Isolation and Analysis of Brain-sequestered Leukocytes from Plasmodium berghei ANKA-infected Mice
Summary
A method for isolation of adherent inflammatory leukocytes from brain blood vessels of Plasmodium berghei ANKA-infected mice is described. The method allows quantification as well as phenotypic characterization of isolated leukocytes after staining with fluorescent antibodies and subsequent analysis by flow cytometry.
Abstract
We describe a method for isolation and characterization of adherent inflammatory cells from brain blood vessels of P. berghei ANKA-infected mice. Infection of susceptible mouse-strains with this parasite strain results in the induction of experimental cerebral malaria, a neurologic syndrome that recapitulates certain important aspects of Plasmodium falciparum-mediated severe malaria in humans 1,2 . Mature forms of blood-stage malaria express parasitic proteins on the surface of the infected erythrocyte, which allows them to bind to vascular endothelial cells. This process induces obstructions in blood flow, resulting in hypoxia and haemorrhages 3 and also stimulates the recruitment of inflammatory leukocytes to the site of parasite sequestration.
Unlike other infections, i.e neutrotopic viruses4-6, both malaria-parasitized red blood cells (pRBC) as well as associated inflammatory leukocytes remain sequestered within blood vessels rather than infiltrating the brain parenchyma. Thus to avoid contamination of sequestered leukocytes with non-inflammatory circulating cells, extensive intracardial perfusion of infected-mice prior to organ extraction and tissue processing is required in this procedure to remove the blood compartment. After perfusion, brains are harvested and dissected in small pieces. The tissue structure is further disrupted by enzymatic treatment with Collagenase D and DNAse I. The resulting brain homogenate is then centrifuged on a Percoll gradient that allows separation of brain-sequestered leukocytes (BSL) from myelin and other tissue debris. Isolated cells are then washed, counted using a hemocytometer and stained with fluorescent antibodies for subsequent analysis by flow cytometry.
This procedure allows comprehensive phenotypic characterization of inflammatory leukocytes migrating to the brain in response to various stimuli, including stroke as well as viral or parasitic infections. The method also provides a useful tool for assessment of novel anti-inflammatory treatments in pre-clinical animal models.
Protocol
1. Infection of Mice With P. berghei-ANKA
- Defrost an aliquot of cryopreserved P. berghei ANKA pRBC.
- Restrain a cerebral malaria-resistant BALB/c donor mouse (8-12 weeks-old) using the two-handed restraint technique. Inject mouse with 100-200 μl of pRBC using a 1 ml insulin syringe (28G needle). Routinely, 1-2 donor mice are injected.
- On days 4-5 post-infection (p.i) remove donor mouse from cage and place it on a workstation or a disposable working pad.
- Gently restrain mouse by the end of the tail and using small scissors cut the tail tip (approximately 1 mm). Alternatively, a small tail puncture using a 25 G needle could be performed.
- Place a drop of blood from the mouse’s tail vein near the end of a frosted-end microscope slide.
- Place a second slide (spreader) on a 45° angle and back it into the drop of blood. Once the blood spreads along the edge, push the spreader-slide evenly across the microscope slide to make the blood smear. Allow the smear to air dry.
- Fix blood smears in 100% methanol for 30 sec and then stain slides in freshly prepared Giemsa for 10 min.
- Rinse blood smear with running water for 1 min, allow to air-dry and examine slide under the microscope (100x, oil immersion). Enumerate pRBC within 1,000 erythrocytes and calculate percent parasitemia. Donor mice should reach parasitemia levels between 2.5-5% before they can be bled for infection of experimental animals.
- Collect blood from the donor mouse by retro-orbital bleeding using a heparinized micro-hematocrit capillary tube. All experiments are performed in compliance with The Walter & Eliza Hall Institute Animal Ethics Committee requirements. Depending on local Animal Ethic Committee requirements other bleeding procedures might be used. Dissolve required amount of blood in RPMI medium at a final concentration of 1X106 pRBC/0.2 ml. Consider that a normal mouse hematocrit is ~6×109 red blood cells/1 ml.
- Infect experimental C57BL/6 mice (8-12 weeks old) by injecting intraperitoneally (i.p) 1×106 pRBC/0.2 ml.
- To monitor parasitemia levels of infected mice follow steps 1.3-1.8. Parasitemia should be determined every 2-3 days starting on day 2 or 3 p.i.
- Onset of severe malaria in C57BL/6 mice might manifest as hunched appearance, ruffed fur and low activity. Some mice may recover at this stage, but progression to loss of self-righting reflex indicates irreversible disease and animals must be euthanized.
2. Intracardial Perfusion of Mice and Brain Extraction
- Assemble a manual gravity perfusion system by securing a 500 ml reservoir to a column holder attached to the top of a 60 cm column stand. Connect plastic tubing to the bottom end of the reservoir and secure a tubing clamp to control buffer flow. Attach tubing to a 23 G needle. Fill up the reservoir with PBS (kept at 22 °C), open clamp and allow buffer to run through the tubing to remove all air bubbles.
- Euthanize P. berghei ANKA-infected mouse by CO2 inhalation. Confirm death by the absence of pedal, orbital and respiratory responses.
- Pin euthanized mouse by the hind and front paws dorsally on a styrofoam dissection board contained in a plastic tray. Depending on local Animal Ethic Committee requirements anesthesia could be administered prior commencement of intracardial pefusion.
- Wipe ventral side with 70% ethanol.
- Use large scissors and forceps to open skin along the midline to expose the thoracic cavity. Fold and pin skin to the sides.
- Hold the sternum with fine forceps and cut the diaphragm and along both sides of sternum severing the ribs. Take care not to damage any large blood vessels.
- Pin the rib cage by the sternum loosely next to the head.
- Hold ventricles with fine forceps and carefully incise right atrium with fine scissors.
- Insert 23G needle attached to gravity perfusion system into left ventricle towards the ascending aorta while PBS is running. Insert only 0.5 cm of the needle tip.
- Perfuse mouse for 5 min or until effluent is clear.
- Unpin mouse and lay it on its abdomen. Wipe head with 70% ethanol.
- Using large scissors, make a cut just above the cervical spinal cord area.
- Use fine scissors to make a median caudal-rostral cut starting at the base of the skull and peel skin away to expose the skull.
- Holding the head, place the blades of a small scissors into each orbital cavity and make a cut between the orbits.
- Make a longitudinal cut along the sagittal suture and carefully peel the skull on each brain hemisphere outward.
- Using a spatula, gently lift the brain and place it into a 10 ml centrifuge tube containing RPMI medium.
3. Isolation of Brain-sequestered Leukocytes (BSL)
- Working in a safety cabinet, place freshly harvested brain on top of a stainless steel cell strainer (40-60 mesh size) in a Petri dish containing 3-5 ml of RPMI tissue culture medium.
- Cut brain tissue into small pieces.
- Push small pieces of brain tissue through the cell strainer using a crystal plunger.
- Transfer brain homogenate to a 10 ml tube and centrifuge at 250 x g for 10 min at 4 °C.
- Dissolve pellet in 3 ml of RPMI medium, containing 0.05% Collagenase D and 2U/ml DNAse I.
- Rotate mixture for 30 min at room temperature. Remove cell debris by pushing the mixture through a 70 μm nylon cell strainer and/or by incubating on ice for 5 min.
- Lay brain homogenate onto a 7 ml 30% Percoll cushion and centrifuge at 400 x g (no brakes) for 20 min at room temperature.
- Resuspend pellet in 1 ml of red blood cell lysis buffer and incubate on ice for 5 min to lyse adherent pRBC, which could not be removed from the brain by intracardial perfusion.
- Add 9 ml of RPMI medium, wash cells and centrifuge at 250 x g for 10 min at 4 °C.
- Resuspend BSL-containing pellet in 50-100 μl of RPMI medium and transfer cells to an Eppendorf tube.
- Dilute a 5-10 μl aliquot of the cell sample 1:2 in Trypan blue for identification of viable cells.
- Count viable cells under the microscope using a hemocytometer. From day 6 p.i onwards, when P. berghei ANKA-infected mice display neurological signs, 20,000-100,000 BSLs can be recovered.
4. Immunophenotyping of BSL by Multicolour Flow Cytometry
- Centrifuge cells at 250 x g for 10 min at 4 °C, aspirate the supernatant and resuspend pellet in 50 μl of staining buffer (PBS, 1% foetal calf serum (FCS), 2 mm EDTA).
- Add the 1 μl of purified anti-CD16/32 antibody (Fcblock).
- Incubate cells for 10 min on ice.
- Wash cells with 1 ml of Staining Buffer. Centrifuge cells at 250 x g for 10 min at 4 °C and aspirate the supernatant.
- Resuspend cells in 50 μl of Staining Buffer containing pre-determined optimal dilutions of required fluorescent antibodies, i.e. anti-CD4, anti-CD8, anti-TCR and anti-NK1.1.
- Incubate for 1 hr on ice.
- Wash cells with 1 ml of Staining Buffer. Centrifuge cells at 250 x g for 10 min at 4 °C and aspirate the supernatant.
- Resuspend cells in 100 μl of PBS.
- Transfer cells to a flow cytometry plastic tube.
- Using a flow cytometer, acquire at least 5,000-10,000 events. Appropriate unstained cell controls and fluorochrome compensation samples should be included as required.
- Analyze results using appropriate flow cytometry software.
Representative Results
The results in Fig. 2 show percentages and absolute numbers of different BSL populations recovered from brains of perfused or unperfused malaria-infected and naïve control mice. Isolated BSL were stained with PE-anti-NK1.1 and APC-anti-TCR-β antibodies as indicated in the Protocol text. Consistent with previous findings 7-9, αβTCR+ T cells comprised a high proportion of the BSL pool in brains of perfused malaria-infected mice (day 6 p.i). This population appeared to be significantly underrepresented in brains of non-perfused animals (Fig. 2A-B). The apparent reduction of T cell frequencies in non-perfused brains was associated with a considerably higher percentage and total number of double negative cells (αβTCR– NK1.1–) in these animals (Fig. 2A-B). High percentage and numbers on double negative cells in unperfused brains were not only detected in malaria-infected mice but also in naïve controls, suggesting that these cells are non-inflammatory leukocytes present in brain blood vessels that are recovered together with inflammatory cells if intracardial perfusion is not performed.
Two further examples of BSL analysis are shown in Fig. 3 and Fig. 4. Briefly, C57BL/6 mice were infected with P. berghei ANKA (1×106 pRBC). Temporal associations between leukocyte recruitment to the brain and the onset of neurological symptoms (between days 6-8 p.i) have been demonstrated in P. berghei ANKA infected mice 7-9. In this particular example, malaria-infected mice were euthanized on day 6 p.i, and the BSL were purified as described in the Protocol text. Isolated BSL were stained with PE-anti-NK1.1, APC-anti-TCR-β, FITC-anti-CD4 and PerCPCy5.5-anti-CD8α antibodies. The samples were acquired using a BD Biosciences FACSCalibur flow cytometer and the analysis performed using Weasel 3.0.1 software. Viable cells were gated by forward and side scatter. The percentages of NK cells, T lymphocytes and NKT cells (NK1.1+TCR+ cells) sequestered in brain of naïve and malaria-infected mice (day 6 p.i) are indicated in the top panels (Fig. 3A). The bottom panels show percentages of CD4+ and CD8+ T lymphocytes amongst gated NK1.1–αβTCR+ cells (Fig. 3A). Fig. 3B depicts an example in which absolute numbers of CD4+ and CD8+ brain-sequestered T cells were calculated on day 6 p.i with P. berghei ANKA. In general, 20,000-100,000 BSL can be recovered from brains of P. berghei ANKA infected mice. Several factors such as time p.i, susceptibility of the mouse strain or inclusion of anti-inflammatory treatments might influence cell recovery. Routinely, one individual brain provides enough cells for 1 set of antibody stainings.
In the example provided in Fig. 4 the chemokine receptor usage of brain-sequestered T lymphocytes was analyzed. Mice were infected with P. berghei ANKA and BSL were isolated on day 6 p.i. Cells were stained with APC-anti-TCR-β, PE-anti-CXCR3 and biotinylated-anti-CCR5 antibodies, followed by incubation with a streptavidin-PerCPCy5.5 conjugate. Samples were acquired and analyzed as per Fig. 3. The histograms represent percentages of αβTCR+ cells amongst total BSL in malaria-infected and naïve control mice. The contour plots in the middle and bottom panels show the percentages of CXCR3+ and CCR5+ cells within gated αβTCR+ cells.
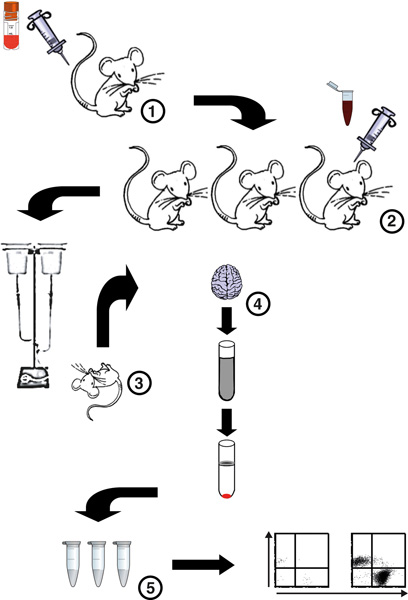
Figure 1. Flow chart of the procedure for isolation and analysis of BSL from P. berghei ANKA-infected mice. (1) A cryopreseved aliquot of P. berghei ANKA pRBC is defrosted and 1 or 2 donor mice are infected. (2) Four days later parsitemia levels of donor mice are calculated, donor mice are bled and blood dilutions prepared for infection of experimental mice. A malaria infection is then set up in severe malaria-susceptible C57BL/6 mice. (3) On days 5-7 p.i, mice are euthanized by CO2 inhalation and immediately intracardially perfused to remove all circulating non-adherent cells. (4) Brains are then harvested and a brain homogenate prepared by digestion of the tissue with Collagenase D and DNAse I. BSL are then separated from myelin and cell debris by a Percoll gradient. (5) Precipitated BSL are then washed, counted using a hemocytometer, stained with fluorescent antibodies and analyzed by flow cytometry.
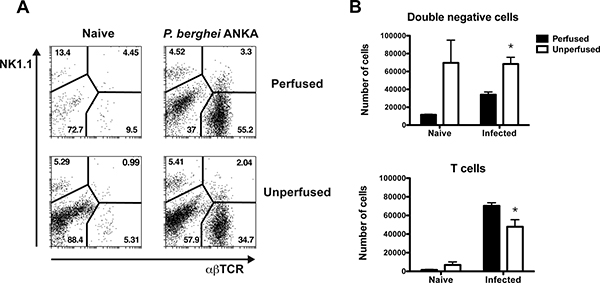
Figure 2. BSL analysis in brains of perfused or unperfused mice. C57BL/6 mice were infected with P. berghei ANKA (1×106 pRBC). Brains were harvested on day 6 p.i from perfused or unperfused animals. The BSL were isolated, stained with anti-NK1.1 and anti-TCR fluorescent antibodies and analyzed by flow cytometry. (A) Dot plots depict percentages of NK cells, T lymphocytes, NK1.1+TCR+ cells and double negative cells NK1.1–TCR– in perfused (top panels) or unperfused (bottom panels) malaria-infected and naïve control mice. (B) The absolute number of double negative cells and T lymphocytes and was calculated on day 6 p.i with P. berghei ANKA and naïve control mice. Each bar represents the mean of 3 samples ± SEM, *p>0.05.
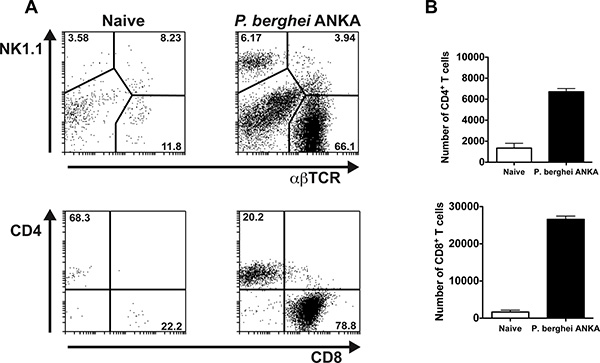
Figure 3. NK cells and T lymphocytes can be detected in brains of P. berghei ANKA infected mice. C57BL/6 mice were infected with P. berghei ANKA (1×106 pRBC). Brains were extracted on day 6 p.i after perfusion of the euthanized animals. The BSL were isolated, stained with anti-NK1.1, anti-TCR, anti-CD4 and anti-CD8 fluorescent antibodies and analyzed by flow cytometry. (A) Top panels depict percentages of NK cells, T lymphocytes and NK1.1+TCR+ cells in malaria-infected and naïve control mice. Bottom panels illustrate percentages of CD4+ and CD8+ T cells within gated αβTCR+ NK1.1– cells. Representative dot plots are shown. (B) The absolute number of brain-sequestered CD4+ and CD8+ T cells was calculated on day 6 p.i with P. berghei ANKA and naïve control mice. Each bar represents the mean of 3 samples ± SEM.
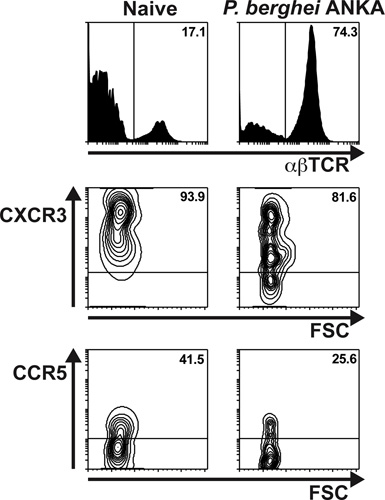
Figure 4. The majority of T lymphocytes migrating to the brain in response to severe malaria infection express the chemokine receptor CXCR3. C57BL/6 mice were infected with P. berghei ANKA (1×106 pRBC). Brains were extracted on day 6 p.i after extensive perfusion of the euthanized animals. The BSL were isolated, stained with anti-TCR, anti-CXCR3 and anti-CCR5 antibodies and analyzed by flow cytometry. Top panels depict percentages of αβT lymphocytes in malaria-infected and naïve control mice. The contour plots illustrate percentages of CXCR3+ (middle panels) and CCR5+ (bottom panel) cells within gated αβTCR+ lymphocytes.
| Problem | Troubleshooting |
| Incomplete perfusion |
|
| Not enough BSL recovered |
|
Table 1.
Discussion
The isolation and analysis of BSL is a method that allows characterization and quantification of inflammatory cells migrating to the brain in response to tissue injury or infection in experimental mouse models. The introduction of an intracardial perfusion step for removal of the blood compartment before organ extraction and subsequent cell isolation is useful to prevent contamination of inflammatory cells with non-inflammatory circulating leukocytes. This might not be an essential requirement in neurotropic infections such as murine encephalomyelitis virus in which inflammatory cells penetrate the brain parenchyma5, but is particularly relevant in rodent malaria, in which infected erythrocytes and inflammatory leukocytes remain sequestered within blood vessels rather than infiltrating brain tissue. Accordingly, intracardial perfusion of malaria-infected mice should not only be recommended for analysis of BSL but could be also useful for assessment of parasite-tissue sequestration 10,11 . Similar to non-inflammatory circulating leukocytes, immature forms of malaria parasites are unable to adhere to the vascular endothelium and should be removed by the perfusion procedure. In contrast, adherent pRBC (mature schizonts) appear to remain within brain blood vessels. P. berghei ANKA transgenic parasites expressing luciferase have been generated 12 and are a valuable resource for this type of analysis. After infection with luciferase-expressing lines, parasite tissue-sequestration can be determined by imaging of perfused brains from infected animals using an IVIS system 10,11 . A direct comparison of parasite-sequestration on days 6-7 p.i in brains of perfused animals and brains of mice infected with stage-specific reporter parasites (i.e expressing luciferase only during schizont stage) would be useful for further validation of this method.
One important drawback of traditional histological approaches for analysis of tissue-infiltrating cells is that these techniques do not allow assessment of cell populations that require recognition of more than one cell marker for their identification (i.e. NK1.1+αβTCR+ CD1d-restricted NKT or CD4+Foxp3+ T regulatory cells). Unlike histology, flow cytometric analysis of inflammatory leukocytes is amenable to multiple antibody stainings, providing a very useful tool for comprehensive phenotypic characterization of cellular infiltrates 7,9,13 . In addition, this method is sensitive enough to detect cell populations occurring at frequencies as low as 1-3% of the total intravascular infiltrate, including not only endogenous but also adoptively transferred cells as well as antigen specific T cells. P. berghei ANKA transgenic parasites expressing MHC I and MHC II-restricted epitopes from OVA 14 have been generated (PbTG). These parasites allow the analysis of parasite-specific immune responses by using transgenic T cells from OT-I and OT-II mice, which recognize the encoded MHC I and MHC II-restricted OVA epitopes, respectively. Using the method described here, adoptively transferred Ly5.1+CD8+ T cells from OT-I mice could be detected amongst BSL of Ly5.2+C57BL/6 PbTG-infected mice, providing evidence that inflammatory T cells migrating to the brain in response to malaria are parasite-specific 14.
The analysis of BSL is also useful to evaluate the potential of novel anti-inflammatory treatments in pre-clinical animal models. For example, the capacity of monoclonal antibodies against the CXCR3 chemokine IFN-γ-inducible protein 10 (IP-10) to prevent brain intravascular infiltration and alleviate disease symptoms associated with severe malaria has been successfully demonstrated using this method 11.
One limitation that this method might have is that the total number of cells recovered from one individual brain is generally enough for one set of antibody stainings. Thus separate experiments might be needed if more than 4-6 cell markers are required for the analysis. In general, the procedure is easy to perform. The only step that might require some initial training is the intracardial perfusion. A few hints that could be useful to overcome potential problems are listed in Table 1.
Divulgations
The authors have nothing to disclose.
Acknowledgements
The authors would like to thank Miss Liana Mackiewicz for technical assistance. This work was made possible through Victorian State Government Operational Infrastructure Support and Australian Government National Health and Medical Research Council IRIISS and Project Grant 1031212.
Materials
| Name of the reagent | Company | Catalogue number | Comments (optional) |
| Solutions and buffers | |||
| Giemsa’s azur eosin methylene blue solution | Merck Millipore | 1.09204.0500 | 1:10 dilution in distilled water |
| RPMI medium | Mouse tonicity | ||
| Mouse tonicity PBS | 20 mM Sodium Phosphate, 0.149 NaCl, pH 7.3 | ||
| 0.4%Trypan Blue | Sigma Aldrich | T-8154 | 1:2 dilution |
| Collagenase D | Worthington Biochemical | ||
| Deoxyribonuclease (DNAse) I | Sigma Aldrich | D4263-5VL | From bovine pancreas |
| Percoll | GE Healthcare | 17-0891-01 | 30% solution in PBS |
| Ultrapure Tris | Invitrogen | 15505-020 | |
| Ammonium Chloride (NH4Cl) | AnalaR | 10017 | |
| Red Cell Lysis Buffer | 17 mM Tris,14 nM NH4Cl, pH 7.2 | ||
| FCS | Gibco | 1009 | |
| EDTA disodium salt | Merck | 10093.5V | 0.1M, pH 7.2 |
| Antibodies and conjugates | |||
| Anti-mouse CD16/CD32 (Fc Block), clone 2.4G2 | BD Pharmingen | 553142 | 1 μl in 50 μl staining buffer (0.5 mg/50 ml) |
| FITC-anti-mouse CD4, clone H129.19 | BD Pharmingen | 553651 | |
| PE-anti-mouse NK1.1, clone PK136 | BD Pharmingen | 553165 | |
| PerCPCy5.5-anti-mouse CD8, clone 53-6-7 | BD Pharmingen | 551162 | |
| APC-anti-mouse TCR-β, clone H57-597 | BD Pharmingen | 553174 | |
| PE-anti-mouse CXCR3, clone 220803 | R&D Systems | FAB1685P | |
| Biotinylated-anti-mouse CCR5, clone C34-3448 | BD Pharmingen | 559922 | |
| Steptavidin-PerCP-Cy5.5 | BD Pharmingen | 551419 | |
| Equipment and material | |||
| SuperFrost microscope slide | Lomb Menzel-Gläser | ||
| Dissection forceps, scissors | REDA Instrumente | ||
| 500 ml PBS reservoir | Nalgene | ||
| Rubber tubing | |||
| 23G needle | BD PrecisionGlide | 302008 | |
| Cell dissociation kit containing metal sieve | Sigma Aldrich | CD-1 | |
| 70 μm nylon cell strainer | BD Falcon | 352350 | |
| Hemocytometer | GmbH Neubauer | 717810 | |
| Flow cytometry tubes | BD Falcon | 352008 |
References
- Brian de Souza, J., Riley, E. M. Cerebral malaria: the contribution of studies in animal models to our understanding of immunopathogenesis. Microbes and Infection. 4, 291-300 (2002).
- Schofield, L., Grau, G. E. Immunological processes in malaria pathogenesis. Nature. 5, 722-735 (2005).
- Miller, L. H., Baruch, D. I., Marsh, K., Doumbo, O. K. The pathogenic basis of malaria. Nature. 415, 673-679 (2002).
- Howe, C. L., Lafrance-Corey, R. G., Sundsbak, R. S., Lafrance, S. J. Inflammatory monocytes damage the hippocampus during acute picornavirus infection of the brain. Journal of neuroinflammation. 9, 50 (2012).
- LaFrance-Corey, R. G., Howe, C. L. Isolation of Brain-infiltrating Leukocytes. J. Vis. Exp. (52), e2747 (2011).
- Lim, S. M., Koraka, P., Osterhaus, A. D., Martina, B. E. West Nile virus: immunity and pathogenesis. Viruses. 3, 811-828 (2011).
- Belnoue, E., et al. On the pathogenic role of brain-sequestered alphabeta CD8+ T cells in experimental cerebral malaria. Journal of Immunology. 169, 6369-6375 (2002).
- Campanella, G. S., et al. Chemokine receptor CXCR3 and its ligands CXCL9 and CXCL10 are required for the development of murine cerebral malaria. Proceedings of the National Academy of Science U S A. 105, 4814-4819 (2008).
- Hansen, D. S., Bernard, N. J., Nie, C. Q., Schofield, L. NK cells stimulate recruitment of CXCR3+ T cells to the brain during Plasmodium berghei-mediated cerebral malaria. Journal of Immunology. 178, 5779-5788 (2007).
- Amante, F. H., et al. A role for natural regulatory T cells in the pathogenesis of experimental cerebral malaria. The American journal of pathology. 171, 548-559 (2007).
- Nie, C. Q., et al. IP-10-mediated T cell homing promotes cerebral inflammation over splenic immunity to malaria infection. PLoS pathogens. 5, e1000369 (2009).
- Franke-Fayard, B., et al. Murine malaria parasite sequestration: CD36 is the major receptor, but cerebral pathology is unlinked to sequestration. Proceedings of the National Academy of Science U S A. 102, 11468-11473 (2005).
- Nitcheu, J., et al. Perforin-dependent brain-infiltrating cytotoxic CD8+ T lymphocytes mediate experimental cerebral malaria pathogenesis. Journal of Immunololgy. 170, 2221-2228 (2003).
- Lundie, R. J., et al. Blood-stage Plasmodium infection induces CD8+ T lymphocytes to parasite-expressed antigens, largely regulated by CD8alpha+ dendritic cells. Proceeding of the National Academy of Science U S A. 105, 14509-14514 (2008).

