Isolation of Adipogenic and Fibro-Inflammatory Stromal Cell Subpopulations from Murine Intra-Abdominal Adipose Depots
Summary
This protocol describes the technical approach to isolate adipogenic and fibro-inflammatory stromal cell subpopulations from murine intra-abdominal white adipose tissue (WAT) depots by fluorescence-activated cell sorting or immunomagnetic bead separation.
Abstract
The stromal-vascular fraction (SVF) of white adipose tissue (WAT) is remarkably heterogeneous and consists of numerous cell types that contribute functionally to the expansion and remodeling of WAT in adulthood. A tremendous barrier to studying the implications of this cellular heterogeneity is the inability to readily isolate functionally distinct cell subpopulations from WAT SVF for in vitro and in vivo analyses. Single-cell sequencing technology has recently identified functionally distinct fibro-inflammatory and adipogenic PDGFRβ+ perivascular cell subpopulations in intra-abdominal WAT depots of adult mice. Fibro-inflammatory progenitors (termed, “FIPs”) are non-adipogenic collagen producing cells that can exert a pro-inflammatory phenotype. PDGFRβ+ adipocyte precursor cells (APCs) are highly adipogenic both in vitro and in vivo upon cell transplantation. Here, we describe multiple methods for the isolation of these stromal cell subpopulations from murine intra-abdominal WAT depots. FIPs and APCs can be isolated by fluorescence-activated cell sorting (FACS) or by taking advantage of biotinylated antibody-based immunomagnetic bead technology. Isolated cells can be used for molecular and functional analysis. Studying the functional properties of stromal cell subpopulation in isolation will expand our current knowledge of adipose tissue remodeling under physiological or pathological conditions on the cellular level.
Introduction
White adipose tissue (WAT) represents the principal site for energy storage in mammals. Within this tissue, adipocytes, or “fat cells,” store excess calories in the form of triglyceride, packaged into large unilocular lipid droplets. Moreover, adipocytes secrete a multitude of factors that regulate various aspects of energy homeostasis1,2,3. Adipocytes constitute the bulk of WAT volume; however, adipocytes only represent less than 50% of total cells found in WAT4,5. The non-adipocyte compartment of WAT, or stromal-vascular fraction (SVF), is quite heterogeneous and contains vascular endothelial cells, tissue-resident immune cells, fibroblasts, and adipocyte precursor cell (APC) populations.
WAT is exceptional in its remarkable capacity to expand in size as the demand for energy storage increases. Maintaining this tissue plasticity is essential as adequate storage of lipids in WAT protects against deleterious ectopic lipid deposition into non-adipose tissues6. The manner by which individual WAT depots undergo this expansion in response to caloric excess is a critical determinant of insulin sensitivity in the setting of obesity7. Pathologic WAT expansion, observed in obese individuals with metabolic syndrome, is characterized by preferential expansion of visceral WAT depots at the expense of metabolically favorable subcutaneous fat tissue. Moreover, insulin resistance in obesity is associated with pathologic remodeling of WAT. This is characterized by hypertrophic growth of existing adipocytes (increase in size), inadequate angiogenesis, chronic metabolic-inflammation, accumulation of extracellular matrix components (fibrosis), and tissue hypoxia8,9. These WAT phenotypes of obesity are associated with hepatic steatosis and insulin resistance, similar to what is observed in the condition of lipodystrophy (absence of functional WAT). In contrast, healthy WAT expansion is observed in the metabolically healthy obese population and is characterized by preferential expansion of protective subcutaneous WAT and depot expansion through adipocyte hyperplasia10. The recruitment of new adipocytes is mediated by de novo adipocyte differentiation from adipocyte precursor cells (APCs) (termed, “adipogenesis”). Adipocyte hyperplasia coincides with relatively lower degrees of WAT fibrosis and metabolic inflammation6,11. A multitude of cell types within the WAT microenvironment directly influence the health and expandability of WAT in obesity12. As such, defining the function of the various cell types present in WAT remains a high priority for the field.
Over the past decade, several strategies have been employed to define and isolate native APCs from human and mouse WAT SVF13. Such strategies isolate APCs based on the cell surface expression of common mesenchymal stem/progenitor cell markers using antibody-based cell separation techniques. These approaches include fluorescence-activated cell sorting (FACS), using fluorophore-labelled antibodies, or immunomagnetic bead separation (i.e., chemically modified antibodies). Cell surface proteins targeted for the isolation of APCs include PDGFRα, PDGFRβ, CD34, and SCA-1. These approaches have helped enrich for APCs; however, cell populations isolated based on these markers are quite heterogeneous. Very recent single-cell RNA-sequencing (scRNA-seq) studies have highlighted the molecular and functional heterogeneity of stromal cells within the isolated stromal-vascular fraction (SVF) of murine WAT14,15,16,17. From our own scRNA-seq and functional analyses, we have identified and characterized functionally distinct immune-modulating and adipogenic PDGFRβ+ perivascular cell subpopulations in the stromal compartment of intra-abdominal WAT in adult mice15. Fibro-inflammatory precursors, or FIPs, represent a prominent subpopulation of PDGFRβ+ cells and can be isolated based on LY6C expression (LY6C+ PDGFRβ+ cells)15. FIPs lack adipogenic capacity, exert a strong pro-inflammatory response to various stimuli, produce collagen, and secrete anti-adipogenic factors15. The pro-inflammatory and fibrogenic activity of these cells increases in association with obesity in mice, implicating these cells as regulators of WAT remodeling. The LY6C- CD9- PDGFRβ+ subpopulation represents adipocyte precursor cells (APCs). These APCs are enriched in the expression of Pparg and other pro-adipogenic genes, and readily differentiate into mature adipocytes in vitro and in vivo15. Here, we provide a detailed protocol for the isolation of these distinct cell populations from intra-abdominal WAT depots of adult mice using FACS, and immunomagnetic bead separation with biotinylated antibodies. This protocol can be used to isolate functionally distinct adipose progenitor subpopulations from multiple intra-abdominal WAT depots of adult male and female mice15. Studying these functionally distinct cell populations in isolation may contribute greatly to our current understanding of the molecular mechanisms that regulate adipogenesis and intra-abdominal adipose tissue remodeling in health and disease.
The protocol below details the isolation of adipose progenitors from murine epididymal WAT; however, the same procedure can be used to isolate corresponding cells from the mesenteric and retroperitoneal WAT depots of both male and female mice15. A detailed protocol on how to identify and isolate these depots in mice can be found in Bagchi et al.18. This protocol has been optimized for the use of mice 6-8 weeks of age. The frequency and differentiation capacity of APCs may decline in association with ageing.
Protocol
All animal protocols and procedures have been approved by the University of Texas Southwestern Medical Center Institutional Animal Use and Care Committee.
1. Isolation of stromal vascular fraction (SVF) from gonadal white adipose tissue
- Dissect the gonadal white adipose tissue from 6-8-week-old mice and place fat pads in 1x PBS solution.
- Combine up to 4 fat depots (2-4 depots from 1-2 mice recommended) and mince the tissue in a 10 mL beaker containing 200 µL of digestion buffer (1x HBSS, 1.5% BSA and 1 mg/mL collagenase D).
- Transfer the minced tissue to a 50 mL centrifuge tube containing 10 mL digestion buffer.
- Incubate mixture at 37 °C in a water bath for 1 h while shaking.
- Filter the digested tissue through a 100 µm cell strainer to remove undigested tissue.
- Dilute filtered sample to 30 mL with PBS containing 2% FBS, and centrifuge at 600 x g for 5 min at 4 °C. Aspirate the supernatant, which contains mature adipocytes.
- Proceed immediately to preferred cell isolation method.
2. Isolation of APCs and FIPs using FACS
- Dissolve the pellet in 1 mL of 1x RBC lysis buffer by shaking the tube gently.
- Incubate at RT for 1-2 min.
- Add 10 mL of 2% FBS/PBS and pass through a 40 µm cell strainer into a clean 50 mL centrifuge tube.
- Centrifuge at 600 x g for 5 min at 4 °C.
- Aspirate media and resuspend the pellet in 400-800 µL of 2% FBS/PBS containing Fc block (1:200).
- Incubate at 4 °C for 10 min.
- Transfer 400 µL-800 µL of cell suspensions containing ≤106 cells per mL to 1.5 mL tubes and add antibodies. Antibody concentrations are listed in the Table of Materials section.
- Prepare separate control tubes for 1) unstained cells, 2) single color controls, and 3) FMO (fluorescence minus one) controls.
- Stain the samples with PDGFRβ, CD45, CD31, CD9, LY6C antibodies.
- Incubate at 4 °C for 15 min protected from light.
- Centrifuge at 600 x g for 5 min at 4 °C.
- Aspirate media and resuspend cells in 400 µL of 2% FBS/PBS.
- Centrifuge at 600 x g for 5 min at 4 °C.
- Aspirate media and resuspend cells in 400-800 µL of 2% FBS/PBS. Then pass through 40 µm filter caps into 5 mL polystyrene round-bottom tubes for FACS.
- Follow the following steps for gating.
- Use unstained and single-color controls for compensation.
- Use FMO controls to set experimental gates.
- Use the gating strategy shown in Figure 1 to obtain APCs and FIPs. Gate APCs as CD45– CD31– PDGFRβ+ LY6C– CD9– and FIPs as CD45– CD31– PDGFRβ+ LY6C+ cells.
- Collect sorted cells in tubes containing 500 µL of 100% serum and maintain the cells on ice.
- Centrifuge cells at 600 x g for 5 min at 4 °C. Add 2% FBS/PBS to wash the cells by centrifuging again at 600 x g for 5 min at 4 °C. Discard the supernatant use the pelleted cells.
- Resuspend the pelleted cells in the appropriate volume of gonadal APC culture media (for cell culture) or appropriate buffer for subsequent analysis.
3. Immunomagnetic separation of adipogenic and non-adipogenic fractions
- Isolate SVF from gonadal white adipose tissue following steps 1.1-1.7.
- Aspirate the supernatant and resuspend the SVF pellet in 10 mL of 1x commercially available MS Buffer.
- Filter the cell suspension through a 40 µm cell strainer.
- Centrifuge at 600 x g for 5 min at 4 °C.
- Aspirate the supernatant and resuspend pelleted cells in 100 µL of 1x MS Buffer.
- Perform CD31+ and CD45+ cell depletion as discussed below (Figure 2A, Step 1). This is done to remove endothelial and hematopoietic lineage cells.
- Count cells using a cell counter and adjust the concentration to ≤ 1 x 108 cells/mL.
- Add the biotin conjugated CD31 and CD45 antibodies to the cell suspension, each at a concentration of ≤ 0.25 µg per 106 cells and incubate on ice for 15 min.
- Wash cells by adding 4 mL of 1x MS Buffer.
- Centrifuge at 600 x g for 5 min at 4 °C.
- Aspirate the supernatant and resuspend the pellet with 100 µL of 1x MS buffer.
- Add 10 µL of streptavidin nanobeads and incubate cells on ice for 15 min.
- Wash cells by adding 4 mL of 1x MS buffer.
- Centrifuge at 600 x g for 5 min at 4 °C, then aspirate the supernatant.
- Resuspend cells in 2.5 mL of 1x MS buffer and transfer to a 5 mL polypropylene tube.
- Place the tube in the magnet rack for 5 min.
- Collect unlabeled cells by pouring the cell suspension into a clean 15 mL centrifuge tube.
NOTE: Avoid shaking or blotting off hanging droplets as this leads to contamination from unwanted cell fraction. - Remove the tube from magnet and repeat steps 3.6.9. to 3.6.11. two more times for a total of 3 washes.
- Separation of adipogenic and non-adipogenic fractions (Figure 2A, Step 2)
- Continue working with unlabeled fraction (i.e., CD45– CD31– fraction).
- Centrifuge the 15 mL tube containing unlabeled cells at 600 x g for 5 min at 4 °C.
- Aspirate the supernatant and resuspend the pellet in 100 µL of 1x MS buffer.
- Add biotin conjugated LY6C and CD9 antibodies, respectively, at a concentration of ≤ 0.25 µg per 106 cells and incubate on ice for 15 min.
- Follow steps 3.6.3. to 3.6.12. to complete the second separation.
- Collect unbound fractions. Unlabeled cells (LY6C– CD9–) represents adipogenic fraction containing APCs (Figure 2A, Step 3).
- Remove tube from the magnet, resuspend and elute bound cells in 1x MS buffer. Eluates or labeled fraction (LY6C+ CD9+), represents non-adipogenic fraction containing FIPs (Figure 2A, Step 3).
- Centrifuge labeled and unlabeled fractions at 600 x g for 5 min to pellet cells at 4 °C.
- Proceed immediately to cell culture (step 6) or use undifferentiated precursors for preferred analyses (step 4 and/or step 5).
4. Assess purity of adipogenic and non-adipogenic fractions by flow cytometry
- Resuspend bead-isolated cell fractions in 200-400 µL of 2% FBS/PBS containing Fc block (1:200).
- Incubate at 4 °C for 10 min.
- Transfer the cell suspension to 1.5 mL tubes and add antibodies. Antibody concentrations are listed in the Table of Materials.
- Prepare separate control tubes for 1) unstained cells, 2) single color controls, and 3) FMO controls.
- To the samples, add CD45, CD31, CD9, and LY6C antibodies.
- Incubate at 4 °C for 15 min protected from light.
- Centrifuge at 600 x g for 5 minutes at 4 °C.
- Aspirate supernatant and resuspend cells in 400 µL of 2% FBS/PBS.
- Centrifuge the suspension at 600 x g for 5 min at 4 °C.
- Aspirate the supernatant and resuspend cells in 400-800 µL of 2% FBS/PBS. Filter through 40 µm filter caps into 5 mL polystyrene round-bottom tubes for analysis by flow cytometry.
- Flow cytometry analysis to assess purity
- Use unstained and single-color controls for compensation.
- Use FMO controls to set experimental gates.
- Use the gating strategy for live and single cells as shown in Figure 2B.
- Perform the gating as shown in Figure 2B for CD45, CD31, LY6C, and CD9.
- Use flow cytometry software to evaluate the frequencies of CD45– CD31– LY6C– CD9– cells (APCs) and CD45– CD31– LY6C+ cells (FIPs) within isolated fractions.
5. Gene expression analysis using quantitative PCR to assess purity of FIPs and APCs
- Extract mRNA from magnetically or FACS isolated cells using commercially available extraction kit (see Table of Materials) following the manufacturer’s instructions.
- Use 1 µg of RNA to synthetize cDNA using a cDNA Reverse Transcriptase kit (see Table of Materials) by following the manufacturer’s instructions.
- Determine relative mRNA levels of APC and FIPs-selective genes (Table 1) by quantitative PCR using SYBR green PCR master mix.
- Set up the sample reaction for PCR as follows: 5 µL of 2x SYBR green dye, 1 µL of cDNA (~50 ng/ µL), 0.5 µL of each forward and reverse primer (10 µM) and 3 µL of water.
- Use the following standard PCR conditions for the quantitative PCR run: hold stage: 50 °C for 2 min, 95°C for 10 min; PCR stage (40 cycles): 95 °C for 15 s, 60 °C for 1 min.
- Normalize values to house-keeping gene (Rps18) levels by calculating ΔΔ-Ct.
- To evaluate statistical significance, perform unpaired Student’s t-test.
6. Cell culture and differentiation
- Centrifuge magnetically- or FACS- isolated cells at 600 x g for 5 min at 4 °C.
- Resuspend the pellet in 500 µL of gonadal APC culture media and plate 40K cells/well from each fraction in a 48 well culture plate.
- Replace media every 1-2 days. APCs will begin to undergo differentiation into adipocytes as they approach confluence. FIPs maintained in the same media are resistant to undergoing adipogenesis.
Representative Results
This protocol describes two strategies that allow for the isolation of distinct stromal cell populations from intra-abdominal WAT depots of adult mice. APCs and FIPs can be isolated by FACS (Figure 1) or immunomagnetic bead separation with biotinylated antibodies (Figure 2). Both approaches utilize reagents and antibodies that are all commercially available. Immunomagnetic bead separation leads to the separation of adipogenic from non-adipogenic cells from the gWAT SVF. Flow cytometry analysis showed that 75% of cells within the adipogenic fraction represented LY6C– CD9– APCs. >75% of the non-adipogenic fraction represented FIPs (LY6C+ cells).
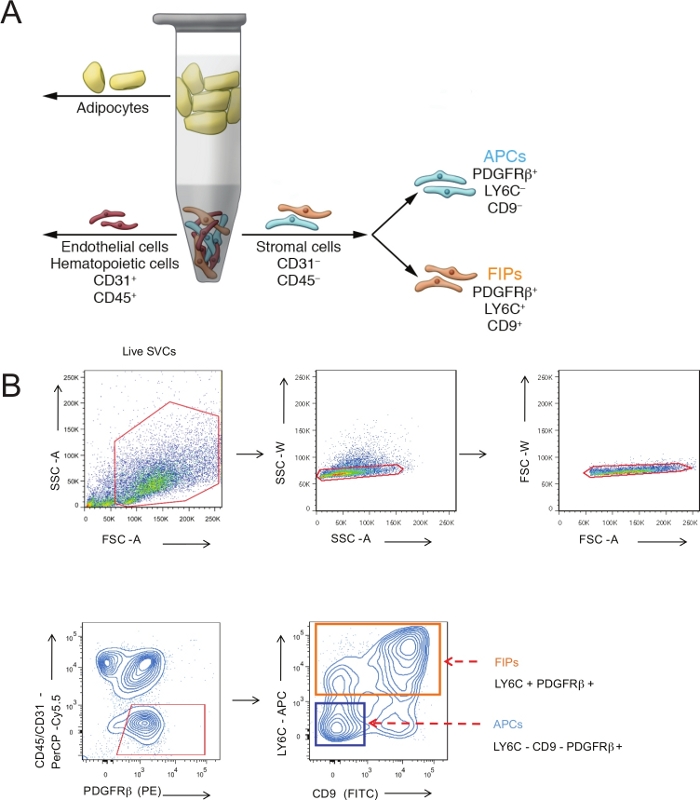
Figure 1: Isolation of PDGFR β + stromal cell subpopulations from gonadal WAT by FACS. (A) Schematic overview of the procedure: The stromal vascular fraction (non-adipocyte cells) was separated from mature adipocytes by enzymatic tissue digestion and centrifugation. Fluorescence-activated cell sorting (FACS) was then used to remove endothelial (CD31+) and hematopoietic (CD45+) lineage cells and isolate LY6C+ PDGFRβ+ cells (FIPs) and LY6C– CD9– PDGFRβ+ cells (APCs). (B) Representative FACS collection gates. Panel A is reproduced from ref.11 with permission. Please click here to view a larger version of this figure.
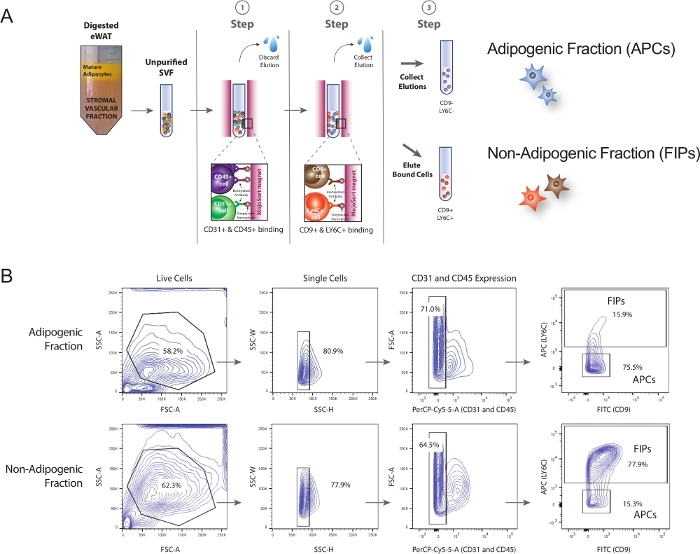
Figure 2: Separation of adipogenic and non-adipogenic stromal cells by immunomagnetic bead separation. (A) Schematic overview of the procedure: Step 1: CD31+ & CD45+ cells bind to the magnet. This removes both endothelial and hematopoietic lineage cells. The eluate containing CD31– & CD45– cells were collected and then incubated with antibodies recognizing LY6C and CD9, respectively. Step 2: CD9+ and LY6C+ cells binding to the magnet. Step 3: The supernatant (unbound fraction) containing CD9- & LY6C- cells was collected as this represented the adipogenic fraction (APCs). Non-adipogenic CD9+ and LY6C+ cells bound to nanospheres were eluted as the non-APC fraction containing FIPs. (B) Flow cytometry analysis to assess the frequency of APCs (LY6C– CD9–) and FIPs (LY6C+) within adipogenic and non-adipogenic fractions, respectively. Please click here to view a larger version of this figure.
Light microscopy and gene expression analysis demonstrate that APCs isolated by FACs or through magnetic bead separation from gWAT of 6-8 week-old mice differentiated into lipid-containing adipocytes to a high degree within 7-10 days following the initial plating of cells in Gonadal APC Culture media (Figure 3). In contrast, non-adipogenic precursors (such as fibro-inflammatory precursors, or FIPs) remained fibroblast-like and did not become adipocytes when maintained in the same culture media (Gonadal APC Culture Media) (Figure 3). It should be noted that few cells in the non-APCs cultures showed some lipid accumulation (Figure 3D). These likely arise from APC-contamination during cell isolation. Additional washes might improve the purity of this fraction.
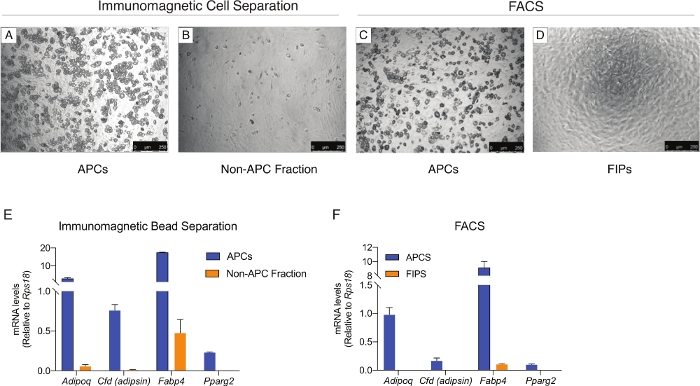
Figure 3: In vitro differentiation of PDGFR β + stromal cell populations isolated from gWAT of adult mice. (A-D) Representative bright-field images of differentiated stromal cell subpopulations isolated by immunomagnetic bead separation (A-B) or FACS (C-D) from 6-8-week-old mouse gWAT SVF. Images were taken seven days after plating cells in Gonadal APC Culture Media. Within 7-10 days of plating, APCs undergo spontaneous adipocyte differentiation. Magnification 10X. Scale = 250 µM. (E-F) mRNA levels of adipocyte-selective genes in differentiated cultures shown in A-D. Bar graphs represent mean + SEM. Please click here to view a larger version of this figure.
| FIPs | Enriched Genes (vs. APCs) | Forward Primer 5’-3’ | Reverse Primer 5’-3’ | ||
| Ly6c1 | ACTGTGCCTGCAACCTTGTCT | GGCCACAAGAAGAATGAGCAC | |||
| CD9 | GCGGGAAACACTCAAAGCCAT | AAAGCTGTTTCTTGGGGCAGG | |||
| Nov | GTTCCAAGAGCTGTGGAATGG | CTCTTGTTCACAAGGCCGAAC | |||
| Efhd1 | GGCCGCTCTAAGGTCTTCAAT | GTCAATAAAGCCGTCCCTTCC | |||
| Stmn4 | ACCTGAACTGGTGCGTCATCT | CTTGGGAGGGAGGCATTAAAC | |||
| Dact2 | AGCCCCCTAAAGGAAGAAACC | GGTCCTTGGCCACAGTCATTA | |||
| Il33 | ATTTCCCCGGCAAAGTTCAG | AACGGAGTCTCATGCAGTAGA | |||
| Ccl2 | CCACAACCACCTCAAGCACTTC | AAGGCATCACAGTCCGAGTCAC | |||
| Tgfb2 | GGTGTTGTTCCACAGGGGTTA | CGGTCCTTCAGATCCTCCTTT | |||
| Fn1 | GAGAGCACACCCGTTTTCATC | GGGTCCACATGATGGTGACTT | |||
| DPP4 | TGGTGGATGCTGGTGTGGATT | AAGGGGCCTCTCTTCTCTTCCT | |||
| Thy1 | TCTTCTTTCCCTTGCCCCTCTG | AGGTTGCAAGACTCTCGCTGT | |||
| APCs | Enriched Genes (vs. FIPs) | Forward Primer 5’-3’ | Reverse Primer 5’-3’ | ||
| Agt | GTTCTGGGCAAAACTCAGTGC | GAGGCTCTGCTGCTCATCATT | |||
| Cxcl14 | TGGACGGGTCCAAGTGTAAGT | TCCTCGCAGTGTGGGTACTTT | |||
| Mmd2 | ATCTGGGAGCTGATGACAGGA | AGTGGGTACCAGCACCAAATG | |||
| Pde11a | CGAGCTTGTCAGGAAAGGAGA | TTCAGCCACCTGTCTGGAGAT | |||
| Lrn1 | CAACATGGGAGAGCTGGTTTC | GCACACTACGGAAAGCCAAAC | |||
| Pparg | GCATGGTGCCTTCGCTGA | TGGCATCTCTGTGTCAACCATG | |||
| Fabp4 | ACTGGGCGTGGAATTCGATGA | ACCAGCTTGTCACCATCTCGT | |||
| Lpl | CATCGAGAGAGGATCCGAGTGAA | TGCTGAGTCCTTTCCCTTCTG | |||
| Cd36 | GAGTTGGCGAGAAAACCAGTG | GAGAATGCCTCCAAACACAGC | |||
Table 1: qPCR primers sequences used to validate the isolation of FIPs and APCs
Discussion
The C57BL/6 strain of mice is the most used mouse strain in studies of diet-induced obesity. C57BL/6 mice rapidly gain weight when placed on a high-fat diet (HFD) and develop some of the prominent features of metabolic syndrome associated with obesity (e.g., insulin resistance and hyperlipidemia). Notably, WAT expansion occurring in association with high-fat diet (HFD) feeding occurs in a depot-specific manner19,20,21,22,23. Expansion of the subcutaneous inguinal WAT depot (iWAT) occurs almost exclusively through adipocyte hypertrophy, whereas the expansion of the gonadal WAT (gWAT) occurs through both adipocyte hypertrophy and hyperplasia. The gWAT depot of obese mice is also a prominent site of metabolic inflammation. Thus, the gWAT depot of diet-induced obese mice represents a model to study multiple features of adipose tissue remodeling linked to obesity.
Over the past several years, the most commonly used strategies to prospectively isolate APCs from adipose depots selects cells on the basis of CD29, SCA-1, and CD34 expression (CD29+ CD34+ SCA-1+ CD31– CD45–)24,25. This approach remains useful for the selection of APCs from iWAT and other WAT depots; however, in the gonadal WAT depot and other intra-abdominal depots, CD34 and SCA-1 expression are enriched in anti-adipogenic cells rather than APCs15,26. Buffolo et al. provide direct evidence of this, demonstrating that gWAT stromal cells selected on the basis of high expression of CD34 (CD34high) are anti-adipogenic26. Therefore, the selection of cells based on the expression of CD34 and SCA-1 from this WAT depot yields a heterogeneous population that likely includes FIPs. The presence of such anti-adipogenic cells may explain the reported lack of adipogenic potential that isolated gonadal CD34+ SCA-1+ cells possess in vitro when compared to corresponding cells from the inguinal WAT depot25. The approach we describe here allows for the enrichment of intra-abdominal WAT APCs that are highly adipogenic in vitro. Moreover, APCs transplanted into lipodystrophic mice can form an ectopic fat pad15. Our strategy allows for the isolation of APCs from multiple intra-abdominal depots of both male and female mice, including gWAT, mesenteric WAT, and retroperitoneal WAT15. Multiple genetic lineage tracing studies demonstrate that adipocytes emerging in gWAT in association with HFD feeding originate from perivascular stromal cells expressing Pdgfrb (PDGFRβ protein)21,23. Importantly, the health of gWAT in obese mice is dependent on the adipogenic capacity of PDGFRβ+ cells27. These data support the notion that the gWAT APCs isolated by the approach described here are of physiological relevance.
Gonadal WAT APCs isolated by this approach differentiate rapidly into adipocytes upon reaching confluence in two-dimensional culture, or even prior to confluence. Unlike most established preadipocyte cell lines, these primary APCs do not require the addition of commonly used adipogenic factors (i.e., dexamethasone, IMBX, or PPARγ agonist). Readers should note that the commercially used ITS supplement used in this protocol does contain high levels of insulin. In addition, adipocyte differentiation can vary significantly with different sources/lots of FBS. Testing multiple lots of FBS is sometimes necessary to find serum that supports differentiation. Moreover, the varying levels of endotoxin in FBS may also influence the baseline pro-inflammatory phenotypes of APCs and FIPs.
FACS has been the commonly used technique for isolating APCs from the adipose SVF. This approach allows for the precise separation of cell populations and removal of debris and dead cells. Nevertheless, the duration and physical stress imposed on the cells may impact gene expression and/or cellular function. Moreover, multi-channel cell sorters may not be readily available to all investigators. We provide details here on how APCs can be also isolated by magnetic bead separation. From our experience, the yield of both populations through magnetic bead separation is lower than observed when using FACS. Moreover, as shown in Figure 2 above, this approach sacrifices some degree of purity. Nevertheless, magnetic bead separation yields cultures of APCs with high adipogenic potential. The purity of APC isolated through this approach can likely increase with repeated washing steps; however, this may compromise yield. A critical step in the protocol is the binding of biotinylated antibodies to target antigens on the surface of desired or undesired cells. If incubation time is insufficient or antibody concentrations are too low, target cells will remain unlabeled. Investigators may need to optimize antibody concentration for their isolations. The same principle applies to the incubation with streptavidin nanospheres. Failure to form streptavidin-biotin complexes will affect the efficiency of the isolation. Researchers should also pay additional attention to each washing step and resist the temptation to blot off any hanging droplets when collecting or discarding eluates from the magnet; blotting can result in cross-contamination from undesired cell populations. It should be of note that when performing a positive selection, the nanobeads are not removed from the cell fraction and may be detectable under a microscope. In our experience, the presence of these beads does not interfere with downstream functional assays. Investigators should note that under this magnetic-bead separation strategy, the non-APC fraction remains heterogeneous. This population contains mostly FIPs (>75% LY6C+); however, other cell types are likely present (e.g., CD9+ mesothelial cells). As such, the magnetic bead separation protocol presented here is perhaps most useful when the aim is to simply isolate APCs, and FACS machines are not readily available or cost prohibitive.
Investigators should also note important limitations to the overall sorting strategies described here. First and foremost, the protocols we describe here are currently only applicable to intra-abdominal WAT depots of mice. The subcutaneous iWAT depot in mice contains PDGFRβ+ adipose progenitors; however, LY6C expression does not readily discriminate between functionally distinct progenitor subpopulations within that depot27. Readers are referred to the work of Merrick et al. and Church et al. for protocols to isolate APCs from that depot16,25. We have not yet tested whether this sorting strategy can isolate functional APCs from rats. Moreover, it should be noted that there is no apparent ortholog for LY6C in humans28. As such, human APCs cannot be sorted based on these markers. Recent single-cell sequencing studies of human adipose stromal cells may lead to new strategies to isolate distinct progenitor populations from human tissues29. Second, there are limitations to the use of the cells in vitro. FIPs are highly proliferative and can be propagated for several passages and maintain their functional properties; however, APCs substantially lose their adipogenic potential with passage. This provides a technical challenge for those aiming to perform biochemical assays that require high cell numbers or manipulate gene expression (e.g., CRISPR/Cas9 or RNA interference). In our view, our approach is well-suited when the objective is to compare the frequency and properties of native APCs and/or FIPs derived directly from intra-abdominal WAT depots of animal models (e.g., APC frequency in control and experimental animals; comparison of male and female progenitors; effect of diet, age, etc., on progenitor frequency and properties). The ability to study these distinct cell populations in isolation should greatly aid in attempts to dissect molecular mechanisms that regulate adipogenesis and adipose tissue remodeling in mice.
Divulgazioni
The authors have nothing to disclose.
Acknowledgements
The authors are grateful to Lisa Hansen and Kirsten Vestergaard for excellent technical assistance, and P. Scherer, N. Joffin, and C. Crewe for critical reading of the manuscript. The authors thank the UTSW Flow Cytometry Core for excellent guidance and assistance in developing the protocols described here. R.K.G. is supported by NIH NIDDK R01 DK104789, NIDDK RC2 DK118620, and NIDDK R01 DK119163. J.P. is sponsored by a pre-doctoral award from Innovation Fund Denmark.
Materials
| Mechanical Tissue Preparation and SVF Isolation | |||
| 40 and 100 µm cell strainers | Fisher Scientific | 352340/352360 | |
| 1X Phosphate buffered saline (PBS) | Fisher Scientific | 21040CV | |
| 5ml polypropylene tubes | Fisher Scientific | 352053 | |
| Digestion Buffer (for 10mL) | |||
| 10 ml HBSS | Sigma | H8264 | |
| 10 mg Collagenase D (1 mg/ml final cc.) | Roche | 11088882001 | |
| 0.15 g BSA (1.5 % final cc.) | Fisher Scientific | BP1605-100 | |
| Immunomagnetic separation of APCs and non-APCs | |||
| 5X MojoSort Buffer (MS buffer) | BioLegend | 480017 | |
| 5 ml MojoSort Magnet (MS magnet) | BioLegend | 480019 | |
| 100 µL MojoSort Streptavidin Nanobeads | BioLegend | 480015 | |
| Purity Check and FACS | |||
| 10X Red Blood Cell Lysis Buffer | eBioscience | 00-4300-54 | |
| Fc block (Mouse CD16/CD32) | eBioscience | 553141 | |
| Antibodies | |||
| Biotin CD45 | BioLegend | 103103 | Concentration: ≤ 0.25 µg per 10^6 cells Species: Mouse Clone: 30-F11 |
| Biotin CD31 | BioLegend | 102503 | Concentration: ≤ 0.25 µg per 10^6 cells Species: Mouse Clone: MEC13.3 |
| Biotin CD9 | BioLegend | 124803 | Concentration: ≤ 0.25 µg per 10^6 cells Species: Mouse Clone: MZ3 |
| Biotin LY6C | BioLegend | 128003 | Concentration: ≤ 0.25 µg per 10^6 cells Species: Mouse Clone: HK1.4 |
| CD31-PerCP/Cy5.5 | BioLegend | 102419 | Concentration: Dilution 1:400 Species: Mouse Clone: 390 |
| CD45-PerCP/Cy5.5 | BioLegend | 103131 | Concentration: Dilution 1:400 Species: Mouse Clone: 30-F11 |
| CD140b PDGFRβ-PE | BioLegend | 136006 | Concentration: Dilution 1:50 Species: Mouse Clone: APB5 |
| LY6C-APC | BioLegend | 128016 | Concentration: Dilution 1:400 Species: Mouse Clone: HK1.4 |
| CD9-FITC | BioLegend | 124808 | Concentration: Dilution 1:400 Species: Mouse Clone: MZ3 |
| Cell Culture and Differentiation | |||
| Gonadal APC Culture media (for 500mL) | |||
| 288 mL DMEM with 1 g/L glucose | Corning | 10-014-CV | |
| 192 mL MCDB201 | Sigma | M6770 | |
| 10 mL Fetal bovine serum (FBS)** lot#14E024 | Sigma | 12303C | |
| 5 mL 100% ITS premix | BD Bioscience | 354352 | |
| 5 mL 10 mM L-ascorbic acid-2-2phosphate | Sigma | A8960-5G | |
| 50 µL 100 g/ml FGF-basic | R&D systems | 3139-FB-025/CF | |
| 5 mL Pen/Strep | Corning | 30-001-CI | |
| 500 µL Gentamycin | Gibco | 15750-060 | |
| **NOTE: The adipogenic capacity of primary APCs can vary from lot to lot of commercial FBS. Multiple lots/sources of FBS should be tested. |
Riferimenti
- Ouchi, N., Parker, J. L., Lugus, J. J., Walsh, K. Adipokines in inflammation and metabolic disease. Nature Reviews Immunology. 11 (2), 85-97 (2011).
- Rosen, E. D., Spiegelman, B. M. What we talk about when we talk about fat. Cell. 156 (1-2), 20-44 (2014).
- Funcke, J. B., Scherer, P. E. Beyond adiponectin and leptin: adipose tissue-derived mediators of inter-organ communication. Journal of Lipid Research. 60 (10), 1648-1684 (2019).
- Eto, H., et al. Characterization of structure and cellular components of aspirated and excised adipose tissue. Plastic and Reconstructive Surgery. 124 (4), 1087-1097 (2009).
- Hirsch, J., Batchelor, B. Adipose tissue cellularity in human obesity. Clinics in Endocrinology and Metabolism. 5 (2), 299-311 (1976).
- Ghaben, A. L., Scherer, P. E. Adipogenesis and metabolic health. Nature Reviews Molecular Cell Biology. 20 (4), 242-258 (2019).
- Hepler, C., Gupta, R. K. The expanding problem of adipose depot remodeling and postnatal adipocyte progenitor recruitment. Molecular Cell Endocrinology. 445, 95-108 (2017).
- Jo, J., et al. Hypertrophy and/or Hyperplasia: Dynamics of Adipose Tissue Growth. PLoS Computational Biology. 5 (3), 1000324 (2009).
- Sun, K., Kusminski, C. M., Scherer, P. E. Adipose tissue remodeling and obesity. Journal of Clinical Investigation. 121 (6), 2094-2101 (2011).
- Kloting, N., et al. Insulin-sensitive obesity. American Journal of Physiology-Endocrinology and Metabolism. 299 (3), 506-515 (2010).
- Vishvanath, L., Gupta, R. K. Contribution of adipogenesis to healthy adipose tissue expansion in obesity. Journal of Clinical Investigation. 129 (10), 4022-4031 (2019).
- Choe, S. S., Huh, J. Y., Hwang, I. J., Kim, J. I., Kim, J. B. Adipose Tissue Remodeling: Its Role in Energy Metabolism and Metabolic Disorders. Frontiers in Endocrinology (Lausanne). 7, 30 (2016).
- Hepler, C., Vishvanath, L., Gupta, R. K. Sorting out adipocyte precursors and their role in physiology and disease. Genes and Development. 31 (2), 127-140 (2017).
- Burl, R. B., et al. Deconstructing Adipogenesis Induced by beta3-Adrenergic Receptor Activation with Single-Cell Expression Profiling. Cell Metabolism. 28 (2), 300-309 (2018).
- Hepler, C., et al. Identification of functionally distinct fibro-inflammatory and adipogenic stromal subpopulations in visceral adipose tissue of adult mice. Elife. 7, 39636 (2018).
- Merrick, D., et al. Identification of a mesenchymal progenitor cell hierarchy in adipose tissue. Science. 364 (6438), 2501 (2019).
- Schwalie, P. C., et al. A stromal cell population that inhibits adipogenesis in mammalian fat depots. Nature. 559 (7712), 103-108 (2018).
- Bagchi, D. P., MacDougald, O. A. Identification and Dissection of Diverse Mouse Adipose Depots. Journal of Visualized Experiments. (149), e59499 (2019).
- Jeffery, E., Church, C. D., Holtrup, B., Colman, L., Rodeheffer, M. S. Rapid depot-specific activation of adipocyte precursor cells at the onset of obesity. Nature Cell Biology. 17 (4), 376-385 (2015).
- Kim, S. M., et al. Loss of white adipose hyperplastic potential is associated with enhanced susceptibility to insulin resistance. Cell Metabolism. 20 (6), 1049-1058 (2014).
- Vishvanath, L., et al. Pdgfrbeta+ Mural Preadipocytes Contribute to Adipocyte Hyperplasia Induced by High-Fat-Diet Feeding and Prolonged Cold Exposure in Adult Mice. Cell Metabolism. 23 (2), 350-359 (2016).
- Wang, Q. A., Tao, C., Gupta, R. K., Scherer, P. E. Tracking adipogenesis during white adipose tissue development, expansion and regeneration. Nature Medicine. 19 (10), 1338-1344 (2013).
- Gao, Z., Daquinag, A. C., Su, F., Snyder, B., Kolonin, M. G. PDGFRalpha/PDGFRbeta signaling balance modulates progenitor cell differentiation into white and beige adipocytes. Development. 145 (1), 155861 (2018).
- Rodeheffer, M. S., Birsoy, K., Friedman, J. M. Identification of white adipocyte progenitor cells in vivo. Cell. 135 (2), 240-249 (2008).
- Church, C. D., Berry, R., Rodeheffer, M. S. Isolation and study of adipocyte precursors. Methods Enzymol. 537, 31-46 (2014).
- Buffolo, M., et al. Identification of a Paracrine Signaling Mechanism Linking CD34(high) Progenitors to the Regulation of Visceral Fat Expansion and Remodeling. Cell Reports. 29 (2), 270-282 (2019).
- Shao, M., et al. De novo adipocyte differentiation from Pdgfrbeta(+) preadipocytes protects against pathologic visceral adipose expansion in obesity. Nature Communications. 9 (1), 890 (2018).
- Lee, P. Y., Wang, J. X., Parisini, E., Dascher, C. C., Nigrovic, P. A. Ly6 family proteins in neutrophil biology. Journal of Leukocyte Biology. 94 (4), 585-594 (2013).
- Vijay, J., et al. Single-cell analysis of human adipose tissue identifies depot and disease specific cell types. Nature Metabolism. 2 (1), 97-109 (2020).

