow the CM enough time to reach RT or put it in a water bath pre-warmed at 37 °C. Supplement the CM with antibiotic solution (CMT) before use. Discard any leftover antibiotic solution. Pour 70% ethanol solution into a clean container to soak the forceps and scalpel whenever needed during the dissection procedure. Clean the tools and change the scalpel blade between dissections of specimens from multiple donors.
- Using sterile forceps, transfer the sample from the transportation container into a 100 mm Petri dish containing 10–20 mL of CMT.
- Use the lid of the Petri dish as a cutting surface to dissect the tissue. Holding the tissue gently with forceps, separate the mucosa of the ectocervix and/or endocervix from the underneath stromal and muscular tissue (submucosa) with a scalpel and blade to obtain strips of mucosa.
NOTE: While working on one piece of tissue, it is important to keep the rest of the tissue submerged in medium to avoid tissue desiccation. - Cut the mucosa into 2 mm-wide strips, remove and discard as much submucosa as possible, leaving only a 2 mm-thick layer of tissue. Cut the strips into 2 mm-thick blocks. This should result in tissue explants of roughly 8 mm3.
Caution: Handling sharp tools to dissect human specimens increases the risk of injury and contamination. The operator should consider wearing metal, mesh, cut-resistant gloves as additional protection. - Transfer tissue explants into a new 100 mm Petri dish containing 10–20 mL of CMT to avoid tissue desiccation while proceeding with the dissection. At the end of dissection, swirl the plate to randomize the explant distribution.
- With sterile forceps, transfer the explants into sterile 1.5-mL conical tube(s) (maximum 16 explants per tube). Remove any medium in the tube using a pipette.
- Thaw the HIV-1 preparation in a water bath at 37 °C. If necessary, dilute the virus stock with CM. Transfer the virus into the tube(s) containing the explants. Discard any residual virus preparation.
NOTE: The virus stock should be diluted so that the selected inoculum is contained in a volume of minimum 0.5 mL (Table 1). To reduce result variability between independent experiments, the same virus preparation should be used for an entire study (Table of Materials). - Transfer the tubes into a thermo-shaker and incubate for 2 h at 37 °C rocking at 300 rpm. Gently invert the tubes a few times every 30–60 min.
Note: For an efficient infection, it is critical to use the minimum time required between thawing the HIV-1 preparation and transferring the tubes to 37 °C. - Fill a 6-well plate with 3–4 mL per well of sterile phosphate buffer saline (PBS). At the of the incubation with HIV-1, discard all virus preparation in the tube(s) into a container with disinfectant solution using a pipette. Transfer the explants into the 6-well plate containing PBS using forceps.
- Allow the explants to rest in PBS for 1 min at RT, and then wash them by gently pipetting up-and-down the PBS into the well 2-3 times. Discard the PBS into a container with disinfectant solution using a pipette. Add 3–4 mL of new PBS to each well. Repeat two more times for a total of three washes. Discard the PBS just before transferring the explants to the sponges to avoid tissue desiccation.
NOTE: Explants of cervical mucosa, and in particular endocervix, release great amounts of mucus during infection. It is critical to wash and remove as much mucus as possible because unspecific retention on explants and subsequent release of virus into culture supernatant can mask virus replication. - Using forceps, transfer 5-8 explants on top of each gelatin sponge in a 12-well plate.Return the plate to the incubator.
- Dispose of all biological waste in apposite containers according to the institute's regulations on handling hazardous biologicals and the specific risk assessment.
5. Histoculture
- Change the CM every 3 days starting from the time of infection until day 12–15 post-infection. The CM and/or explants can be sampled at regular intervals throughout the culture time to assess HIV-1 replication, among other parameters.
- Put the CM in a water bath pre-warmed at 37 °C.
NOTE: It is not required to supplement the CM with antibiotic solution at this stage. - Collect a sample of CM with a pipette and transfer it into sterile 1.5 or 2 mL screw cap tube(s) for storage at -80 °C.
NOTE: The CM from replicate wells are pooled at collection. - Harvest the tissue explants with sterile forceps, remove the excess medium on explants by placing them on a piece of paper (optional), and transfer explants into sterile 1.5 or 2 mL screw cap tube(s). Process or store the tissue samples as required by the experiment.
NOTE: For flow cytometry, explants are immediately digested with an enzymatic cocktail to obtain a single-cell suspension (for more details see references 1, 9, 16, and 17). For RNA extraction, explants are kept in a RNA stabilization solution at 4 °C overnight before storing them at -80 °C. For DNA extraction or in situ staining (cervix), explants can be snap-frozen in liquid nitrogen or dry ice/ethanol slurry and stored at -80 °C. Alternatively, tonsillar explants can be fixed by submersion in a solution of PBS and 4% paraformaldehyde for in situ staining. - Aspirate the residual CM in the well with a pipette and discard it into a container with disinfectant solution. Tilt the plate and gently push the gelatin sponges to the upper part of the well to allow the medium to gather at the bottom, and then aspirate and discard it.
- Add 3–4 mL of CM to each well. Using sterile forceps, return any tissue explants that dropped into the medium to the gelatin sponge. Return the plate to the incubator.
- At the end of culture, dispose of all biological waste in apposite containers according to the institute's regulations on handling hazardous biologicals and the specific risk assessment.
Representative Results
Several techniques can be used to assess HIV-1 replication in tissue explants. Our standard read-out is to measure the amount of HIV-1 p24gag released in CM over time with an immunoassay18.
Tissue explants from different donors, infected with the same inoculum of the same HIV-1 stock, may yield different amounts of virus (Table 1). This is due to several factors, such as the number and status of HIV-1 target cells and the presence of co-infecting pathogens in the tissue16,19. In Figure 1, we provide an example of productive and abortive HIV-1 infection of cervical mucosa explants as defined by the amount of p24gag released in CM compared to donor-matched explants treated with the antiretroviral drug lamivudine (3TC) that completely suppresses HIV-1 replication. Although this control appears superfluous for infection of tissue explants from the donor in A, it helps in discriminating abortive (B) from productive infection (C) in explants that yield low levels of HIV-1 replication.
The use of an antiretroviral drug as a control condition can be useful to study HIV-1 infection in tissues that harbor low numbers of target cells, like the cervical mucosa, and when using slow-replicating HIV-1 variants, such as some primary isolates. In addition, for tissues infected with such viruses, it is important to consider using more sensitive detection methods, for instance qPCR.
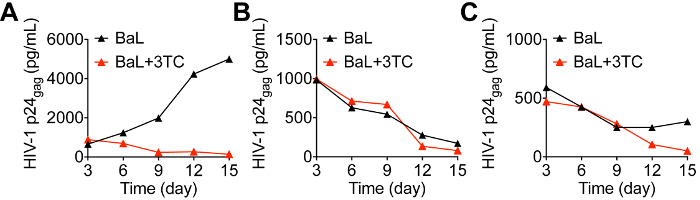
Figure 1: HIV-1 replication in cervical mucosa explants from three different tissue donors. Cervical tissue explants were infected with the same inoculum of HIV-1BaL by submersion in virus stock and cultured for 15 days in the presence or absence of the antiretroviral drug lamivudine (3TC) at the concentration of 10 µM. Culture medium was sampled every 3 days and samples from replicate wells were pooled at collection for analysis of HIV-1 replication by HIV-1 p24gag immunoassay. Please click here to view a larger version of this figure.
| Tissue type | Virus | Inoculum per explant (pg of HIV-1 p24gag) | No. of explants | Culture medium volume (mL) | No. of wells (technical replicates) | HIV-1 p24gag production (ng/mL) |
| Tonsillar | HIV-1BaL | 350–500 | 9 | 3-4 | 2–3 | 1–10 |
| HIV-1LAI.04 | 9 | 3-4 | 2–3 | 1–100 | ||
| Cervical | HIV-1BaL | 1,500–2,000 | 8 | 1 | 2 | 1–5 |
| HIV-1LAI.04 | 8 | 1 | 2 | undetectable |
Table 1: Reference values of HIV-1 inoculum for infection of tissue explants and virus production. The value of HIV-1 inoculum per individual tissue explant refers to virus stocks at the concentration of 50–70 ng/mL: a volume of 7 µL of undiluted virus stock is used to infect each tonsillar explant on top of a gelatin sponge; a volume of 500 µL of undiluted virus stock is used to infect 16 cervical explants by submersion in a 1.5 mL tube. Cervical explants are extensively washed in PBS before transferring them onto gelatin sponges. The value of HIV-1 production by tissue explants refers to the cumulative amount of p24gag released by 8 explants in 1 mL (cervix), or 9 explants in 3-4 mL (tonsils) of culture medium (CM) sampled every 3 days over 12-15 days of culture. CM from replicate wells is pooled at collection for each time point before replacing it with fresh CM. The value of p24gag concentration measured at day 3 was excluded from analysis because it partially accounts for virus absorption on explants and subsequent release into CM, i.e., inoculum carry-over. Typically, the infection of cervical tissue with HIV-1LAI.04 does not lead to detectable HIV-1 replication in our experimental system16.
Discussion
The use of human tissue explants for the study of HIV-1 infection provides advantages over traditional bi-dimensional and monotypic experimental systems, such as primary cells or cell lines, due their superior ability to reproduce intercellular interactions and cellular functions (e.g., cytokine production) as they are in vivo. Nevertheless, tonsillar and cervical tissue differ in many aspects including the number, and phenotypic and functional characteristics of HIV target cells1,16. For the same reason, HIV-1 variants with different co-receptor tropism (e.g., CCR5-tropic HIV-1BaL vs. CXCR4-tropic HIV-1LAI.04) perform differently both in tonsils and cervix (Table 1). The distribution of HIV coreceptors on target cells at the immune inductive and effector sites only partially accounts for local susceptibility to infection: CD4 T cells carrying CXCR4 are more abundant than CCR5-expressing cells in tonsillar tissue, thus explaining higher replication levels of HIV-1LAI.04 than HIV-1BaL, but the receptors are equally represented in the cervical mucosa16. Nevertheless, we rarely detected productive virus replication in cervical tissue challenged with HIV-1LAI.04, which is in line with the preferential transmission of individual HIV-1 CCR5-tropic variants observed in vivo20. This suggests that the differentiation and activation status of HIV-1 target cells may ultimately determine their ability to support HIV-1 replication16.
Gelatin sponges are hemostatic devices obtained from purified porcine skin (collagen), which are designed to be completely absorbed by the human body after a few weeks. We recommend using products that show slow degradation rate in culture as they better suit the purpose of maintaining tissue explants at the liquid-air interface for 2-3 weeks. We also recommend testing different batches of the same product to assess consistent performance in explant culture.
Similarly, the type and lot of fetal bovine serum (FBS) can affect HIV-1 replication levels. We advise testing several lots of FBS for CM optimization and use the same lot of FBS for an entire study. We routinely test FBS on tissue explants from 10 donors and select the lot that gives the highest HIV-1 replication.
For most of the experiments, we pool explants from endocervix and ectocervix to maximize the number of experimental conditions. One may consider keeping them separated because of their different structural and immunologic features21. Also, endocervical explants release and continue to produce a great amount of mucus in culture that might interfere with downstream analysis. Seeing as the area covered by endocervix is much smaller than ectocervix, it is challenging to conduct HIV infection experiments exclusively on the endocervical mucosa using an adequate number of explants and technical replicates.
Performing HIV-1 infection by submersion of cervical explants maximizes the chances of obtaining a productive infection due to the lower number of CD4 T cells present in the mucosa compared with lymphoid tissue. For the same reason, the cervical tissue is more sensitive to overnight storage and yields higher HIV-1 replication when infected shortly after surgery and immediately after dissection. Although infection by submersion in virus stock can be performed also for tonsillar tissue to ensure uniform exposure of explants to the virus, this approach entails higher tissue manipulation and cell loss than infection of explants on gelatin sponges as described in the protocol.
Polarized systems of HIV-1 challenge and culture of mucosal tissues exist and are currently used in other laboratories3,22,23,24,25. Although these systems are a valuable model of HIV-1 entry and penetration into the mucosa, their set up is generally more time-consuming and may require extensive tissue manipulation. Non-polarized models of mucosal transmission/pathogenesis still offer a valid platform to investigate the regulation of HIV-1 replication and the local pool of HIV-infected cells by endogenous and exogenous factors9,17,26, including drugs12,13,14,15.
Inter-donor variability can represent a major issue for result reproducibility between independent experiments conducted using specimens from multiple donors. Variability in cellular composition may also affect areas within the same specimen, i.e., intra-donor variability. To reduce variability and properly interpret results, it is critical to set up all conditions within one experiment using an adequate number of explants obtained from the same donor (donor-matched conditions). Results can be normalized to an internal control when compiling data from multiple experiments for statistical analysis. To reduce intra-donor variability, we recommend including at least 2 technical replicates for each experimental condition, for a total of 18 explants of tonsillar tissue (9/well), and 10-16 explants of cervical mucosa (5-8/well) (Table 1). The availability of medical records and the inclusion of additional analysis of patient material and/or experimental conditions, for instance to address the inflammatory status of a specimen, may significantly improve result interpretation (see reference 9 for an example).
Divulgations
The authors have nothing to disclose.
Acknowledgements
This work was supported by grants from the Foundation Blanceflor Boncompagni Ludovisi nee Bildt (http://blanceflor.se/), the Foundation Swedish Physicians against AIDS (http://www.aidsfond.se/, ref. FOa2014-0006), and Fondazione Andrea e Libi Lorini (http://fondazionelorini.it/) to Andrea Introini.
Materials
| Gelfoam 12-7 mm Absorbable gelatin sponge | Pfizer | NDC: 0009-0315-08 | Gelfoam and Spongostan perform equally well in histocuture for both tonsillar and cervical tissue. |
| SPONGOSTAN Standard 70 × 50 × 10 mm Absorbable haemostatic gelatin sponge | Ferrosan Medical Devices | MS0002 | Gelfoam and Spongostan perform equally well in histocuture for both tonsillar and cervical tissue. |
| RPMI 1640 with phenol red and glutamine | ThermoFisher Scientific | 21875034 | To RPMI1640 add MEM non-essential aminoacids, sodium pyruvate, gentamicin, amphotericin B and FBS 15% (v/v) to make culture medium (CM). |
| Modified Eagle's medium (MEM) non-essential aminoacids (100x) | ThermoFisher Scientific | 11140035 | To RPMI1640 add MEM non-essential aminoacids, sodium pyruvate, gentamicin, amphotericin B and FBS 15% (v/v) to make culture medium (CM). |
| Sodium pyruvate, 100 mM (100x) | ThermoFisher Scientific | 11360070 | To RPMI1640 add MEM non-essential aminoacids, sodium pyruvate, gentamicin, amphotericin B and FBS 15% (v/v) to make culture medium (CM). |
| Gentamicin 50 mg/mL (1000x) | ThermoFisher Scientific | 15750037 | To RPMI1640 add MEM non-essential aminoacids, sodium pyruvate, gentamicin, amphotericin B and FBS 15% (v/v) to make culture medium (CM). |
| Amphotericin B 250 μg/mL (100x) | ThermoFisher Scientific | 15290018 | To RPMI1640 add MEM non-essential aminoacids, sodium pyruvate, gentamicin, amphotericin B and FBS 15% (v/v) to make culture medium (CM). |
| Fetal bovine serum (FBS) | To RPMI1640 add MEM non-essential aminoacids, sodium pyruvate, gentamicin, amphotericin B and FBS 15% (v/v) to make culture medium (CM). | ||
| Ticarcillin disodium salt | Sigma-Aldrich | T5639-1G | Resuspend in sterile cell culture grade water tircacillin disodium (3g) and potassium clavulanate (100mg) and mix to obtain 100 mL of antibiotic solution (100x). Aliquote and store at -20 °C. Avoid repeated freezing and thawing. Supplement CM with antibiotic solution to make CMT. |
| Potassium clavulanate | Sigma-Aldrich | 33454-100MG | Resuspend in sterile cell culture grade water tircacillin disodium (3g) and potassium clavulanate (100mg) and mix to obtain 100 mL of antibiotic solution (100x). Aliquote and store at -20 °C. Avoid repeated freezing and thawing. Supplement CM with antibiotic solution to make CMT. |
| Sterile phosphate buffer saline (PBS) pH 7.4 w/o calcium, magnesium and phenol red | To use for storage and transportation of surgical specimens. PBS can be replaced with another isotonic solution with physiologic pH. Culture medium is best for overnight storage. | ||
| Sterile cell culture grade water | |||
| Sterile transportation container | |||
| 70% ethanol solution | |||
| Disinfectant solution for biological waste disposal | |||
| Sterile metal forceps or tweezers | |||
| Sterile metal scissors | |||
| Sterile flat weighing metal spatula | |||
| Sterile scalpels and blades | |||
| 6-well cell culture plates | |||
| 12-well cell culture plates | |||
| Sterile Petri dish, 100 mm × 20 mm | |||
| Cell-free HIV-1 viral preparation HIV-1BaL | NIH AIDS Reagent Program | 510 | The virus should be propagated to generate a stock large enough to perform several experiments. Aliquote virus suspension and store at -80 °C. Avoid repeated freezing and thawing. |
| Cell-free HIV-1 viral preparation HIV-1LAI.04 | NIH AIDS Reagent Program | 2522 | The virus should be propagated to generate a stock large enough to perform several experiments. Aliquote virus suspension and store at -80 °C. Avoid repeated freezing and thawing. |
| Lamivudine (3TC) | NIH AIDS Reagent Program | 8146 | Resuspend in DMSO at 10 mg/ml, aliquote and store at -20 °C. Avoid repeated freezing and thawing. |
| Biological safety cabinet | |||
| Water-jacketed CO2 incubator, set at 37 °C, 5% CO2, ≥ 90% humidity | |||
| Water bath set at 37 °C | |||
| Sterile 1.5- and 2-mL screw cap tubes | |||
| Dry bath shaker with heating block for 1.5-mL tubes, set at 37 °C, 300 rpm |
References
- Grivel, J. C., Margolis, L. Use of human tissue explants to study human infectious agents. Nature protoc. 4 (2), 256-269 (2009).
- Glushakova, S., Grivel, J. C., Fitzgerald, W., Sylwester, A., Zimmerberg, J., Margolis, L. B. Evidence for the HIV-1 phenotype switch as a causal factor in acquired immunodeficiency. Nat Med. 4 (2), 346-349 (1998).
- Dezzutti, C. S. Animal and human mucosal tissue models to study HIV biomedical interventions: can we predict success. J Int AIDS Soc. 18 (1), 20301 (2015).
- Lederman, M. M., Margolis, L. The lymph node in HIV pathogenesis. Semin Immunol. 20 (3), 187-195 (2008).
- Chun, T. W., Moir, S., Fauci, A. S. HIV reservoirs as obstacles and opportunities for an HIV cure. Nat Immunol. 16 (6), 584-589 (2015).
- Biancotto, A., et al. HIV-1 induced activation of CD4+ T cells creates new targets for HIV-1 infection in human lymphoid tissue ex vivo. Blood. 111 (2), 699-704 (2008).
- Van Laar, J. M., et al. Sustained secretion of immunoglobulin by long-lived human tonsil plasma cells. Am J Pathol. 171 (3), 917-927 (2007).
- Introini, A., et al. Seminal plasma induces inflammation and enhances HIV-1 replication in human cervical tissue explants. PLoS Pathog. 13 (5), 1006402 (2017).
- Grivel, J. C., et al. Suppression of CCR5- but not CXCR4-tropic HIV-1 in lymphoid tissue by human herpesvirus 6. Nat Med. 7 (11), 1232-1235 (2001).
- Rollenhagen, C., Lathrop, M. J., Macura, S. L., Doncel, G. F., Asin, S. N. Herpes simplex virus type-2 stimulates HIV-1 replication in cervical tissues: implications for HIV-1 transmission and efficacy of anti-HIV-1 microbicides. Mucosal Immunol. 7 (5), 1165-1174 (2014).
- Lisco, A., et al. Acyclovir is activated into a HIV-1 reverse transcriptase inhibitor in herpesvirus-infected human tissues. Cell Host Microbe. 4 (3), 260-270 (2008).
- Vanpouille, C., et al. A common anti-cytomegalovirus drug, ganciclovir, inhibits HIV-1 replication in human tissues ex vivo. AIDS. 31 (11), 1519-1528 (2017).
- Andrei, G., et al. Topical tenofovir, a microbicide effective against HIV, inhibits herpes simplex virus-2 replication. Cell Host Microbe. 10 (4), 379-389 (2011).
- Greenhead, P., Hayes, P., Watts, P. S., Laing, K. G., Griffin, G. E., Shattock, R. J. Parameters of human immunodeficiency virus infection of human cervical tissue and inhibition by vaginal virucides. J Virol. 74 (12), 5577-5586 (2012).
- Saba, E., et al. HIV-1 sexual transmission: early events of HIV-1 infection of human cervico-vaginal tissue in an optimized ex vivo model. Mucosal Immunol. 3 (3), 280-290 (2010).
- Introini, A., Vanpouille, C., Lisco, A., Grivel, J. C., Margolis, L. Interleukin-7 facilitates HIV-1 transmission to cervico-vaginal tissue ex vivo. PLoS Pathog. 9 (2), 1003148 (2013).
- Biancotto, A., et al. A highly sensitive and dynamic immunofluorescent cytometric bead assay for the detection of HIV-1 p24. J Virol Methods. 157 (1), 98-101 (2009).
- Lisco, A., Vanpouille, C., Margolis, L. War and peace between microbes: HIV-1 interactions with coinfecting viruses. Cell Host Microbe. 6 (5), 403-408 (2009).
- Keele, B. F., et al. Identification and characterization of transmitted and early founder virus envelopes in primary HIV-1 infection. Proc Natl Acad Sci U S A. 105 (21), 7552-7557 (2008).
- Pudney, J., Quayle, A. J., Anderson, D. J. Immunological microenvironments in the human vagina and cervix: mediators of cellular immunity are concentrated in the cervical transformation zone. Biol Reprod. 73 (6), 1253-1263 (2005).
- Ganor, Y., et al. Within 1h, HIV-1 uses viral synapses to enter efficiently the inner, but not outer, foreskin mucosa and engages Langerhans-T cell conjugates. Mucosal Immunol. 3 (5), 506-522 (2010).
- Cavarelli, M., Foglieni, C., Rescigno, M., Scarlatti, G. R5 HIV-1 envelope attracts dendritic cells to cross the human intestinal epithelium and sample luminal virions via engagement of the CCR5. EMBO Mol Med. 5 (5), 776-794 (2013).
- Cummins, J. E., et al. Preclinical testing of candidate topical microbicides for anti-human immunodeficiency virus type 1 activity and tissue toxicity in a human cervical explant culture. Antimicrob Agents Chemother. 51 (5), 1770-1779 (2007).
- Abner, S. R., et al. A human colorectal explant culture to evaluate topical microbicides for the prevention of HIV infection. J Infect Dis. 192 (9), 1545-1556 (2005).
- Saba, E., et al. Productive HIV-1 infection of human cervical tissue ex vivo is associated with the secretory phase of the menstrual cycle. Mucosal Immunol. 6 (6), 1081-1090 (2013).

