In Vitro Cellular Activity Evaluation of the Nanoemulsion Vaccine Adjuvant Ophiopogonin D
Summary
The protocol presents detailed methods for evaluating whether the nanoemulsion ophiopogonin D adjuvant promotes effective cellular immune responses.
Abstract
As a principal ingredient of vaccines, adjuvants can directly induce or enhance the powerful, widespread, innate, and adaptive immune responses associated with antigens. Ophiopogonin D (OP-D), a purified component extracted from the plant Ophiopogon japonicus, has been found to be useful as a vaccine adjuvant. The problems of the low solubility and toxicity of OP-D can be effectively overcome by using a low-energy emulsification method to prepare nanoemulsion ophiopogonin D (NOD). In this article, a series of in vitro protocols for cellular activity evaluation are examined. The cytotoxic effects of L929 were determined using a cell counting kit-8 assay. Then, the secreted cytokine levels and corresponding immune cell numbers after the stimulation and culture of splenocytes from immunized mice were detected by ELISA and ELISpot methods. In addition, the antigen uptake ability in bone marrow-derived dendritic cells (BMDCs), which were isolated from C57BL/6 mice and matured after incubation with GM-CSF plus IL-4, was observed by laser scanning confocal microscopy (CLSM). Importantly, macrophage activation was confirmed by measuring the levels of IL-1β, IL-6, and tumor necrosis factor alpha (TNF-α) cytokines by ELISA kits after coculturing peritoneal macrophages (PMs) from blank mice with the adjuvant for 24 h. It is hoped that this protocol will provide other researchers with direct and effective experimental approaches to evaluate the cellular response efficacies of novel vaccine adjuvants.
Introduction
Vaccines are an important means of preventing and treating infectious and noncommunicable diseases. The appropriate addition of adjuvants and delivery vehicles to vaccine formulations is beneficial for enhancing the immunogenicity of antigens and generating long-lasting immune responses1. In addition to the classical adjuvant alum (aluminum salt), there are six kinds of adjuvants for vaccines that are currently marketed: MF592,3, AS043, AS033, AS013, CpG10184, and Matrix-M5. Generally, when the human body encounters a viral attack, the first and second lines of defense (skin, mucosa, and macrophages) take the lead in clearing the virus, and finally, the third line of defense, involving the immune organs and immune cells, is activated. Aluminum and aluminum salts have been the most widely used adjuvants for human vaccines since the early 1920s, eliciting an effective innate immune response6. However, it has been proposed that the activation of antigen-presenting cells (APCs) by classical adjuvants, which stimulates the immune cells to generate specific sets of cytokines and chemokines, is the mechanism by which adjuvants work and may be one of the reasons why adjuvants exert only transient effects on specific immune responses7. The presence of limited licensed adjuvants for human use is a restrictive factor for developing vaccines that elicit effective immune responses8.
Currently, an increasing number of adjuvant studies are demonstrating the ability to induce a strong cellular immune response in mice. QS-21 has been shown to induce a balanced T-helper 1 (Th1) and T-helper 2 (Th2) immune response, produce higher levels of antibody titers, and prolong the protection as an adjuvant, but its strong toxicity and hemolytic properties limit its development as a standalone clinical adjuvant9,10. OP-D (ruscogenin-O-α-L-rhamnopyranosy1-(1→2)-β-D-xylopyranosyl-(1→3)-β-D-fucopyranoside) is one of the steroidal saponins isolated from the root of the Chinese medicinal plant Ophiopogon japonicas4. Additionally, it is the chief pharmacologically active component (Shen Mai San) found in Radix Ophiopogonis and is known to have certain pharmacological properties11. Moreover, it is a member of the Liliaceae family and is widely utilized for its inhibitory and protective effects in cellular inflammation and myocardial injury. For example, OP-D ameliorates DNCB-induced atopic dermatitis-like lesions and tumor necrosis factor alpha (TNF-α) inflammatory HaCaT cells in BALB/c mice12. Importantly, OP-D promotes the antioxidative protection of the cardiovascular system and protects the heart against doxorubicin-induced autophagic injury by reducing both reactive oxygen species generation and disrupting mitochondrial membrane damage. Experiments have shown that taking OP-D with mono-desmoside helps to boost immune health, increase white blood cell counts and DNA synthesis, and make antibodies last longer13. It has previously been found that OP-D has an adjuvant effect14.
Nanoemulsions are oil-in-water nanoformulations composed of a combination of surfactants, oil, cosurfactants, and water12,15. These nanovaccine designs allow antigens and adjuvants to be encapsulated together to enhance immune stimulation, protect the antigens, and promote dendritic cell (DC) maturation16. For development of these novel adjuvants obtained from screening, it is important to find appropriate methods to evaluate their cellular response abilities.
The purpose of this protocol is to systematically evaluate whether adjuvants can enhance phagocytosis and the expression of immune cells in in vitro cell culture and to elaborate on the main experimental methods. The experiment is divided into four subsections: (1) the toxicity of OP-D and NOD to L929 cells is determined by the cell counting kit-8 (CCK-8) assay; (2) the cytokine levels of endocrine IFN-γ and IL-17A and the corresponding cell numbers in immunized mice are detected by splenocyte stimulation and ELISpot assays; (3) the antigen presentation ability of DCs after adjuvant stimulation is observed using confocal microscopy; and (4) the three kinds of cytokines, IL-1β, IL-6, and TNF-α, in the supernatants obtained from peritoneal macrophages (PMs) in normal mice cocultured with adjuvants are detected.
Protocol
All cell experiments were performed in a cell engineering laboratory equipped with basic operating rooms, buffer rooms, sterile culture rooms, and identification and analysis rooms. The working environment and conditions were free from microbial contamination and other harmful factors. The animal experiments were conducted based on the Guidelines for the Care and Use of Laboratory Animals and were approved by the Laboratory Animal Welfare and Ethics Committee of the Third Military Medical University.
1. Autoclaving and material preparation
- Prepare the reagents and consumables, such as phosphate-buffered saline (PBS), scissors, forceps, and abrasive mesh, by moist heat sterilization by autoclaving at 121 °C for 20 min.
- For the required reagents and equipment, see the Table of Materials. For the formula of the blank nanoemulsion (BNE), check Table 1.
2. L929 cytotoxicity assay
- Turn on the water bath and adjust the temperature to 37 °C. Collect one tube of frozen L929 cells from liquid nitrogen and thaw quickly in a 37 °C water bath.
- Pipette the cells into a 15 mL sterile centrifuge tube quickly after thawing, add 2 mL of DMEM, and mix well.
- Centrifuge the samples at 129 x g for 5 min and discard the supernatant. Then, add 2mL of DMEM to resuspend the cells, and centrifuge the samples again at 129 x g for 5 min.
- Discard the supernatant, add 6 mL of DMEM complete medium (containing 10% FBS) for resuspension, and transfer to a T25 culture flask in a 37 °C incubator with 5% CO2 to culture for 48 h.
- Discard the culture medium in the culture flask and wash the cells twice with 2 mL of PBS. Then, add 1 mL of 0.25% trypsin to digest the cells for 1-2 min at 37 °C.
- When rounding of the cells is observed, add 4 mL of DMEM complete medium to terminate digestion immediately and mix well. Then, aspirate the cells into a 15 mL sterile centrifuge tube and centrifuge at 129 x g for 5 min.
- Remove the supernatant and resuspend the cells in 1 mL of DMEM complete medium. Use a 20 µL cell suspension for cell counting using cell counting plates and dilute the remaining cells to 1 x 105 cells/mL with DMEM complete medium.
- Add 100 µL of ultrapure water to the periphery of a 96-well plate and add 100 µL of cell diluent to the internal wells only. Place the plate in the incubator for adherent culture for 4 h at 37 °C.
- After the cells adhere, add OP-D and NOD separately in DMEM complete medium to a final volume of 200 µL/well (the final concentrations of each drug are 480 µg/mL, 240 µg/mL, 120 µg/mL, 60 µg/mL, and 30 µg/mL). For each concentration, use three wells as replicates. Then, place the cells back into the incubator and culture for another 24 h.
- Dilute CCK-8 to 10% with DMEM complete medium and add 100 µL/well dilutions containing the adjuvant and cell solutions to the 96-well plate. Place the plate back into the incubator and incubate for another 2-3 h.
- Mix frequently while plating the cell solution to prevent inhomogeneity due to cell precipitation. Gently shake the plate several times before and after adding the CCK-8 to mix the medium and CCK-8 solution well.
- Measure the absorbance at 450 nm using a microplate reader. Set up a zeroing well with only medium and CCK-8 for a baseline absorbance value. Calculate accurate absorbance values by subtracting the zeroed absorbance value from the obtained absorbance value when plotting.
- Confirm that no bubbles are present in any wells before testing with the microplate reader because bubbles will interfere with the assay.
3. Splenocyte stimulation
- Immunize BALB/c mice aged 6-8 weeks with 30 µg of protein antigen plus 30 µg of adjuvant via an intramuscular injection (200 µL) on day 0, day 7, and day 14 according to the following experimental groups: (1) PBS group, (2) antigen (Ag) group, (3) antigen + OP-D (Ag/OP-D) group, (4) antigen + BNE (Ag/BNE) group, (5) antigen + NOD (Ag/NOD) group, and (6) antigen + AlPO4 (Ag/Al) group.
- Preparation room: On day 24 after the primary immunization, remove the mice from the animal room and euthanize them by an intraperitoneal injection of 100 mg/kg of 1% sodium pentobarbital. Place the mice in a glass dish and soak in 75% alcohol for 5 min.
- Place the centrifuge tubes on a centrifuge tube rack, number the disposable Petri dishes, and add 5 mL of PBS to each Petri dish with a 10 mL pipette.
- Make a 6-8 cm incision with scissors in the middle of the left ventral side of the mouse, tear open the skin, expose the abdominal wall, and locate the long red strip of the spleen.
- Lift the peritoneum on the inferior side of the spleen with forceps, cut it open, and turn it upward to expose the spleen. Lift the spleen with forceps, separate the connective tissue beneath the spleen with ophthalmic scissors, and remove the spleen.
- Place the spleen in a Petri dish containing 5 mL of PBS and mill with a sieve (200 mesh, 70 µm) and grinding bar. After grinding, transfer the liquid into a 15 mL centrifuge tube with an elbow dropper in accordance with the numbering.
- Centrifuge the liquid at 453 x g for 5 min. Discard the supernatant, add 3 mL of red blood cell lysis buffer to each tube, resuspend the cells, and lyse at room temperature for 10 min.
- Add 10-12 mL of PBS to each tube, mix the tube upside down, and centrifuge at 453 x g for 5 min. Discard the supernatant, add 10 mL of PBS to each centrifuge tube, and resuspend the cells.
- Take 20 µL of each sample in a well of the cell counting plate and record the number of live cells using an automated cell counter.
- Centrifuge the samples at 453 x g for 5 min and discard the supernatant. Resuspend the cells, dilute to 2.5 x 106 cells/mL with RF-10 medium (formulation information in Table 2), and add to a 96-well plate at 100 µL/well.
- Dilute the antigen with RF-10 medium to 10 µg/mL, add 100 µL to each well, and incubate for 3 days at 37 °C in 5% CO2.
- Aspirate the cell suspension obtained from each group of cells in 1.5 mL centrifuge tubes, centrifuge at 453 x g for 20 min, and aspirate the supernatant into a clean centrifuge tube.
- Carry out IFN-γ and IL-17A content detection strictly according to the ELISA kit instructions. The methods and procedures are as follows.
- Prepare 1x washing buffer working solution (provided with the kit), standard gradient concentration solution (dilute cytokine standard solution to 500 pg/mL, 250 pg/mL, 125 pg/mL, 62.5 pg/mL, 31.3 pg/mL, and 15.6 pg/mL in the dilution buffer R [1x] provided with the kit), biotinylated antibody working solution (dilute biotinylated antibody solution to 1:100 using the dilution buffer R [1x] provided with the kit to form the working solution), and streptavidin-HRP working solution as needed.
- Add 100 µL/well of diluted cytokine standard solution into the standard well, 100 µL/well of sample into the sample well (the dilution buffer R [1x] provided with the kit is used for the sample dilution), and 100 µL/well of dilution buffer R (1x) into the blank control well.
- Add biotinylated antibody working solution at 50 µL/well. Mix well, cover with a sealing membrane, and incubate at 37 °C for 90 min.
- Remove the liquid from the wells and add 1x washing buffer working solution at 300 µL/well. Discard the liquid from the wells after 1 min. Repeat this process 4x allowing the liquid to dry on filter paper each time.
- Add 100 µL/well of streptavidin-HRP working solution. Cover and incubate the samples at 37 °C for 30 min. Centrifuge the samples at 453 x g for 5 min and discard the supernatant.
NOTE: The washing solution remaining in the reaction well during the washing process should be thoroughly patted until no watermark can be seen on the filter paper. - Add TMB at 100 µL/well, incubate the plates at 37 °C for 5-30 min in the dark, and judge the termination reaction according to the depth of color in the well (dark blue). Usually, 10-20 min for color development can achieve good results.
- Terminate the reaction quickly by adding stop solution at 100 µL/well. Detect the absorbance value at 450 nm within 10 min after termination.
NOTE: Equilibrate the reagent at room temperature for 30 min before use.
4. ELISpot assay
- Perform immunization of the mice and the collection of splenocytes exactly as described in steps 3.1-3.10 above. Perform the assays for IFN-γ and IL-17A in strict accordance with the kit instructions. The methods and procedures are as follows.
- Remove the plate from the sealed package, wash 4x with sterile PBS (200 µL/well), and add 1640 complete culture medium (200 µL/well) to balance it at room temperature for 2 h.
- Remove the medium and dilute the splenocyte suspension with RF-10 medium to 2 x 105 cells/mL, adding 50 µL of cells and antigen per well (final concentration: 10 µg/mL).
- Place the plate in a humidified incubator at 37 °C with 5% CO2 for 48 h. Do not move the plate during this time, and take measures to avoid evaporation (e.g., wrap the plate with aluminum foil).
- Dilute the detection antibody (BVD6-24G2-biotin) to 1 µg/mL (1:1,000) in phosphate buffered saline (0.5 mL:100 mL) containing 0.5% fetal bovine serum (PBS-0.5% FBS). Add 100 µL/well to the plate, and incubate it at room temperature for 2 h after filtration through a 0.22 µm membrane.
- Decant the liquid in the wells, add 1x washing buffer at 200 µL/well, and wash 5x. Leave for 30-60 s each time, and for the last time, allow to dry on blotting paper.
- Dilute the streptavidin-horseradish peroxidase (1:1,000) in PBS-0.5% FBS and add 100 µL/well. Incubate the plate for 1 h at room temperature. Wash the plate as in step 4.6.
- Add 100 µL/well of ready-to-use TMB substrate solution and develop until a clear spot appears. Stop the color development by washing extensively in deionized water (rinse 5x-6x repeatedly). If necessary, remove the culvert (the soft plastic under the plate), and rinse the lower side of the membrane.
- Examine and count the spots on an ELISpot reader or dissecting microscope after the plate has dried.
5. Uptake by DCs
- Euthanize BALB/c normal mice by an intraperitoneal injection of 100 mg/kg of 1% sodium pentobarbital. Soak the mice in 75% alcohol for 5 min.
- Cut a 6-8 cm incision below the abdomen of the mouse with scissors, and clamp the two ends of the opening to separate it in different directions and expose the legs of the mouse. Separate the mouse femur from the mouse body and the tibia from the joint, and keep the bones intact at both ends.
- Remove the residual tissue and cartilage from the articular joints at both ends of the femur with scissors and forceps. Soak the femurs in 75% alcohol for 5 min, and then soak in sterile PBS solution to wash off the surface alcohol.
- Cut off the ends of the femurs with scissors, and rinse the bone marrow in a sterile Petri dish with sterile PBS solution followed by aspiration with a 1 mL syringe. Repeat the washing 3x-5x.
- Filter by a cell sieve (200 mesh, 70 µm) and collect the BMDCs into a 15 mL centrifuge tube. Centrifuge the samples at 290 x g for 5 min. Discard the supernatant, add 4 mL of red blood cell lysis buffer, resuspend, and lyse at room temperature for 5 min.
- Add 10 mL of sterile PBS solution to neutralize the lysate, centrifuge at 290 x g for 5 min, and discard the supernatant.
- Resuspend the cells in 1 mL of DMEM containing 1% penicillin-streptomycin solution and 10% FBS and count. Then, add GM-CSF (20 ng/mL) plus IL-4 (10 ng/mL) to the medium, adjust the cell concentration to 5 x 105/mL, and inoculate the cells on coverslips.
- Add the cell suspension to a 6-well plate at 2 mL/well, and place the plate in a humidified incubator at 37 °C with 5% CO2 for 48 h. Change the medium completely after 2 days, and change half of the medium after 4 days.
- Select five wells with cells in good condition (large and radiolucent cells with dendritic protrusions on the cell surface) using an inverted microscope at 100x magnification for the experiment on the seventh day of culture. Discard the supernatant, add 2 mL of GFP, OP-D + GFP, and NOD + GFP solutions diluted with DMEM complete medium (GFP final concentration: 20 µg/mL; adjuvant final concentration: 10 µg/mL) to each well, and incubate the plates at 37 °C for 30 min in the dark.
- Wash the plates 3x with PBS, add 1 mL of 4% paraformaldehyde to each well, and incubate at room temperature for 15 min. Remove the paraformaldehyde after fixation, incubate the cells with phalloidin and DAPI to a final concentration of 10 µg/mL for 10 min for staining, and then wash 3x with PBS.
- Add 1 mL of PBS to each well, and observe the antigen uptake using CLSM, as described below.
- Open the CLSM software, click on ZEN System, and wait for the hardware initialization to complete.
- Click on the GFP and DAPI shortcuts in locate tab to find the area that can be observed. Turn off the fluorescent light and transmitted light.
- Click on Smart Setup in acquisition menu to open the dye library, and add three fluorescent dyes: EGFP, phalloidin, and DAPI. Click on Best Signal > OK. Click on the EGFP channel in channels tab and click on Live to select the correct field of view on the right interface.
- Select 1 AU for the pinhole, rotate the fine focusing screw to adjust the focal length, and select the appropriate focal plane. Click on Range Indicator and adjust the combination of laser power and master gain so that only sporadic red dots appear on the image.
- Adjust the phalloidin and DAPI channels with the same parameters without changing the laser power.
- Select Stop Live and click on Acquisition Mode to change the shooting parameters: Frame Size: 1024 pixels x 1024 pixels; Scan Speed: 7; Averaging: 2x. Click on Snap and select Split to view all the images taken.Save the images.
6. Macrophage activation
- Immerse C57BL/6 mice in 75% alcohol after euthanasia and place them face up in a glass Petri dish in numbered order.
- Pass the mice through the transfer window into the sterile operation room and place on the operation table for 5 min.
- Using a syringe, aspirate 10 mL of saline, tilt the mice downward at approximately 45°, and inject into the middle of the abdominal cavity. Draw about 5 mL of cell suspension into a 15 mL centrifuge tube for each 10 mL and repeat the injection 3x.
- Centrifuge the cell suspension at 129 x g for 5 min to obtain mouse peritoneal primary macrophages. Resuspend the cells, adjust the cell concentration to 2 x 106 cells/mL with RPMI 1640 complete medium (containing 10% FBS), and inoculate the cell suspension in a 24-well plate to ensure a consistent number of cells per well (1 mL/well).
- Culture at 37 °C in 5% CO2 overnight (approximately 16-20 h), followed by incubation with PBS, Ag, Ag/OP-D, Ag/NOD, and Ag/Al (Ag final concentration: 5 µg/mL; adjuvant final concentration: 10 µg/mL; total volume: 2 mL) for 24 h. Detect the levels of IL-1β, IL-6, and TNF-α in the culture supernatant with ELISA kits using the methods and procedures described in steps 3.12-3.19.
Representative Results
The cellular activity evaluation of the adjuvants OP-D and NOD was completed in vitro according to the protocol. L929 fibroblasts are a useful screening model for the in vitro toxicity testing of NOD (Figure 1). The quantification of inflammatory cytokine levels in the spleen can help researchers better understand the immune response (Figure 2). Monitoring CTLs with ELISpot is the gold standard for assessing antigen-specific T-cell immunity in clinical trials and for screening vaccine candidates (Figure 3). The increased uptake of an antigen by DCs can elicit enhanced adaptive immune responses (Figure 4). Macrophages play an important role in presenting antigens to T cells, as well as inducing other antigen-presenting cells to express costimulatory molecules, thereby initiating adaptive immune responses (Figure 5). The above experimental results were published by Tong et al., and the different antibody responses in vivo and protection efficiency against mice can be found in the original article14.
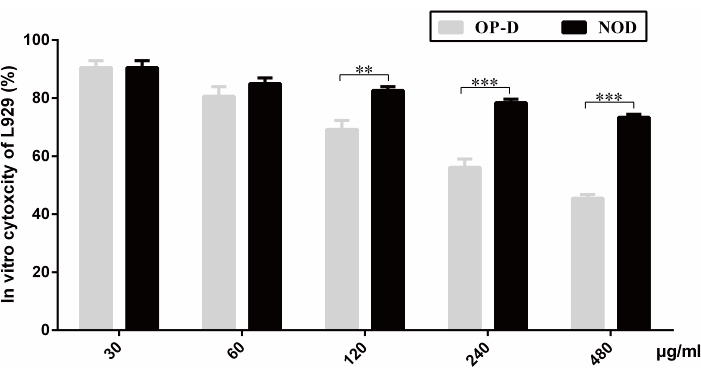
Figure 1: In vitro cytotoxicity test of L929 cells. The cytotoxic effects of different gradient concentrations of OP-D and NOD (30 µg/mL, 60 µg/mL, 120 µg/mL, 240 µg/mL, and 480 µg/mL) when incubated with L929 cells are shown. A CCK-8 kit was used for detection. Statistical analysis was performed using a statistical analysis software. Differences between the two groups were analyzed using an unpaired, two-tailed Student's t-test. All values are expressed as mean ± SD (n = 3), and significant differences are expressed as follows: *p < 0.05, **p < 0.01, and ***p < 0.001. This figure has been modified from Tong et al.14. Please click here to view a larger version of this figure.
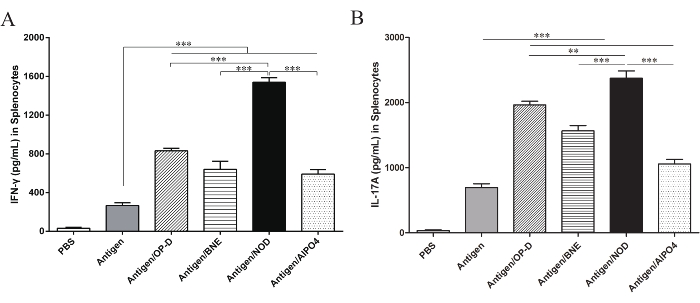
Figure 2: Levels of IFN-γ and IL-17A in splenocytes. Splenocytes from vaccinated mice were stimulated with the antigen for 3 days, and the levels of the cytokines (A) IFN-γ and (B) IL-17A in the supernatant were measured by ELISA. The results showed that IFN-γ and IL-17A production were significantly increased in the Ag/NOD group compared with the Ag/OP-D, Ag/BNE, and Ag/Al groups (p < 0.01). Statistical analysis was performed using a statistical analysis software. Differences among the multiple groups were analyzed using one-way ANOVA followed by Tukey's multiple comparison test. All values are expressed as mean ± SD (n = 8), and significant differences are expressed as follows: *p < 0.05, **p < 0.01, and ***p < 0.001. This figure has been modified from Tong et al.14. Please click here to view a larger version of this figure.
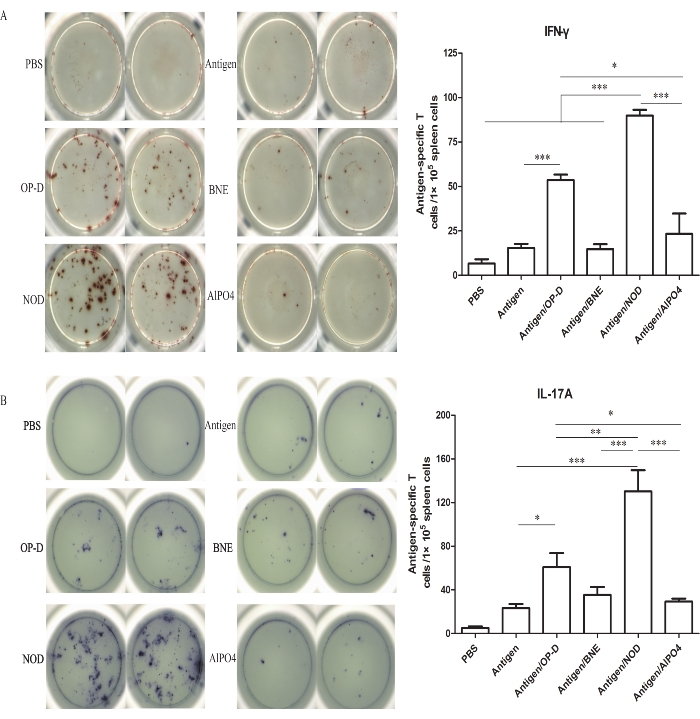
Figure 3: Number of IFN-γ- and IL-17A-secreting cells in the splenocyte population. (A) ELISpot analysis of IFN-γ spot-forming antigen-specific T cells among the splenocytes. (B) ELISpot analysis of IL-17A spot-forming antigen-specific T cells among the splenocytes. Similar to the cytokine results, the Ag/OP-D and Ag/NOD groups showed significantly increased ratios and numbers of IFN-γ- and IL-17A-forming cells in the splenic lymphoid T cell population. The Ag/NOD group induced stronger Th1 (p < 0.001) and Th17 (p < 0.01) immune responses than the other groups. Statistical analysis was performed using a statistical analysis software. Differences among the multiple groups were analyzed using one-way ANOVA followed by Tukey's multiple comparison test. All values are expressed as mean ± SD (n = 8), and significant differences are expressed as follows: *p < 0.05, **p < 0.01, and ***p < 0.001. This figure has been modified from Tong et al.14. Please click here to view a larger version of this figure.
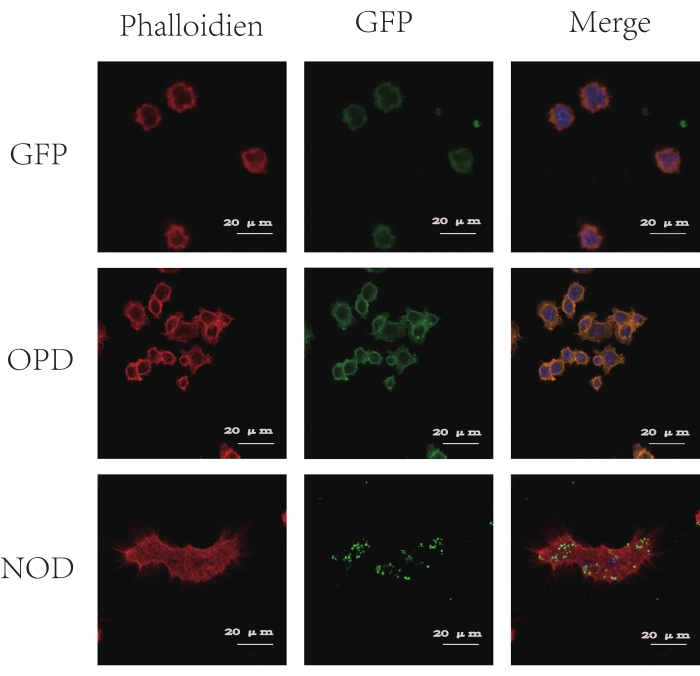
Figure 4: CLSM images of antigen uptake by BMDCs. Phalloidin stains the cytoskeleton in red, DAPI stains the nucleus in blue, and GFP presents green fluorescence. As shown in the figure, green fluorescence is observed in CLSM after 30 min of coincubation of the GFP + OP-D and GFP + NOD groups with BMDCs, but the GFP + NOD particles are surrounded by phagosome-like vesicular structures, while the GFP + OP-D particles are not. This figure has been modified from Tong et al.14. Please click here to view a larger version of this figure.
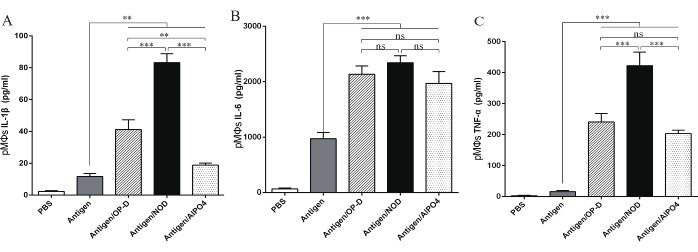
Figure 5: Impact of adjuvant-formulated antigen on the activation of PMs. ELISA for the detection of the concentrations of the cytokines IL-1β, IL-6, and TNF-α in the supernatant of PMs coincubated with PBS, Ag, Ag/OP-D, Ag/NOD, and Ag/Al. Compared with antigen stimulation, Ag/NOD, Ag/OP-D, and Ag/Al stimulation all significantly increased IL-1β, IL-6, and TNF-α secretion from the PMs (p < 0.05). The activation of macrophages was significantly improved in the NOD group compared with the OP-D and AlPO4 groups (p < 0.05). Statistical analysis was performed using a statistical analysis software. Differences among the multiple groups were analyzed using one-way ANOVA followed by Tukey's multiple comparison test. All values are expressed as mean ± SD (n = 8), and significant differences are expressed as follows: *p < 0.05, **p < 0.01, and ***p < 0.001. This figure has been modified from Tong et al.14. Please click here to view a larger version of this figure.
| Reagent | Density | Mass(per 10g) |
| Cremophor EL-35 | bulk | 1.92 |
| glycerol | bulk | 0.48 |
| GTCC | bulk | 0.6 |
| Ultrapure water | bulk | residual amount |
Table 1: The formula of BNE.
| Reagent | Density | Volume |
| β- Mercaptoethanol | 50µM | 0.366µL |
| Fetal Bovine Serum | 1X | 10mL |
| Glutamax | 2mM | 1mL |
| Glutamax RPMI 1640 | 1X | 85mL |
| HEPES | 10mM | 1mL |
| Non-essential amino acids(100x) | 1X | 1mL |
| Penicillin-Streptomycin Solution | 100U/mL | 1mL |
| Sodium pyruvate(100 mM) | 1mM | 1mL |
Table 2: Preparation information for the RF-10 complete medium.
Discussion
Subunit vaccines provide excellent safety but poor immunogenicity. The main strategy to enhance the immunogenicity is to physically adsorb or couple antigens with adjuvants and incorporate them into the drug delivery systems to promote the uptake and presentation by DCs. Natural plant saponins such as quillaia saponin and its derivatives are highly toxic and are not suitable for the development of human vaccines17. Therefore, the study of the toxic effects of vaccines or adjuvants on cells is a necessary first step in the evaluation of new vaccines.
The protocol presented in this study is performed according to ISO 10993-5:200918, which allows some flexibility in sample fabrication. The standard toxic cell line, L929 fibroblasts, and gingival fibroblasts have similar levels of cytotoxicity. However, L929 fibroblasts have become a useful screening model for in vitro toxicity tests of nanomaterials because of their excellent reproducibility19. MTT and CCK-8 are commonly used for cell viability and cytotoxicity assays. The results of MTT and CCK-8 assays contradict each other and are not significantly correlated, but the cell viability of the CCK-8 assay is significantly different from that of the MTT assay20. A possible explanation for the MTT results in the previous study is that accelerating cell death can be induced at higher MTT concentrations21. The experimental results of the CCK-8 method are generally consistent with the results of animal toxicity tests22. Therefore, until new cytotoxicity evaluation methods are available, the use of the CCK-8 assay to detect the toxicity of OP-D and NOD to L929 cells is probably the best option at present. This method will also continue to be applied in the field of vaccine materials and adjuvant evaluation.
The spleen is the largest secondary lymphoid organ in the human body, and the quantification of inflammatory cytokine levels in the spleen may help us understand the immune response23. It is believed that there are some fundamental differences in the structure and cell types between the spleens of mice and humans24, but the basic similarity of specific immune cell types and the function of the spleen region make studies using the mice spleen T cells relevant24. In this protocol, we measured the secretory levels of the Th1 cytokine IFN-γ and the Th17 cytokine IL-17A in the spleen using ELISA kits. This assay is usually used for quantitative determinations and has high sensitivity because it uses high-affinity antibodies to wash away nonspecific substances. The main limitations of this study are the long measuring time and the high consumption of reagents. Cytokines can also be detected with flow cytometry and Luminex methods, but these methods require complex instruments, as well as expensive raw materials and specialized training. Therefore, this simple and economical ELISA kit is a valuable tool for measuring specific immune responses. ELISpot has become one of the most commonly used techniques for determining the immune responses of specific cytokine spot-forming cells. It can be used not only to detect CD8+ T cell responses elicited by vaccine candidates but also for the recognition of specific antigens after immunization25. With high-throughput screening and a sensitive detection limit (1/100,000 cells), ELISpot is widely used as it also offers advantages of direct observation of cells and rapid analysis. The formation of each spot indicates the frequency of activation of individual T cells or B cellsTheevaluation of cellular response to vaccines and adjuvants is of great significance which makes ELISpot irreplaceable at present.
The presentation of antigens by DCs is a prerequisite for eliciting immune responses14. DCs, which are used for antigen uptake, migration to lymph nodes, and the activation of naive T cells, are one of the essential cell types for the development of T cell-mediated immune responses14. Considering that the interaction of nanoemulsion particles with the cell membrane is a key determinant of particle uptake, GFP phagocytosis within DCs was determined using CLSM in this experimental protocol. It has been shown that DCs can efficiently transport antigens to draining lymph nodes, which may be why adjuvants enhance antigen immunogenicity in vivo. In addition, CLSM is the most common commercial implementation of the technique and is widely used in imaging laboratories. The optical sectioning capability, clear resolution, and versatility of the 3D imaging26 of CLSM make it the best tool for analyzing antigen uptake by DCs, even if it cannot be used for the collection of quantitative data.
The major histocompatibility complex (MHC I and II) is important for the specific recognition of antigens. MHC II functional molecules are highly expressed in APCs and function to induce CD4+ T cell activation. APCs include macrophages, DCs, and B lymphocytes27, which strongly modulate adaptive immunity. Macrophages are widely distributed in the host immune system and play a key role in defense and homeostasis28. The activation of macrophages is essential for initiating adaptive immune responses29. Meanwhile, nanoemulsion adjuvants that are the same size as pathogens can promote antigen recognition and phagocytosis, activate NALP3 inflammasomes and macrophages, and modulate antigen presentation28. In this protocol, PMs were mainly used as a model to determine the secretion of the proinflammatory cytokines IL-1β andTh2, cytokines IL-6, and TNF-α by ELISA, which can be used to qualitatively evaluate the macrophage activation ability of vaccines and adjuvants. However, the degree and mechanism of activation need to be determined by more experiments. For example, whether EGF, IL-6, and other factors necessary for the activation of immune cells are secreted and the related signaling pathways (JAK-STAT, JNK, PI3K-Akt, etc.) need to be studied.
In summary, a series of protocols to confirm the in vitro cellular responses to novel adjuvants, including cytotoxicity, cytokine secretion, DC uptake, and macrophage activation have been established. These protocols not only demonstrate low toxicity and high cellular delivery but also provide detailed procedures for CCK-8, ELISA, and ELISpot. Cellular response assessments of the plant-derived immunopotentiator OP-D and its modified powerful nanoemulsion vaccine adjuvant NOD were completed in vitro, and the protocol was effective. Although ELISA, ELISpot, and confocal laser scanning techniques have classically been used to evaluate the in vitro immunocompetence of adjuvants to cells, these methods have many disadvantages, such as long measurement times, heavy workloads, expensive materials, and the need for professional technicians. Many accurate methods and advanced technologies, such as gene chips, single-cell sequencing, and transcriptome technology, need to be used in future studies to further expand the scope of the technique.
Divulgations
The authors have nothing to disclose.
Acknowledgements
This study was supported by grant No. 2021YFC2302603 of the National Key Research and Development Program of China, grants No. 31670938, 32070924, 82041045, and 32000651 of the National Natural Science Foundation Program of China, grants No. 2014jcyjA0107 and No. 2019jcyjA-msxmx0159 of the Natural Science Foundation Project Program of Chongqing, grant No. CYS21519 of the Postgraduate Research and Innovation Project of Chongqing, grant No. 2020XBK24 of the Army Medical University Special projects, and grant No. 202090031021 of the National Innovation and Entrepreneurship Program for college students.
Materials
| 0.25% Trypsin-EDTA (1x) | GIBCO, USA | 25200056 | |
| 96-well filter plates | Millipore. Billerica, MA | CLS3922 | |
| AlPO4 | General Chemical Company, USA | null | |
| Automated Cell Counter | Countstar, China | IC1000 | |
| BALB/c mice and C57BL/6 mice | Beijing HFK Bioscience Co. Ltd | null | |
| caprylic/capric triglyceride (GTCC) | Beijing Fengli Pharmaceutical Co. Ltd., Beijing, China | null | |
| CCK-8 kits | Dojindo, Japan | CK04 | |
| Cell Counting Plate | Costar, Corning, USA | CO010101 | |
| Cell Sieve | biosharp, China | BS-70-CS | |
| Centrifuge 5810 R | Eppendorf, Germany | 5811000398 | |
| DAPI | Sigma-Aldrich, St. Louis, USA | D9542 | |
| DMEM basic(1x) medium | GIBCO, USA | C11885500BT | |
| DSZ5000X Inverted Microscope | Nikon,Japan | DSZ5000X | |
| EL-35 (Cremophor-35) | Mumbai, India | null | |
| ELISpot classic | AID, Germany | ELR06 | |
| Fetal Bovine Serum | GIBCO, USA | 10099141C | |
| Full-function Microplate Reader | Thermo Fisher Scientific, USA | VL0000D2 | |
| GFP | Sigma-Aldrich, St. Louis, USA | P42212 | |
| Glutamax | Invitrogen, USA | 35050061 | |
| Granulocyte Macrophage Colony-Stimulating Factor | GM-CSF, R&D Systems, USA | 315-03 | |
| HEPES | Invitrogen, USA | 15630106 | |
| HF 90/240 Incubator | Heal Force, Switzerland | null | |
| IL-4 | PeproTech, USA | 042149 | |
| L929 cell line | FENGHUISHENGWU, China | NCTC clone 929 (RRID:CVCL_0462) | |
| Laser Scanning Confocal Microscopy | Zeiss, Germany | LSM 980 | |
| MONTANE 85 PPI | SEPPIC, France | L12910 | |
| MONTANOX 80 PPI | SEPPIC, France | 36372K | |
| Mouse IFN-γ ELISA kit | Dakewe, China | 1210002 | |
| Mouse IFN-γ precoated ELISPOT kit | Dakewe, China | DKW22-2000-096 | |
| Mouse IL-17A ELISA kit | Dakewe, China | 1211702 | |
| Mouse IL-17A ELISpotPLUS Kit | ebiosciences, USA | 3521-4HPW-2 | |
| Mouse IL-1β ELISA kit | Dakewe, China | 1210122 | |
| Mouse IL-6 ELISA kit | Dakewe, China | 1210602 | |
| Mouse TNF-α ELISA kit | Dakewe, China | 1217202 | |
| Non-essential amino acids(100x) | Invitrogen, USA | 11140050 | |
| Ophiopogonin-D | Chengdu Purui Technology Co. Ltd | 945619-74-9 | |
| Penicillin-Streptomycin Solution | Invitrogen, USA | 15070063 | |
| Phalloidin | Solarbio, China | CA1620 | |
| Phosphate Buffered Saline | ZSGB-BIO, China | ZLI-9062 | |
| Red Blood Cell Lysis Buffer | Solarbio, China | R1010 | |
| RPMI 1640 medium | Hyclone (Life Technology), USA | SH30809.01 | |
| Sodium pyruvate(100 mM) | Invitrogen, USA | 11360070 | |
| Squalene | Sigma, USA | S3626 | |
| β- Mercaptoethanol | Invitrogen, USA | 21985023 |
References
- Cao, W., et al. Recent progress of graphene oxide as a potential vaccine carrier and adjuvant. Acta Biomaterials. 112, 14-28 (2020).
- Ko, E. J., Kang, S. M. Immunology and efficacy of MF59-adjuvanted vaccines. Human Vaccines & Immunotherapeutics. 14 (12), 3041-3045 (2018).
- Shi, S., et al. Vaccine adjuvants: Understanding the structure and mechanism of adjuvanticity. Vaccine. 37 (24), 3167-3178 (2019).
- Kuo, T. Y., et al. Development of CpG-adjuvanted stable prefusion SARS-CoV-2 spike antigen as a subunit vaccine against COVID-19. Scientific Reports. 10, 20085 (2020).
- Twentyman, E., et al. Interim recommendation of the Advisory Committee on Immunization Practices for use of the Novavax COVID-19 vaccine in persons aged >/=18 years – United States, July 2022. MMWR Morbidity and Mortality Weekly Report. 71 (31), 988-992 (2022).
- Wang, Z., et al. Improved aluminum adjuvants eliciting stronger immune response when mixed with hepatitis B virus surface antigens. ACS Omega. 7 (38), 34528-34537 (2022).
- Wang, N., Chen, M., Wang, T. Liposomes used as a vaccine adjuvant-delivery system: From basics to clinical immunization. Journal of Controlled Release. 303, 130-150 (2019).
- Akin, I., et al. Evaluation of the safety and efficacy of Advax(TM) as an adjuvant: A systematic review and meta-analysis. Advances in Medical Sciences. 67 (1), 10-17 (2022).
- Lacaille-Dubois, M. A. Updated insights into the mechanism of action and clinical profile of the immunoadjuvant QS-21: A review. Phytomedicine. 60, 152905 (2019).
- Marty-Roix, R., et al. Identification of QS-21 as an inflammasome-activating molecular component of saponin adjuvants. The Journal of Biological Chemistry. 291 (3), 1123-1136 (2016).
- Zhang, Y. Y., et al. Ophiopogonin D attenuates doxorubicin-induced autophagic cell death by relieving mitochondrial damage in vitro and in vivo. The Journal of Pharmacology and Experimental Therapeutics. 352 (1), 166-174 (2015).
- An, E. J., et al. Ophiopogonin D ameliorates DNCB-induced atopic dermatitis-like lesions in BALB/c mice and TNF-alpha- inflamed HaCaT cell. Biochemical and Biophysical Research Communications. 522 (1), 40-46 (2020).
- Song, X., et al. Effects of polysaccharide from Ophiopogon japonicus on immune response to Newcastle disease vaccine in chicken. Pesquisa Veterinária Brasileira. 36 (12), 1155-1159 (2016).
- Tong, Y. N., et al. An immunopotentiator, ophiopogonin D, encapsulated in a nanoemulsion as a robust adjuvant to improve vaccine efficacy. Acta Biomaterialia. 77, 255-267 (2018).
- Lin, C. A., et al. Hyaluronic acid-glycine-cholesterol conjugate-based nanoemulsion as a potent vaccine adjuvant for T cell-mediated immunity. Pharmaceutics. 13 (10), 1569 (2021).
- Xu, H. H., et al. Global metabolomic and lipidomic analysis reveals the potential mechanisms of hemolysis effect of ophiopogonin D and ophiopogonin D’ in vivo. Chinese Medicine. 16 (1), 3 (2021).
- Drane, D., Gittleson, C., Boyle, J., Maraskovsky, E. ISCOMATRIX adjuvant for prophylactic and therapeutic vaccines. Expert Review of Vaccines. 6 (5), 761-772 (2007).
- Rudolf, R., et al. Microstructure characterisation and identification of the mechanical and functional properties of a new PMMA-ZnO composite. Materials. 13 (12), 2717 (2020).
- Cannella, V., et al. Cytotoxicity evaluation of endodontic pins on L929 cell line. BioMed Research International. 2019, 3469525 (2019).
- Jiao, G., et al. Limitations of MTT and CCK-8 assay for evaluation of graphene cytotoxicity. RSC Advances. 5 (66), 53240-53244 (2015).
- Ghasemi, M., Turnbull, T., Sebastian, S., Kempson, I. The MTT assay: Utility, limitations, pitfalls, and interpretation in bulk and single-cell analysis. International Journal of Molecular Sciences. 22 (23), 12827 (2021).
- Li, W., Zhou, J., Xu, Y. Study of the in vitro cytotoxicity testing of medical devices. Biomedical Reports. 3 (5), 617-620 (2015).
- Wu, F., et al. Correlation between elevated inflammatory cytokines of spleen and spleen index in acute spinal cord injury. Journal of Neuroimmunology. 344, 577264 (2020).
- Lewis, S. M., Williams, A., Eisenbarth, S. C. Structure and function of the immune system in the spleen. Science Immunology. 4 (33), (2019).
- Cox, J. H., Ferrari, G., Janetzki, S. Measurement of cytokine release at the single cell level using the ELISPOT assay. Methods. 38 (4), 274-282 (2006).
- Elliott, A. D. Confocal microscopy: Principles and modern practices. Current Protocols in Cytometry. 92 (1), 68 (2020).
- Zhou, Y., et al. CD4(+) T cell activation and inflammation in NASH-related fibrosis. Frontiers in Immunology. 13, 967410 (2022).
- Martinez, F. O., Sica, A., Mantovani, A., Locati, M. Macrophage activation and polarization. Frontiers in Bioscience. 13, 453-461 (2008).
- Quesniaux, V., Erard, F., Ryffel, B. Adjuvant activity on murine and human macrophages. Methods in Molecular Biology. 626, 117-130 (2010).

