Air-Inflation of Murine Lungs with Vascular Perfusion-Fixation
Summary
Presented is a method for air-inflation with vascular perfusion-fixation of the lungs that preserves the location of cells within airways, alveoli and interstitium for structure-function analyses. Constant airway pressure is maintained with an air-inflation chamber while fixative is perfused via the right ventricle. Lungs are processed for histologic studies.
Abstract
Lung histology is often used to investigate the contributions provided by airspace cells during lung homeostasis and disease pathogenesis. However, commonly used instillation-based fixation methods can displace airspace cells and mucus into terminal airways and can alter tissue morphology. In comparison, vascular perfusion-fixation techniques are superior at preserving the location and morphology of cells within airspaces and the mucosal lining. However, if positive airway pressure is not simultaneously applied, regions of the lungs may collapse and capillaries may bulge into the alveolar spaces, leading to distortion of the lung anatomy. Herein, we describe an inexpensive method for air-inflation during vascular perfusion-fixation to preserve the morphology and location of airway and alveolar cells and interstitium in murine lungs for downstream histologic studies. Constant air pressure is delivered to the lungs via the trachea from a sealed, air-filled chamber that maintains pressure via an adjustable liquid column while fixative is perfused through the right ventricle.
Introduction
Lung histology represents the gold standard for assessing lung architecture during health and disease and is one of the most commonly used tools by pulmonary researchers1. One of the most critical aspects of this technique is the proper isolation and preservation of lung tissue, since variability in this step can lead to poor tissue quality and erroneous results1,2,3. In living animals, lung volume is determined by the balance between inward elastic recoil of the lung and outward forces transmitted from the chest wall and diaphragm by surface tension. Accordingly, when the thorax is entered, outward forces are lost and the lung collapses. Histologic sections prepared from collapsed lungs have a crowded appearance and boundaries between anatomic compartments (i.e., airspaces, vasculature, and interstitium) can be difficult to distinguish. To circumvent this challenge, researchers often inflate the lungs during chemical fixation so that airspace size and architecture is maintained.
Lungs can be inflated with air or liquid. The pressure necessary to inflate the lungs to the same volume differs between air- and liquid-inflation due to intermolecular forces at the air-liquid interface. Higher pressure (e.g., 25 cmH2O) is required during air-inflation than liquid inflation (e.g., 12 cmH2O) to overcome surface tension and open the collapsed alveoli4. Once alveoli have been recruited, a lower pressure can keep the alveoli open to the same volume as the pressure-volume curve plateaus, and pressures equalize throughout the lung according to Pascal's law4,5,6,7,8.
Two main methods of lung inflation and fixation exist to preserve murine lungs for histology. Most commonly, the airspaces are instilled with liquid – often containing a fixative. The main advantage of this approach is that it is relatively easy and requires little training. While intratracheal instillation of fixative may be preferred in studies that focus on the vasculature, liquid that is instilled via the trachea tends to push proximal airway cells and mucins into more distal airspace regions while air inflation does not1,3,4,9,10,11. Moreover, inadvertent detachment of leukocytes from the epithelium during liquid inflation alters their morphology, artifactually giving them a simple, rounded appearance4,10,11,12. Finally, inflation of the lungs with liquid can unintentionally compress the interstitium4,10,11. Together, these factors can distort the normal anatomy and cellular distributions within the preserved lungs, thus limiting the technique.
An alternative method of tissue preservation is vascular perfusion-fixation. In this method, fixative is perfused into the pulmonary vasculature via the vena cava or the right ventricle. This method preserves the location and morphology of cells in the airspace lumen. However, unless the lungs are inflated during perfusion-fixation, the lung tissue is likely to collapse.
Air-inflation with vascular perfusion-fixation harnesses strengths from each of the above fixation techniques. Herein we provide a protocol for this technique. The materials and equipment that are required are relatively inexpensive and can be easily obtained and assembled. The completed setup, shown in Figure 1A, provides constant airway pressure to the lungs by way of an adjustable, fluid-filled column while a peristaltic pump delivers fixative via the right ventricle. Lungs with preserved morphology can then be further processed for structure-function analyses.
Protocol
All methods described in this protocol have been approved by the Institutional Animal Care and Use Committee (IACUC) of National Jewish Health.
NOTE: The protocol is organized into three components. The first component details the construction of the air-inflation with perfusion/fixation equipment. A second section describes how to set up the equipment for an experiment. The final section describes how to prepare the animal and perform the experiment.
1. Construction of the water column apparatus (Figure 1B)
- Remove the plunger from a 60 mL slip tip syringe.
- Attach tape around the syringe at the 30 mL mark. Set the height of the syringe to this mark for the initial inflation pressure of 25 cmH2O. This is also where the water level in the column should be throughout the entire procedure. Label the tape either as "25 cm" (as depicted in Figure 1A) or "inflation".
NOTE: An inflation pressure of 25 cmH2O is used to ensure recruitment of collapsed airspaces. Once alveoli have been recruited, the pressure is lowered to 20 cmH2O to ensure that the airspaces are not distended. - Measure 5 cm from the tape towards the plunger end and attach another piece of tape to the syringe. Move the syringe down to this mark to lower the inflation pressure to 20 cmH2O during fixation. Label the tape either as "20 cm" (as depicted in Figure 1A) or "fixation".
- Attach 180 polyvinyl chloride (PVC) tubing to the slip tip end of the syringe. The length of tubing is dependent upon the distance between the syringe and air inflation chamber (approximately 25-30 cm).
- Place a male Luer (2) thread style tee (1.219 inches length, 0.904 inches height, 0.0904 inches inner diameter) into the other end of the tubing. This male Luer will connect to the stopcock of the air-inflation chamber (Step 2.4).
2. Construction of the air-inflation chamber (Figure 1C)
- Drill two holes (approximately 4 mm in diameter) in a 500 mL plastic container with a screw-on cap. The holes should be the same size as the female Luers (1.224 inches length, 0.312 inches height, 0.098 inches inner diameter).
NOTE: Empty media or buffer containers can be utilized for the air-inflation chamber. - Coat threads of female Luers with silicone gasket maker and place the smaller side into the pre-drilled holes of the container.
- Add silicone gasket maker around the female Luers where they enter the container to ensure an air-tight seal.
- Screw on a one-way stopcock on the lower female Luer on the air-inflation chamber.
- Cut tubing to the length of roughly 25 cm and attach male Luers to the free ends of the tubing. Connect the male Luer on one end of the tubing to the free female Luer on the air-inflation chamber. The other male Luer will connect to the animal-processing container.
3. Construction of the animal-processing container (Figure 1D)
- Drill a hole (approximately 4 mm diameter) in the side of a large plastic container. The hole should be the diameter of the female Luer. The plastic container is needed to catch excess fixation solution.
NOTE: A 30 cm x 22 cm, 3.8 L plastic storage container was used. - Coat threads of a female Luer with a silicone gasket maker and place the smaller side into the predrilled hole of the container.
- Add silicone gasket maker around the female Luer where it enters and exits the container to ensure an air-tight seal.
- Screw a one-way stopcock onto the female Luer. Tubing from the air-inflation chamber will attach to this stopcock.
4. Preparation of solutions
- Heparin solution
- Fill a container with calcium-free PBS and heparin (20 U/mL). Prepare a total of 10 mL heparin solution for each mouse. Heparin is an anti-coagulant that prevents blood clots from forming in the vessels during perfusion-fixation. Heparin solution will be used to flush blood from the lungs prior to perfusion-fixation.
- Fixative solution
CAUTION: Fixatives can present a health hazard and should be used in a chemical fume hood. All apparatuses are set up in a chemical fume hood to prevent inhalation of fixatives.- Fill a container with calcium-free PBS and paraformaldehyde (4% final concentration). Prepare a total of 50 mL fixative solution for each mouse.
NOTE: The type of fixative used may vary and will depend upon downstream histologic studies.
- Fill a container with calcium-free PBS and paraformaldehyde (4% final concentration). Prepare a total of 50 mL fixative solution for each mouse.
5. Preparation of perfusion apparatus
NOTE: A peristaltic pump is suggested for delivery of fluids into vasculature to ensure constant flow rate. The following directions are for setting up the peristaltic pump and may be different for each model. Alternatively, if a peristaltic pump is unavailable, a second water column apparatus may be constructed to perfuse fluids from a height of 35 cm H2O.
- First place the tubing around the roller assembly.
- Secure the tubing into the notched posts.
- Latch the levers into place by first placing the left lever around the tubing and securing it in place with the top and then the right lever.
- Place the proximal end of the tubing into the heparin solution and the distal end into the animal processing container.
- Preload heparin solution into the tubing by running the pump to expel air from the tubing.
- Secure a 25G x 5/8" needle onto the end of the left side of the tubing.
6. Preparation of air-inflation apparatus
- Place the syringe for the water column into a ring holder.
- Measure a vertical height of 25 cm from the animal platform to the "25 cm" tape mark (Step 1.2) on the water column.
- Attach the end of the water column's tube to the stopcock on the air chamber.
- Attach a tube from the female Luer of the air chamber to the stopcock on the animal processing container.
NOTE: If the air-inflation chamber is constructed as depicted in Figure 1C, attaching tubing in reverse order may cause water to leak into the tubing that connects to the tracheal cannula. - Ensure that the cap to the air chamber is tightly closed.
- Ensure that the stopcock on the outside of the animal processing container is closed and the stopcock on the tubing leading from the water column to the air-inflation chamber is open.
- Fill the syringe with water to the "25 cm" mark. Water will leave the syringe through the tubing into the air chamber. Once pressure is equalized water will stop flowing.
- It is possible that water will slowly leak into the air-inflation chamber as ambient air pressure within the chemical hood fluctuates. Keep an eye on the water level within the syringe and add more if necessary. Maintain the water level at the "25 cm" mark throughout the procedure.
NOTE: Usually water levels will stay consistent for the first part of air inflation at 25 cmH2O; however more water will likely need to be added to the syringe during fixation. If the water does not stop flowing, it is likely that an air leak exists within the air-inflation chamber. More silicone gasket maker may need to be applied around the Luers to prevent air leaks.
- It is possible that water will slowly leak into the air-inflation chamber as ambient air pressure within the chemical hood fluctuates. Keep an eye on the water level within the syringe and add more if necessary. Maintain the water level at the "25 cm" mark throughout the procedure.
7. Preparation of animals (Figure 2)
NOTE: This procedure has been modified from Gage et al13. We have completed this procedure on adult male and female mice of varying ages and note no age or sex bias.
- Euthanize the animal with sodium pentobarbital (150 mg/kg, intraperitoneally.). Ensure that the animal is dead prior to beginning dissection.
NOTE: While this procedure is performed on euthanized animals, this procedure can be performed on live animals to utilize the heart to pump perfusates throughout the animal. - Make two lateral incisions through the abdominal wall. Make the first incision below the rib cage and the second above the hips. Cut along the midline from the inferior incision towards the superior incision.
- Using blunt scissors, carefully make an incision into the lateral side of the diaphragm. The lungs should collapse as soon as the diaphragm is punctured.
NOTE: Care must be taken to avoid puncturing the lungs. A punctured lung is less likely to inflate during later steps. - Cut transversely along the diaphragm to open the thoracic cavity.
- Cut superiorly along the sternum from the xiphoid process to the jugular notch and laterally above the rib cage to fully expose the heart and lungs. Pin down the sides of the ribcage.
- Make a midline incision in the neck above the trachea. Remove skin, muscle, thyroid gland and connective tissue surrounding the trachea.
- Using curved forceps, slide two pieces of thread or suture under the posterior trachea. Use one piece of suture to hold the inflation Luer-stub adapter in place, and use the other ultimately to tie off the trachea at the conclusion of air-inflation and vascular perfusion-fixation.
- Poke a small hole in the trachea using an 18G x 1" needle or Vannas spring scissors.
- Place a 20G Luer-stub adapter into this hole in the trachea.
- Tie one thread around the trachea immediately distal to where the Luer-stub adapter enters to hold it in place.
- Transfer the animal to the animal processing container.
- Attach the Luer-stub adapter to the female Luer on the inside of the animal processing container.
8. Air inflation, perfusion and fixation of the lungs (Figure 2)
- Place the 25G x 5/8" needle attached to the perfusion apparatus tubing into the right ventricle of the heart.
- Cut the abdominal aorta to allow blood to drain from the heart and to promote flow of perfusate through the lungs.
- Open the stopcock on the outside of the animal processing container to inflate the lungs.
NOTE: It may take time for the lungs to fully inflate. Watch the water level in the syringe, it should not decrease rapidly unless there is a leak in the lungs. - Inflate the lungs at 25 cmH2O for 5 minutes. Inflation at 25 cmH2O preconditions the lung and assists in recruiting atelectatic lung regions.
NOTE: A small amount of water may need to be added to the syringe to maintain the 25 cm height. Inflammation and/or experimentally induced lung injury may influence inflation of the lungs. In this case, it may be necessary to increase the inflation pressure up to a maximum of 35 cmH2O to assist in recruiting atelectatic regions. - During the last minute of the lung inflation, turn on the peristaltic pump to a flow rate of 10 mL/min. Heparin solution should flow from the bottle through the tubing into the animal.
- The goal of heparin infusion is to prevent formation of thrombi in the vessels. Accordingly, infuse heparin until the lungs become white and are devoid of blood. If the lungs do not turn white, adjustment of the right ventricular needle may be necessary.
- After inflating for 5 minutes, turn off the peristaltic pump and switch the perfusion tubing from the heparin solution to the fixative.
- Lower the water column syringe to the "20 cm" mark (Step 1.3). It is normal for air bubbles to move within the water column as the pressure changes from 25 to 20 cmH2O.
- Check the water level in the syringe. It should be at the "25 cm" mark. It may be necessary to add more at this time.
- Wait for 1 min to allow the lungs to deflate from 25 to 20 cmH2O.
- Restart the perfusion pump at a flow rate of 6.5 mL/min.
- Vascular perfusion-fix for 10 – 15 minutes.
9. Extraction of lungs (Figure 3)
- Tightly tie the second piece of thread around the trachea distal to the Luer-stub adapter. Remove the Luer-stub adapter from the trachea.
- Remove the needle from the heart.
- Free the lungs and heart from the thoracic cavity by cutting the connective tissue posterior to the mediastinum with blunt scissors. Take care to avoid puncturing the lungs.
- Carefully remove the heart from the lungs.
- Place the lungs in fixative overnight.
NOTE: Duration of fixative varies depends on downstream histologic studies.- Place the lungs into a 50 mL conical tube containing 20-25 mL of fixative. Place the thread securing the trachea through the opening of the conical tube and secure by the threads of the cap. Invert the conical tube to ensure that the buoyant, air-inflated lungs remain fully submerged in fixative otherwise they will float to the top of the liquid.
- Process the lungs for histologic studies.
Representative Results
In an intact thorax, the lungs are held open by outward forces applied by the chest wall via the pleural space6,14. When the diaphragm is entered during dissection, the integrity of the pleural space is abolished and the lungs should collapse (Figure 2A, 2B). To re-expand the lungs, air inflation is performed. As a first step, 25 cm of water pressure is applied to ensure recruitment of collapsed airspaces. Accordingly, when the stopcock outside the animal holding container is opened, air will enter the lungs via the trachea and inflation should be easily observed (Figure 2C). Once the lungs are fully expanded, the inflation pressure is decreased to 20 cm water pressure (Figure 2D). The 20 cm of water pressure is chosen because it maintains complete inflation of the lungs but does not over-distend the airspaces.
The lungs should remain inflated after tracheal ligation (Figure 3A) and after removal from the thorax (Figure 3B). Deflation of lungs (Figure 3C) can occur if lungs are punctured during animal preparation or extraction. Adding fixative to the pleural surface may help seal minor leaks during the procedure; however, fixative should be applied cautiously as excess may adhere lungs to the thoracic cavity. Any leaks that are not sealed during fixation will result in collapsed lungs upon removal from the air-inflation apparatuses. Deflation of the lungs may also occur if the trachea is not completely tied off. When submerged in fixative, properly inflated lungs will have greater buoyancy than deflated lungs.
Inflated lungs can then be processed for histological analyses according to established protocols1,15. For Figure 4, lungs were processed for frozen sectioning and stained with a commercial manual staining system. Very few immune cells are present in the airway lumens of tissue fixed using traditional liquid-based inflation (Figure 4A). In contrast, inflammatory cells are preserved throughout airspaces in tissue fixed via vascular perfusion with air-inflation (Figure 4B).
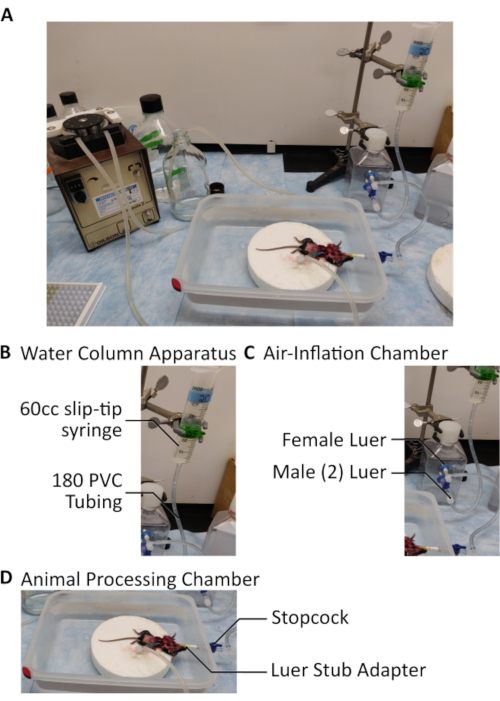
Figure 1: Assembly of apparatuses. A. Full assembly of all apparatuses. B. The water column consists of a 60 mL syringe connected to the air-inflation chamber via 180 PVC tubing and a two-way male Luer. C. A 500 mL sealed plastic container was used to construct the air-inflation chamber. The water column's male Luer connects to a stopcock connected to a female Luer within the walls of the chamber. An additional female Luer connects tubing from the air-inflation chamber to the animal processing container. Both female Luers are coated in silicone gasket maker to ensure an air-tight seal. Two male Luers are connected to both ends of tubing which connects the air-inflation chamber to the animal-processing container. D. Animals are attached to the air-inflation chamber through a 20G Luer stub adapter placed through a hole into the trachea. The Luer stub adapter is connected to a female Luer within the walls of the animal processing container. Please click here to view a larger version of this figure.
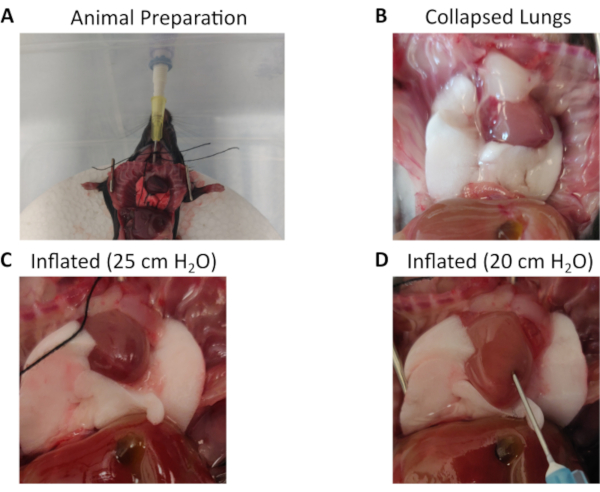
Figure 2: Animal preparation, connection to the air-inflation chamber, and inflation of lungs. A. After euthanasia, the animal's peritoneal and thoracic cavities are exposed. The rib cage is removed or pinned down to allow expansion of the lungs upon inflation. A Luer stub adapter is inserted into a small hole cut into the trachea and secured with thread or suture. The Luer stub adapter is connected to a female Luer within the wall of the animal processing chamber. The other end of the female Luer is attached to a stopcock to control air flow from the air-inflation chamber (not shown). B. Collapsed lungs before air inflation. C. Lungs are inflated to 25 cm water pressure to recruit atelectasic regions. D. When the pressure is changed to the intended fixation pressure (20 cm water), the lungs deflate slightly. Also depicted is placement of a 25G x 5/8 needle into the right ventricle for vascular perfusion-fixation of the lung. All images are photographs at 15.9 megapixel resolution and at 4:3 aspect ratio. Please click here to view a larger version of this figure.

Figure 3: Extraction of lungs following completion of air-inflation with vascular perfusion fixation. A. The trachea is tied off distal to the Luer stub adapter and lungs are extracted by cutting the connective tissue posterior to the mediastinum. B. Air-inflated lungs after successful procedural completion. C. Example of poorly inflated lungs that resulted from an air leak that occurred within the air-inflation chamber. Note these lungs are smaller than the successfully inflated lungs. All images are photographs at 15.9 megapixel resolution and at 4:3 aspect ratio. Please click here to view a larger version of this figure.
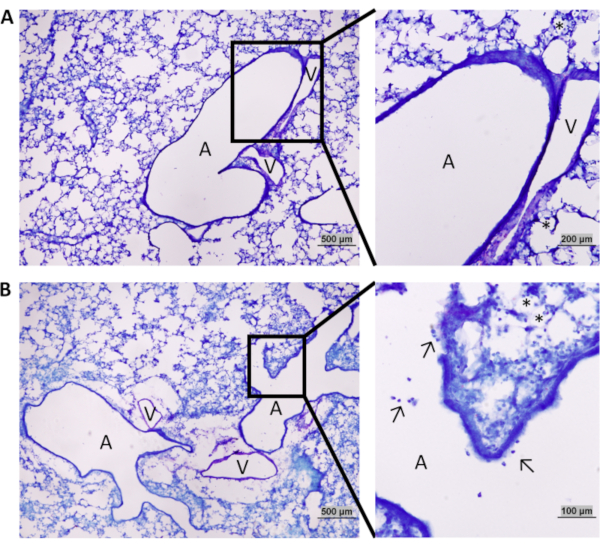
Figure 4: Comparison of lung tissue obtained by intratracheal-based fixation versus air-inflation with vascular perfusion-fixation. A. Lungs preserved by intratracheal-based fixation. B. Lungs preserved by air-inflation with vascular perfusion-fixation. B (inset). Arrows show leukocytes in the airways of a lung fixed by vascular perfusion-fixation; stars highlight leukocytes in the alveoli. In comparison, leukocytes are notably absent in the airways of lungs fixed via the intratracheal route (A inset) and intra-alveolar leukocytes are displaced, appearing to be in tight contact with epithelial cells. Abbreviations: A– airway, V– vessel. Magnification of images are 40x with 100x and 200x for A and B insets respectively. Please click here to view a larger version of this figure.
Discussion
Although commonly used, intratracheal-based fixation methods displace leukocytes from the airways and can alter normal lung architecture. The method of air-inflation with vascular perfusion-fixation that is provided in this protocol overcomes these pitfalls and more accurately preserves lung anatomy. The keys to obtaining high-quality tissue from the vascular perfusion-fixation method include careful monitoring of air-inflation pressures, avoidance of air leaks, and ensuring adequate perfusion of fixative into the vasculature.
One limitation to this procedure is that when the integrity of the thorax is interrupted, the lungs collapse and re-inflation of the lungs after collapse is necessary for accurate histological assessment. An alternative to the protocol that would maintain lung inflation without collapse would be the use of a small animal ventilator. However, such equipment is often expensive, and the protocol here offers an inexpensive solution. In healthy lungs, surfactant produced by alveolar epithelial cells helps to reduce surface tension, and in most cases lungs can be easily re-expanded. However, in diseased lungs, tissues can be stiffer and lung surfactant function can be altered, promoting lung collapse. To mitigate this effect, collapsed areas can be “recruited” using slightly higher air inflation pressures (i.e., 25 cmH2O)5. The pressure can then be reduced to allow slight deflation of the lungs to physiologic size. In our hands, an inflation pressure of 20 cm water works well. Pressures higher than this can over-distend the alveoli and impair vascular perfusion. Conversely, low pressures result in airspace collapse. Along similar lines, vascular perfusion pressures must also be titrated. Excessive perfusion pressures may distend capillaries into the alveolar space or even damage the capillaries and cause lung edema4. On the other hand, if vascular perfusion pressures are too low, perfusion may be inadequate. We have found that flow rates of 10 mL/min for the heparin solution and 6.5 mL/min for the fixative solution achieve an optimal result.
Checking the air inflation chamber for leaks is imperative to ensure constant inflation pressure during vascular perfusion-fixation. Once water is added to the syringe it should flow into the bottom of the air inflation chamber until pressures equalize. A small amount of additional water may need to be added to the syringe to maintain a column height of 25 cm for inflation and 20 cm for fixation. Silicone sealant may need to be replaced if flow into the air inflation chamber does not cease.
Another cause of air leakage is damage to the lungs. This most commonly occurs during opening of the thoracic cavity or during extraction of the lungs from the thorax. Thus, practice and great care must be taken to avoid damaging the lung during mouse preparation. A less common cause is lung pathology that results from severe lung disease. Clues to air leaks from the lungs include slow emptying from the fluid column in the syringe, a hissing sound or bubbles coming from the lung surface. Applying a small amount of fixative to the lungs at the site of the leak can help seal small leaks; however certain fixative can cause adherence of the lungs to the thoracic cavity and when lung damage is extensive, the lungs may still collapse once air pressure is removed.
Once any sources of air leakage have been assessed and managed, lungs should inflate and remain inflated during fixation. The trachea should be ligated below the cannula before removal from the inflation apparatus to prevent collapse. Lungs can then be processed for histologic studies. Air-inflation with vascular perfusion-fixation of lungs aims to preserve numbers, morphology and location of airway cells while adequately preserving global lung architecture for histologic structure-function studies.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This work was funded by the National Heart, Lung, and Blood Institute (NHLBI) grants HL140039 and HL130938. The authors would like to thank Shannon Hott and Jazalle McClendon for their technical expertise.
Materials
| 00117XF-Stopcock 1 way 100/PK M Luer | Cole-Parmer | Mfr # VPB1000050N – Item # EW-00117-XF | Stopcock |
| BD 60 mL syringe, slip tip | BD | 309654 | Syringe used to construct the water column |
| BD PrecisionGlide Needle 25G x 5/8 | BD Biosciences | 305122 | Needle for vascular perfusion/fixation |
| Female Luer Thread Style Panel Mount 1/4-28 UNF to Male Luer | Nordson Medical | FTLLBMLRL-1 | Female Luer |
| Heparin sodium salt from porcine intestinal mucosa | Sigma-Aldrich | H3393 | Heparin solution. |
| Luer-Stub Adapter BD Intramedic 20 Gauge | BD Biosciences | 427564 | Luer-Stub Adapter |
| Male Luer (2) to Female Luer Thread Style Tee | Nordson Medical | LT787-9 | Male Luer |
| Nalgene 180 Clear Plastic PVC Tubing | ThermoFisher Scientific | 8000-9020 | Tubing |
| Paraformaldehyde Aqueous Solution – 32% | Electron Microscopy Sciences | 15714-S | Fixative solution. Diluted to 4% with phosphate buffered saline |
| Permatex Ultra Blue Multipurpose RTV Silicone Gasket Maker | Permatex | 81724 | Silicone Gasket Maker for air-tight sealing of chambers |
| Phosphate-Buffered Saline, 1x Without Calcium and Magnesium | Corning | 21-040-CV | Bottle used to construct the air-inflation chamber, and buffer used for heparin and fixative solutions |
| Sterilite Ultra Seal 16.0 cup rectangle food storage container | Sterilite | 0342 | Animal processing container |
References
- Hsia, C. C. W., Hyde, D. M., Ochs, M., Weibel, E. R. An Official Research Policy Statement of the American Thoracic Society/European Respiratory Society: Standards for Quantitative Assessment of Lung Structure. American Journal of Respiratory and Critical Care Medicine. 181 (4), 394-418 (2010).
- Weibel, E. R., Limacher, W., Bachofen, H. Electron microscopy of rapidly frozen lungs: evaluation on the basis of standard criteria. Journal of Applied Physiology: Respiratory, Environmental and Exercise Physiology. 53 (2), 516-527 (1982).
- Bachofen, H., Ammann, A., Wangensteen, D., Weibel, E. R. Perfusion fixation of lungs for structure-function analysis: credits and limitations. Journal of Applied Physiology: Respiratory, Environmental and Exercise Physiology. 53 (2), 528-533 (1982).
- Gil, J., Bachofen, H., Gehr, P., Weibel, E. R. Alveolar volume-surface area relation in air- and saline-filled lungs fixed by vascular perfusion. Journal of Applied Physiology: Respiratory, Environmental and Exercise Physiology. 47 (5), 990-1001 (1979).
- Harris, R. S. Pressure-Volume Curves of the Respiratory System. Respiratory Care. 50 (1), 78-99 (2005).
- Bachofen, H., Schürch, S. Alveolar surface forces and lung architecture. Comparative Biochemistry and Physiology Part A: Molecular & Integrative Physiology. 129 (1), 183-193 (2001).
- Mead, J., Takishima, T., Leith, D. Stress distribution in lungs: a model of pulmonary elasticity. Journal of Applied Physiology. 28 (5), 596-608 (1970).
- Mariano, C. A., Sattari, S., Maghsoudi-Ganjeh, M., Tartibi, M., Lo, D. D., Eskandari, M. Novel Mechanical Strain Characterization of Ventilated ex vivo Porcine and Murine Lung using Digital Image Correlation. Frontiers in Physiology. 11, 600492 (2020).
- Braber, S., Verheijden, K. a. T., Henricks, P. a. J., Kraneveld, A. D., Folkerts, G. A comparison of fixation methods on lung morphology in a murine model of emphysema. American Journal of Physiology – Lung Cellular and Molecular Physiology. 299 (6), 843-851 (2010).
- Brain, J. D., Gehr, P., Kavet, R. I. Airway Macrophages. American Review of Respiratory Disease. 129 (5), 823-826 (1984).
- Wheeldon, E. B., Podolin, P. L., Mirabile, R. C. Alveolar Macrophage Distribution in a Mouse Model: The Importance of the Fixation Method. Toxicologic Pathology. 43 (8), 1162-1165 (2015).
- Matulionis, D. H. Lung deformation and macrophage displacement in smoke-exposed and normal mice (Mus musculus) following different fixation procedures. Virchows Archiv. A, Pathological Anatomy and Histopathology. 410 (1), 49-56 (1986).
- Gage, G. J., Kipke, D. R., Shain, W. Whole Animal Perfusion Fixation for Rodents. JoVE (Journal of Visualized Experiments). (65), e3564 (2012).
- Crosfill, M. L., Widdicombe, J. G. Physical characteristics of the chest and lungs and the work of breathing in different mammalian species. The Journal of Physiology. 158 (1), 1-14 (1961).
- Ramos-Vara, J. A. Principles and Methods of Immunohistochemistry. Drug Safety Evaluation: Methods and Protocols. , 115-128 (2017).

