Methanol-Based Whole-Mount Preparation for the Investigation of Retinal Ganglion Cells
Summary
Methanol can be used as an auxiliary fixed medium for retinal whole-mount preparations and long-term storage, which is useful for the investigation of retinal ganglion cells.
Abstract
Retinal ganglion cells (RGCs), which are the projection neurons of the retina, propagate external visual information to the brain. Pathological changes in RGCs have a close relationship with numerous retinal degenerative diseases. Whole-mount retinal immunostaining is frequently used in experimental studies on RGCs to evaluate the developmental and pathological conditions of the retina. Under some circumstances, some valuable retina samples, such as those from transgenic mice, may need to be retained for a long period without affecting the morphology or number of RGCs. For credible and reproducible experimental results, using an effective preserving medium is essential. Here, we describe the effect of methanol as an auxiliary fixed medium for retinal whole-mount preparations and long-term storage. In brief, during the isolation process, cold methanol (−20 °C) is pipetted onto the surface of the retina to help fix the tissues and facilitate their permeability, and then the retinas can be stored in cold methanol (−20 °C) before being immunostained. This protocol describes the retina isolation workflow and tissue sample storage protocol, which is useful and practical for the investigation of RGCs.
Introduction
Retinal ganglion cells (RGCs) are the only projection neurons in the retina, and they integrate and transmit outside visual information to the brain1. Many neurodegenerative diseases such as glaucoma and traumatic optic neuropathy are characterized by irreversible damage and loss of RGCs2,3. Analyzing the morphological and quantitative changes of RGCs is a crucial step in determining how neurodegenerative diseases develop and advance4,5.
Indirect immunofluorescence assay is a widely accepted method to monitor the distribution of proteins and cell counting. In the laboratory, whole-mount retinal immunostaining is commonly used in experimental studies on RGCs to evaluate the physiological and pathological conditions of the retina6. The most common markers used for RGC quantification in the whole retina include Brn3a, RNA binding protein with multiple splicing (RBPMS), and so on7,8. Characterizing the amount and distribution of RGCs requires high-quality whole-mount retinal immunostaining. Generally, in immunostaining protocols, the retina is immersed in chemical fixatives before being incubated in antibodies. Ideal fixatives should not change the shape of cells, the accessibility or affinity of the epitopes for antibodies, or the linear dimensions of the tissue9,10.
Due to the complex structure of the retina, problems such as retinal fragility and folding, as well as some common difficulties including cell shrinkage and unclear nuclei, are prone to occur when making a whole-mount retinal patch, which has a negative impact on experimental research. In addition, not all retinas are immunostained immediately, especially when it comes to the retinas of transgenic mice with expensive prices that are of precious origin, necessitating the preservation of the extra retinal samples for further use.
The appropriate fixative solution can fix the tissue quickly, avoid tissue autolysis, preserve the normal morphology and structure of the tissue cells, and keep the antigenicity of proteins and other substances10. At present, formaldehyde-based fixation has been widely used in various tissues, including separated retinas, hemisected eyecups, and whole eyeballs10. Tissue shrinkage and the morphological alteration of cells are the two critical challenges encountered following immersion in formaldehyde11. In addition, modified fixation formulations are increasingly emerging to maximize the retention of the original properties of the retina and the target cells9,10. Different retinal fixation treatments may affect the retinal structure, protein immunogenicity, fluorescence excitation , and attenuation quenching cycle differently12,13. Retinas fixed with Davidson’s solution are more morphologically intact compared to those fixed with formalin, but Davidson’s solution is less compatible with some antibodies, such as microglial marker-ionized calcium binding adaptor molecule 112. Considering the fragile nature of retinas, researchers would naturally wonder whether the retinal integrity, as well as the properties and morphology of the target cells, will change after long-term storage. However, the possible effects of fixation solution on retinal and RGC cell morphology after storage for several months have rarely been reported. The optimization of retinal fixation is critical for the evaluation and preservation of RGCs.
We provide a detailed description of a reliable and technically straightforward method that we use for whole-mount murine retinal staining. Our method emphasizes the proper preparation and storage of retinas for RGC investigation, taking into account the need for the long-term storage of retinal tissue as well as specific aspects of fluorophore formation or degradation.
Protocol
All steps are performed at room temperature unless otherwise indicated. All C57BL/6J mice used were obtained from the Laboratory Animal Center of Wuhan University, and all the related experiments were approved by the Committee on the Ethics of Animal Experiments of Wuhan University. All efforts were made to minimize the suffering of the mice.
1. Enucleation and fixation of the eyes
- Euthanize the mice with carbon dioxide asphyxiation, and enucleate the eyeball gently using toothless tweezers.
- Rinse the eyeball once in phosphate-buffered saline (PBS).
- Puncture the eyeball with a syringe needle at the cornea under a microscope (eyepiece WF: 10x/22; continuous magnification objective: 0.67x-4.5x) to accelerate the fixation into the eyeball and improve the fixing efficiency.
- Transfer to a 24-well plate containing 4% paraformaldehyde (PFA).
- Fix the eyeball in 4% PFA for 45 min, and then transfer it to 1x PBS to remove excess PFA (wash three times, 5 min/time) immediately.
2. Retina isolation and flattening
- Transfer the eyeball to a glass slide, and place it under a dissecting microscope (eyepiece WF: 10x/22; continuous magnification objective: 0.67x-4.5x).
- Hold the forceps in one hand, and use it to clamp the margin of the cornea to prevent eyeball movement. Use the other hand to hold the dissecting scissors and cut around the cornea at approximately 1 mm of depth through the corneoscleral limbus. Remove the lens and vitreous body.
- Hold the optic disc at the center, and using dissecting scissors, cut the retina radially along the four quadrants, reaching approximately 2/3 of the radius of the retina.
- Clamp one of the scleral edges using toothed forceps. With the other hand, hold the edge of the sclera with untoothed forceps, and move from where the sclera is fixed by the toothed forceps toward the base of the sclera. Carefully peel the retina.
- Draw off PBS using a pipette (200 µL) to flush and wet the retina, and then remove any excess PBS with a small piece of absorbent paper. If needed, gently flatten the retina with a small bristle brush.
- Slowly pipette cold methanol (precooled in a −20°C freezer) drop by drop onto the inner surface of the retina (the volume of methanol is not fixed, as long as the retina can be completely coveredby the methanol). The retina turns white and develops increased tenacity.
- Gently flatten the retina, and remove impurities such as residual pigment membranes and the vitreous body with small bristle brushes. Invert the retina using small bristle brushes, and repeat the above-mentioned process.
- Transfer the methanol-treated retina into a well of a 24-well plate, and keep it soaked in methanol.
- Store it at −20°C for 1-2 h for immediate immunostaining, or leave the retina in methanol, and store it at −20°C for long-term storage.
- Remove the methanol from the 24-well plate, and rinse the retina with 1x PBS.
3. Immunofluorescent staining of the RGCs
- Carefully transfer the retina to a 24-well hemagglutination plate with a plastic Pasteur pipette, and block in 5% PBS-TX-BSA (5 g of bovine serum albumin powder dissolved in 100 mL of 1x PBST solution; the PBST is formed by adding 10 mL of Triton X-100 to 2,000 mL of 1 x PBS) at room temperature for 4 h or overnight at 4 °C. Keep the ganglion side up.
- Remove the PBS-TX-BSA, and incubate the retina at 4 °C for 48-96 h, adding 100 µL of the selected primary antibody (guinea pig anti-RBPMS antibody) using a 1:400 dilution.
- Remove the primary antibody, and rinse the retina three times (20 min each) with 1x PBS, shaking at room temperature.
- Incubate the retina with gentle shaking overnight at 4 °C with 100 µL of the corresponding secondary antibody (see Table of Materials), cyanine Cy3 affiniPure donkey anti-guinea pig IgG (H+L), using a 1:400 dilution.
- Rinse the retina with 1x PBS three times (20 min each).
- Lay the retina flat on the slide with the ganglion cell layer facing upward, drop an appropriate amount of anti-fluorescence quenching agent around the retina with a pipette, and cover the slide with a coverslip (be careful not to have bubbles).
NOTE: To determine the appropriate amount of anti fluorescence quencher, ensure that it covers the entire retina. After that, cover the slide without allowing the retina to float and move easily. - Seal the slide all around with a sealing agent to prevent it from moving. Store the samples at −20°C, and protect them from light.
- Image the retina using a fluorescence/confocal microscope.
Representative Results
After dissection, the retina should look like a flat four-leaf clover. In this study, by using the protocol outlined above, the retina turned white after methanol was added (Figure 1). Meanwhile, the retina changed from soft to pliable and flat. Next, the RGCs were labeled with anti-RBPMS8. Four image fields were taken in the whole-mount retina (n = 3) using a confocal microscope (eyepiece: 10x; objective: 40x). Representative views of visualized RGCs of retinas before methanol processing and after 12 months of long-term preservation in methanol, are demonstrated in Figure 2. The fluorescence intensity showed no significant changes. Methanol preservation did not affect the RGC immunostaining.
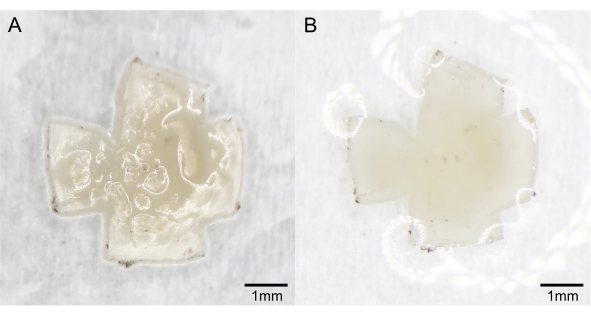
Figure 1: Retinal changes after methanol treatment. (A) Before methanol treatment. (B) After methanol treatment. Please click here to view a larger version of this figure.
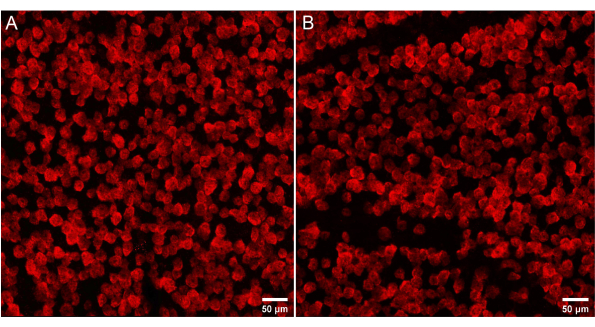
Figure 2: Effect of methanol on retinal ganglion cell (RGC) immunostaining. (A) Retina without methanol treatment. (B) Retina with 12 month storage in methanol. Please click here to view a larger version of this figure.
Discussion
Fixation is an essential step to preserve the retina, which can impact any subsequent RGC investigations based on morphology. Successful fixation rapidly captures the structure and state of the retinas at the moment of exposing them to the fixing medium, which is critical for further analysis. Although formaldehyde has been regarded as one of the most common fixing agents for tissue and cell fixation and preservation, formaldehyde alone does not always work well as the optimal chemical fixative for some investigations10,14. Different kinds of fixatives have varying capacities to precipitate amino acids and nucleotides, stabilize proteins, and maintain cell morphology15. By using mixtures of both types of fixative agents, the strengths of each can be fully utilized16,17. Methanol is frequently used in many fixation procedures before the tissue is freshly frozen or embedded in ideal cutting materials16,18. For whole-mount experiments, 100% cold (−20 °C) methanol is used to achieve retinal sample fixation, which aids the sample permeabilization for the subsequent fluorescence-based imaging19.
A key advantage of methanol fixation is that it allows for easy preservation. In this protocol, methanol is added to the front and back of the retina progressively at −20 °C after the retina has been flattened. It can be easily observed that the color of the retina rapidly changes from translucent to milky white, and the impurities become clearer. It should be noted that the retina should be gently flattened with a brush to prevent curling around it during the methanol-dripping process. After the methanol treatment, the overall toughness of the retina increases, reducing the difficulty of removing the impurities and transferring the retina. Post-fixation with methanol is more convenient for preserving retinas that have been slightly pre-fixed with PFA. However, when the tenacity of the retina is improved, the tenacity of the vitreous and other impurities is also likely to increase accordingly. One can try to gently remove some impurities that are easy to remove before using methanol, and then removing the remaining impurities after drip-adding methanol, which is more easier to perform. The early removal of impurities requires enough practice and experience. It is recommended to gently brush the remaining vitreous body on the retina radially outward from the optic disc.
In this protocol, after the treatment, the retina is soaked in methanol and placed in a −20°C freezer for some time before the subsequent sealing, and other treatments could further increase the toughness of the retina. However, it is difficult to state a precise length of time that would be universally optimal for immersion fixation. If needed, the retina could be stored in cold methanol for long periods.
In this work, with the presented methodology, the impact of storage in methanol on RGC staining – a crucial technique in retinal qualitative and quantitative evaluations – was examined. with the use of methanol, the fluorescence intensity of the RGCs, which would affect the outcomes of qualitative and quantitative testing, were not altered during immunostaining. The retinas could be kept indefinitely in a preserving solution, cold (−20°C) methanol, for at least 12 months before staining. In addition, our previous study revealed no significant difference in RGC survival rate in the optic nerve crush mouse model following long-term storage in methanol, and methanol preservation also had little impact on the quantitative analysis of the retinal vasculature and retinal hypoxia in the oxygen-induced retinopathy model20. We recommend using 4% PFA and cold (−20°C) methanol sequentially for sample preparation, as well as adopting methanol fixation for storage strategies in the laboratory. One limitation is that the analyses do not fully demonstrate subtle morphological changes at the dendrite or axonal level, though the density of the RGCs and the morphology of the soma do not seem to change21,22. It should be noted that, in this protocol, we only tested RBPMS for RGCs. Further verifying different RGC proteins (e.g., Brn3a, neuronal nuclei, neurofilament-L) would provide a more robust result. Moreover, the protocol also has the potential to be applied to any other cell type in the retina that needs further research. However, long-term inhalation or direct cutaneous exposure to methanol may cause toxic effects on the human body. Therefore, it is necessary to take good precautions in the process of using methanol.
Our method places a strong emphasis on using methanol fixation for the storage of retinas for RGC investigations and highlights important considerations regarding the RGC quantification, and fluorescence intensity. This protocol provides a straightforward and practical method to satisfy the necessity of preserving retinal samples for further use.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This work was funded by the Hubei Key Laboratories Opening Project (grant no. 2021KFY055), Natural Science Foundation of Hubei Province (grant no. 2020CFB240), and Fundamental Research Funds for the Central Universities (grant no. 2042020kf0065).
Materials
| 24-well cell culture cluster | Costar | Eyeball fixation | |
| 24-well hemagglutination plate | Labedit Company | Incubation antibody | |
| Adhesion microscope slides | Citotest | Or similar | |
| Anti-fluorescent quenching mountant | Servicebio | G1401 | Slow down fluorescence quenching |
| BSA (bovine serum albumin) | Servicebio | GC305010 | Blocking reagent |
| Confocal microscope | OLYMPUS | Apply 40x objective lens | |
| Curved scissors | Jiangsu Kanghua Medical Equipment Co., Ltd. | Dissecting tools | |
| Dissecting microscope | RWD Life science Co.,LTD | 77001S | Dissecting tools |
| Forceps | Jiangsu Kanghua Medical Equipment Co., Ltd. | Dissecting tools | |
| Methanol | Sinopharm Chemical Reagent Co., Ltd. | 20210624 | GC≥99.5% |
| Nail polish | SecheVite | Sealing agent | |
| Needles | Shanghai Kindly Enterprises Development Group Co., Ltd. | Accelerate the fixation | |
| Paraformaldehyde solution | Servicebio | G1101 | Eyeball fixation |
| PBS (phosphate buffered saline pH 7.4) | Servicebio | G0002 | Rinse the eyeball |
| Primary antibody: guinea pig anti-RNA-binding protein with multiple splicing (RBPMS) | PhosphoSolutions | Cat. #1832-RBPMS | For immunofluorescence. Used at 1:400 |
| Secondary antibody: Cy3 affiniPure donkey anti-guinea pig IgG (H+L) | Jackson ImmunoResearch | 706-165-148 | For immunofluorescence. Used at 1:400 |
| Straight scissors | Jiangsu Kanghua Medical Equipment Co., Ltd. | Dissecting tools |
References
- Sanes, J. R., Masland, R. H. The types of retinal ganglion cells: Current status and implications for neuronal classification. Annual Review of Neuroscience. 38, 221-246 (2015).
- Almasieh, M., Wilson, A. M., Morquette, B., Cueva Vargas, J. L., Di Polo, A. The molecular basis of retinal ganglion cell death in glaucoma. Progress in Retinal and Eye Research. 31 (2), 152-181 (2012).
- Au, N. P. B., Ma, C. H. E. Neuroinflammation, microglia and implications for retinal ganglion cell survival and axon regeneration in traumatic optic neuropathy. Frontiers in Immunology. 13, 860070 (2022).
- Pavlidis, M., Stupp, T., Naskar, R., Cengiz, C., Thanos, S. Retinal ganglion cells resistant to advanced glaucoma: A postmortem study of human retinas with the carbocyanine dye DiI. Investigative Ophthalmology & Visual Science. 44 (12), 5196-5205 (2003).
- Vidal-Sanz, M., et al. Understanding glaucomatous damage: anatomical and functional data from ocular hypertensive rodent retinas. Progress in Retinal and Eye Research. 31 (1), 1-27 (2012).
- Kole, C., et al. Activating transcription factor 3 (ATF3) protects retinal ganglion cells and promotes functional preservation after optic nerve crush. Investigative Ophthalmology & Visual Science. 61 (2), 31 (2020).
- Nadal-Nicolás, F. M., et al. Brn3a as a marker of retinal ganglion cells: qualitative and quantitative time course studies in naive and optic nerve-injured retinas. Investigative Ophthalmology & Visual Science. 50 (8), 3860-3868 (2009).
- Kwong, J. M., Caprioli, J., Piri, N. RNA binding protein with multiple splicing: A new marker for retinal ganglion cells. Investigative Ophthalmology & Visual Science. 51 (2), 1052-1058 (2010).
- Stradleigh, T. W., Ishida, A. T. Fixation strategies for retinal immunohistochemistry. Progress in Retinal and Eye Research. 48, 181-202 (2015).
- Stradleigh, T. W., Greenberg, K. P., Partida, G. J., Pham, A., Ishida, A. T. Moniliform deformation of retinal ganglion cells by formaldehyde-based fixatives. Journal of Comparative Neurology. 523 (4), 545-564 (2015).
- Bucher, D., Scholz, M., Stetter, M., Obermayer, K., Pflüger, H. J. Correction methods for three-dimensional reconstructions from confocal images: I. Tissue shrinking and axial scaling. Journal of Neuroscience Methods. 100 (1-2), 135-143 (2000).
- Chidlow, G., Daymon, M., Wood, J. P., Casson, R. J. Localization of a wide-ranging panel of antigens in the rat retina by immunohistochemistry: Comparison of Davidson’s solution and formalin as fixatives. Journal of Histochemistry & Cytochemistry. 59 (10), 884-898 (2011).
- Tokuda, K., et al. Optimization of fixative solution for retinal morphology: A comparison with Davidson’s fixative and other fixation solutions. Japanese Journal of Ophthalmology. 62 (4), 481-490 (2018).
- Miki, M., Ohishi, N., Nakamura, E., Furumi, A., Mizuhashi, F. Improved fixation of the whole bodies of fish by a double-fixation method with formalin solution and Bouin’s fluid or Davidson’s fluid. Journal of Toxicologic Pathology. 31 (3), 201-206 (2018).
- Zanini, C., Gerbaudo, E., Ercole, E., Vendramin, A., Forni, M. Evaluation of two commercial and three home-made fixatives for the substitution of formalin: A formaldehyde-free laboratory is possible. Environmental Health. 11, 59 (2012).
- Tang, M., et al. An optimized method to visualize the goblet cell-associated antigen passages and identify goblet cells in the intestine, conjunctiva, and airway. Immunobiology. 227 (6), 152260 (2022).
- Brock, R., Hamelers, I. H., Jovin, T. M. Comparison of fixation protocols for adherent cultured cells applied to a GFP fusion protein of the epidermal growth factor receptor. Cytometry. 35 (4), 353-362 (1999).
- Baykal, B., Korkmaz, C., Kocabiyik, N., Ceylan, O. M. The influence of post-fixation on visualising vimentin in the retina using immunofluorescence method. Folia Morphologica. 77 (2), 246-252 (2018).
- Powner, M. B., et al. Visualization of gene expression in whole mouse retina by in situ hybridization. Nature Protocols. 7 (6), 1086-1096 (2012).
- Zhang, N., Cao, W., He, X., Xing, Y., Yang, N. Using methanol to preserve retinas for immunostaining. Clinical and Experimental Ophthalmology. 50 (3), 325-333 (2022).
- Kalesnykas, G., et al. Retinal ganglion cell morphology after optic nerve crush and experimental glaucoma. Investigative Ophthalmology & Visual Science. 53 (7), 3847-3857 (2012).
- Parrilla-Reverter, G., et al. Time-course of the retinal nerve fibre layer degeneration after complete intra-orbital optic nerve transection or crush: a comparative study. Vision Research. 49 (23), 2808-2825 (2009).

