Measurement of the Hepatic Venous Pressure Gradient and Transjugular Liver Biopsy
Summary
Here, we present a protocol for measurement of hepatic venous pressure gradient (HVPG),the gold standard to diagnose clinically significant portal hypertension. Moreover, we describe how to perform a transjugular liver biopsy within the same session.
Abstract
Here we provide a detailed protocol describing the clinical procedure of hepatic venous pressure gradient (HVPG) measurement in patients with advanced chronic liver disease followed by an instruction for transjugular biopsy. Under local anesthesia and ultrasound guidance, a catheter introducer sheath is placed in the right internal jugular vein. Using fluoroscopic guidance, a balloon catheter is advanced into the inferior vena cava (IVC) and inserted into a large hepatic vein. Correct and sufficient wedge position of the catheter is ensured by injecting contrast media while the balloon is blocking the outflow of the cannulated hepatic vein. After calibrating the external pressure transducer, continuous pressure recordings are obtained with triplicate recordings of the wedged hepatic venous pressure (WHVP) and free hepatic venous pressure (FHVP). The difference between FHVP and WHVP is referred to as HVPG, with values ≥10 mm Hg indicating clinically significant portal hypertension (CSPH). Before removing the catheter, pressure readings obtained in the IVC at the same level, as well as the right atrial pressure are recorded.
Finally, a transjugular liver biopsy can be obtained via the same vascular route. Different systems are available; however, core biopsy needles are preferred over aspiration needles, especially for cirrhotic livers. Again, under fluoroscopic guidance a biopsy needle introducer sheath is advanced into an hepatic vein. Next, the transjugular biopsy needle is gently advanced through the introducer sheath: (i) in case of aspiration biopsy, the needle is advanced into the liver parenchyma under aspiration and then removed quickly, or (ii) in case of a core biopsy, the cutting-mechanism is triggered inside the parenchyma. Several separate passages can be safely performed to obtain sufficient liver specimens via transjugular biopsy. In experienced hands, the combination of these procedures takes about 30-45 min.
Introduction
Patients with cirrhosis are at risk for developing complications mostly related to portal hypertension (PHT), such as ascites or bleeding from gastric or esophageal varices1,2,3. The risk of hepatic decompensation is related to the degree of PHT2. Measurement of the hepatic venous pressure gradient (HVPG) is the gold standard to estimate portal venous pressure in patient with cirrhosis, i.e. assessing the severity of sinusoidal portal hypertension4. An HVPG of ≥6 mm Hg to 9 mm Hg indicates elevated portal pressure ('subclinical portal hypertension'), while an HVPG ≥10 mm Hg defines CSPH. This protocol provides a detailed description of the equipment and the procedure and also highlights potential pitfalls and offers advice for troubleshooting.
Clinically, measurement of HVPG is indicated (i) to establish the diagnosis of sinusoidal portal hypertension, (ii) to identify patients at risk for hepatic decompensation by diagnosing CSPH (HVPG ≥10 mm Hg), (iii) to guide pharmacological therapy in primary or secondary prophylaxis of variceal bleeding, and (iv) to assess the risk of hepatic failure after partial hepatectomy2,4. HVPG is used as an established surrogate marker for improvement and/or worsening of liver fibrosis/function, since a decrease in HVPG translates into a clinically meaningful benefit5, whereas higher HVPG values are associated with an increased variceal bleeding risk6. Based on observations on changes in HVPG in patients under non-selective beta-blocker (NSBB) or etiological therapies, a decrease in HVPG of 10% is considered to be clinically relevant7,8.
To date, there are no alternative, non-invasive parameters reflecting the degree of portal pressure with similar accuracy as HVPG. Even if HVPG is actually an ‘indirect’ way to measure portal pressure, it strongly correlates and thus accurately reflects ‘directly’ measured portal pressure in patients with cirrhosis9. Importantly, HVPG measurements should be performed using a balloon catheter to maximize the assessed amount of liver parenchyma10,11,12. Although HVPG measurements are invasive, resource-intensive, and require interventional skills and expertise in interpreting the reliability and plausibility of pressure readings, this method is the current gold standard for diagnosing and monitoring portal hypertension in patients with cirrhosis13,14,15.
Simple laboratory values, such as platelet count, may help to estimate the likelihood for CSPH. However, platelet count, or non-invasive scores that include platelet count, have limited predictive value16. Imaging modalities showing splenomegaly17 or portosystemic collaterals18 in patients with cirrhosis suggest the presence of CSPH, but are not helpful for quantifying the actual degree of portal hypertension. Novel non-invasive imaging tools, such as elastography of the liver19 and/or of the spleen20 are useful for ruling-in or ruling-out the presence of CSPH. Still, none of the available methods is able to directly measure dynamic changes in portal pressure21.
The prognostic value of HVPG has been underlined by several landmark studies, showing that a HVPG ≥10 mm Hg (i.e. CSPH) is predictive for the formation of varices8 (and for the development of complications related to portal hypertension22, while a (pharmacologically-induced) decrease of HVPG modulates the respective risk of variceal growth23 and decompensation7. HVPG-response is the only established surrogate for the effectiveness of NSBBs in preventing (recurrent) variceal bleeding. If HVPG decreases to a value of ≤12 mm Hg or is reduced by ≥10-20% during NSBB treatment, patients are protected from variceal bleeding and survival is increased24,25. Similarly, HVPG-response also decreases the incidence of ascites and related complications in patients with compensated cirrhosis5,26. Several studies have provided evidence supporting the use of HVPG-guided therapy27,28,29,30,31,32. Thus, in centers with sufficient experience, HVPG-response may guide treatment decisions, facilitating personalized medicine for patients with portal hypertension.
Moreover, measuring of HVPG might serve as a surrogate endpoint for proof-of-concept studies assessing the effectiveness of novel treatments for cirrhosis and/or portal hypertension being translated from bench to bedside, such as sorafenib33,34, simvastatin35,36, taurine37, or emricasan38. Ultimately, measurements of HVPG can also provide important prognostic information about the risk for development of HCC39 and for liver failure post hepatic resection40.
The infrastructure to measure HVPG should be readily available at secondary and tertiary care centers. Since the technique of HVPG measurement requires specialized training and equipment, it seems rational for academic and transplant centers to establish a hepatic hemodynamic laboratory, facilitating state-of-the-art diagnosis and management of portal hypertension. Large volume centers perform several hundred HVPG measurements per year. Based on our experience, sufficient expertise to perform accurate HVPG measurements is usually obtained after 50-100 supervised HVPG measurements.
Protocol
The protocol described here complies with the guidelines of the human research ethics committee of the Medical University of Vienna.
1. Preparations
- Use a specialized room dedicated/approved for procedures using x-ray equipped with a digital x-ray fluoroscopy system (Figure 1A), a monitor system (Figure 1B), a pressure recorder and transducer (Figure 1C) that are connected to a printer or recording software, and an ultrasound device (Figure 1D). Also, ensure there is sufficient space for a sterile working area (Figure 1E) next to the patient bench.
- Evaluate patients with suspected advanced chronic liver disease (ACLD) for CSPH by measurement of HVPG. In particular, patients with one of the following features might undergo HVPG measurement: thrombocytopenia <150 G/L, portosystemic collaterals on cross-sectional imaging, gastroesophageal varices prior to initiation of non-selective betablocker therapy, ascites, and hepatic tumors that are scheduled for resection.
- Use the following contraindications for the procedure: (i), absence of vascular access due to jugular or caval vein thrombosis, (ii) clinically evident bleeding disorders (e.g. disseminated intravascular coagulation), (iii) contralateral pneumothorax, and (iv) significant cardiac arrhythmias.
- Ensure that the patient is fastened and gave written informed consent after being informed about the purpose and potential risks of the procedure.
- Explain that the procedure must be performed without general anesthesia. However, low doses of midazolam (up to 0.02 mg/kg bodyweight) might be offered to anxious patients.
- Monitor the patient’s vital signs by non-invasive arterial blood pressure measurement, pulse oximetry, and electrocardiography using a standard monitor system.
- Flush the pressure transducer set using sterile saline solution in a pressure bag.
- Calibrate the pressure transducer (if not precalibrated, calibrate against an external pressure reference before starting measurements, e.g. by using a water column where 13.6 cm H2O equals 10 mm Hg).
- Place the transducer at the level of the right atrium by aiming at the patient’s midaxillary line.
- Prepare the pressure recorder/recording software to be ready for recording pressure tracings.
- Ensure that all necessary sterile equipment is ready (see Table of Materials).
- Ask the patient to take a supine position on the patient bench.
- Have the operator wash and disinfect her/his hands and forearms.
- Put on surgical cap and face mask, sterile gloves and a sterile coat.
- Use a sterile table cover and prepare a sterile working area for the equipment needed for the central venous access (Figure 2A).
2. Central venous access under sterile conditions
- Instruct the patient to turn his/her head slightly to the left side, then disinfect the area of the right anterior and lateral neck with a disinfectant solution.
- Place sterile towels that cover the skin around the carotid triangle.
- Use a ultrasound probe (covered by a sterile US probe cover sheath) to identify the right internal jugular vein and the appropriate puncture site.
- Infiltrate the area of subsequent vascular access with a 21 G needle and apply a local anaesthetic (lidocaine 2%, 5 mL). Then, wait 1–2 min for its full effect.
- Prepare all materials needed for central venous access (see Table of Materials).
- Using the equipment of the 7.5 F catheter introducer sheath set, place the needle in the right internal jugular vein using ultrasound guidance and advance the guidewire through the needle using the Seldinger technique (Figure 3A).
NOTE: If a transjugular biopsy should be performed after HVPG measurement, a larger diameter 10 F liver biopsy introducer sheath set (with extra 18 G needle and guide wire) has to be used. - Make a 2-3 mm incision along the guidewire using a blade 11 scalpel to ease introduction of the vascular access sheath loaded with the dilatator.
- Insert the vascular access percutaneous sheath loaded with the dilatator into the internal jugular vein over the guidewire.
- Remove the guidewire and the dilatator of the vascular access sheath.
- Make sure that the vascular access sheath remains in a stable intravascular position and orient the injection port of the vascular access sheath towards the lateral side (Figure 3B).
NOTE: Suturing or taping is not needed.
3. Placement of the balloon catheter in a hepatic vein
- Prepare all materials needed for placement of the balloon catheter into a hepatic vein (Figure 2B).
- Flush the balloon catheter with contrast media (dye) and check the integrity of the balloon by repetitive insufflation/deflation with the catheter tip immersed in saline solution. No air bubbles should occur.
NOTE: Depending on the visibility of the catheter itself on x-ray, you may also use just sterile saline or diluted dye to flush the vascular lumen of the catheter. - Moisten the balloon catheter on the outside with sterile saline solution before inserting it into the vascular access sheath.
- Advance the balloon catheter under fluoroscopic guidance into the inferior cava vein (IVC). Aligning the tip of the balloon catheter towards the back of the patient and slight rotations of the catheter usually allows to advance from the right atrium to the IVC. Instructing the patient to inhale deeply might help in some cases (Figure 3B).
- Advance the balloon catheter from the IVC into the hepatic vein. Try to get access to the hepatic veins by repeatedly moving with the tip of the balloon catheter facing to the right towards the suspected area of the junction of the hepatic veins and the IVC (Figure 3C).
- Ensure that the catheter is advanced into a stable position that allows the repeated measurement of the free hepatic venous pressure (FHVP) at a 2-4 cm distance from its opening into the IVC and adequate space for the inflated balloon in the lumen of the hepatic vein in order to record the wedged hepatic venous pressure (WHVP).
- Check for an adequate occlusion of the vein (wedge position) by inflating the balloon (about 2 mL of air into the balloon lumen) and contrast agent injection (about 5 mL into the vascular lumen) until the hepatic vein distal to the inflated balloon is visualized (Figure 3D).
- Observe the stasis of the contrast media and exclude washout of the contrast media due to insufficient occlusion of the venous lumen by the balloon or due to the presence of vein-vein communications. If significant contrast media washout is observed, try to reposition the balloon catheter.
- Deflate the balloon and flush the lumen of the catheter with saline.
4. Hemodynamic readings for assessing the HVPG
- Connect the vascular lumen of the balloon catheter to the pressure transducer using an infusion line.
- Start recording the FHVP with the tip of the balloon 2-4 cm from the opening of the hepatic vein to the IVC. The waveform of the curve must be stable without variations over time.
NOTE: Stable values are usually obtained after 15 s. - Inflate the balloon and continue recording the WHVP until the measurement becomes a stable horizontal line with no variations over time.
NOTE: Stable tracings of the wedged pressure are usually obtained after >40 s. - Repeat the measurement of FHVG (>15 s) and WHVP (>40 s) at least three times to obtain triplicate high-quality readings (Figure 3E).
NOTE: If significant discrepancies of ≥2 mm Hg are observed between the single FHVP/WHVP readings, additional measurements should be obtained. Note the reasons for potential artefacts, such as coughing, moving, or talking at the respective timepoints of hemodynamic recording. - Record pressure in the IVC at the level of the ostium of the hepatic vein as well as the right atrial pressure (RAP).
- Stop recordings.
- Remove the balloon catheter.
- Calculate HVPG (FHVP subtracted from WHVP) as the mean of 3 measurements.
NOTE: If significant differences ≥2 mm Hg are noted between the sequentially obtained HVPG readings, additional measurements should be obtained. - Proceed to transjugular biopsy (step 5.1) or remove the catheter introducer sheath from the internal jugular vein.
NOTE: Inserting a stiff guidewire may help to reach the same intrahepatic position for subsequent transjugular liver biopsy. - Apply pressure on top of the vascular insertion site of the internal jugular vein for at least 5 min using a sterile gauze.
5. Preparation for transjugular liver biopsy
NOTE: Two different biopsy methodologies may be used to obtain a transjugular liver biopsy: aspiration (step 6) or core biopsy (step 7). First decide which system to use and then select the appropriate biopsy needle introducer sheath before proceeding with steps 5.1 to 5.3). Alternatively, the needle of the core TJBLX set can also be inserted into the aspiration set (NOTE: use appropriate diameters), which results in a more flexible core biopsy system that may be easier to introduce into a hepatic vein (NOTE: this approach is not described in detail here).
- Prepare the respective transjugular liver biopsy (TJLBX) set (aspiration TJLBX: Figure 4A-B; core TJLBX: Figure 4C; see Table of Materials).
- Flush the biopsy needle introducer sheath with sterile saline or, in case of transjugular aspiration liver biopsy, with contrast agent for better visualization.
- Advance the biopsy needle introducer sheath into a hepatic vein using the same technique as described in 3.4.
- Depending on the biopsy set used, proceed either to step 6.1 for aspiration TJBX or to step 7.1 for core TJBX.
6. Transjugular aspiration liver biopsy
- Use a 10 mL Luer-lock syringe to flush the aspiration TJLBX needle with sterile saline, however, leave about 3 mL in the syringe to facilitate aspiration.
- Advance the biopsy needle gently through the biopsy needle introducer sheath until the tip of the needle reaches the end of the introducer sheath.
NOTE: Avoid any force or fast movements while advancing the needle. Asking the patient to take a deep breath will decrease the angle between the IVC and the hepatic veins for easier advancement of the biopsy needle. - Ask the patient to hold his breath.
- Apply suction using the 10 mL Luer-lock syringe and advance the needle into the liver parenchyma.
- Retract the needle while still applying suction (negative pressure).
- Advice the patient to continue breathing normally.
- Remove the needle (but not the needle introducer sheath) and harvest the liver sample.
NOTE: The liver sample is usually retained in the syringe, not in the needle (Figure 4D). - Repeat steps 6.1 to 6.6 for additional needle passages until sufficient liver specimens are obtained.
- Inject 5-10 mL of contrast media over the catheter introducer sheath to rule out perforation of the liver capsule.
- Remove the biopsy needle introducer sheath.
- Remove the 10 F liver biopsy set introducer sheath and apply pressure on top of the vascular insertion site of the internal jugular vein for at least 5 min using sterile gauzes.
7. TRANSJUGULAR CORE LIVER BIOPSY
- Load the core TJLBX needle by pulling the grip until the shooting mechanism is locked. Advance the core biopsy needle gently through the biopsy needle introducer sheath until the tip of the needle approaches the end of the introducer sheath.
NOTE: Avoid any force or fast movements while advancing the needle. - Ask the patient to hold his/her breath.
- Advance the needle into the liver parenchyma.
- Perform the core biopsy by pulling the trigger of the shooting mechanism.
- Advice the patient to continue breathing normally.
- Remove the needle (but not the needle introducer sheath) and harvest the liver sample. A small needle might help to remove the liver sample (Figure 4D).
- Repeat steps 7.1 to 7.6 for additional needle passages until sufficient liver specimens are obtained.
- Inject 5-10 mL of contrast media over the side port of the catheter introducer sheath to rule out perforation of the liver capsule.
- Remove the biopsy needle introducer sheath.
- Remove the 10 F liver biopsy set introducer sheath and apply pressure on top of the vascular insertion site of the internal jugular vein for about 5 min using sterile gauzes.
Representative Results
In compensated patients with well-preserved liver function (i.e. without any history of hepatic decompensation, such as ascites or variceal bleeding) the measured HVPG values might be normal or in the range of subclinical portal hypertension (HVPG 6–9 mm Hg). However, compensated patients might develop CSPH (HVPG ≥10 mm Hg) which indicates an increased risk for developing varices or hepatic decompensation. In turn, patients with esophageal or gastric varices, HVPG is usually in the range of CSPH, if not patients should be assessed for the presence of portal vein thrombosis or other reasons for prehepatic/presinusoidal portal hypertension. In patients with a history of bleeding from esophageal varices, HVPG is usually at least ≥12 mm Hg. Similarly, in patients with ascites due to cirrhosis, i.e., portal-hypertensive ascites, the HVPG values are usually expected to be at least ≥10 mm Hg (Figure 3E). HVPG values of ≥20 mm Hg indicate high risk of failure to control bleeding and/or recurrent variceal bleeding and patients should be candidates for preemptive transjugular intrahepatic portosystemic shunt (TIPS) placement, if they develop variceal bleeding. While HVPG values might rise to values >30 mm Hg in patients with advanced cirrhosis and severe portal hypertension, HVPG values of >40 mm Hg are very unusual and the accuracy of the measurement and the pressure tracings should be critically assessed.
Very high values of FHVP and IVC may hint to incorrect calibration of the pressure transducer but might also indicate right heart failure or tricuspide valve regurgitation. A difference of more than ≥4mm Hg between the FHVP and the IVC pressure is suggestive of an outflow obstruction/stenosis of the hepatic vein or Budd-Chiari Syndrome. However, in case of severe Budd-Chiari Syndrome with complete thrombotic obstruction of the hepatic veins, the insertion of the balloon catheter is usually not possible. Thus, in case Budd-Chiari Syndrome or other causes of hepatic outflow obstruction are suspected, a Doppler ultrasound examination of the hepatic veins is recommended.
If shunts are observed during contrast media injection while the balloon is inflated, the HVPG is typically underestimated. However, while in this case the absolute value of HVPG cannot be used to estimate prognosis or guide pharmacological therapy, the diagnosis of CSPH can still be made if the HVPG is recorded at ≥10 mm Hg.
In primary prophylaxis of variceal bleeding, hemodynamic response to non-selective betablocker therapy (e.g. with carvedilol 12.5 mg once daily) is defined as an HVPG decrease of at least ≥10% compared to baseline, or as a decrease to absolute values <12 mm Hg: e.g., patient A (who had no previous episode of variceal bleeding) has a baseline HVPG of 20mm Hg. Following administration of carvedilol 12.5 mg/day for 4 weeks, a second HVPG (on carvedilol) of 16 mm Hg is recorded. Thus, HVPG decreased by 4 mm Hg (i.e. 20% of baseline HVPG), indicating a hemodynamic response.
In secondary prophylaxis of variceal bleeding, hemodynamic response requires an HVPG decrease of ≥20% (or to absolute values <12 mm Hg): e.g., patient B has a baseline HVPG of 26 mm Hg and under propranolol 40 mg b.i.d. (80 mg cumulative daily dose) HVPG drops to 24 mm Hg, which is a decrease of just 8%, indicating hemodynamic non-response. In absence of a hemodynamic response, patient B has a high risk of rebleeding if treated with propranolol 40 mg b.i.d only.
It has been shown that HVPG-guided pharmacological therapy plus endoscopic band ligation is more effective than ‘uncontrolled‘ combined therapy of NSBB plus endoscopic band ligation in secondary prophylaxis and even improved survival32.
Transjugular liver biopsy can be safely performed in the same session using the same vascular access sheath after recording HVPG. Liver biopsy specimens obtained with transjugular aspiration biopsy needles might be fragmented, especially in patients with cirrhosis, and thus, less representative than biopsies obtained with core biopsy needles. However, in patients in whom less pronounced liver fibrosis is expected, aspiration needle biopsy yields good sample quality with usually larger diameter specimens being obtained.
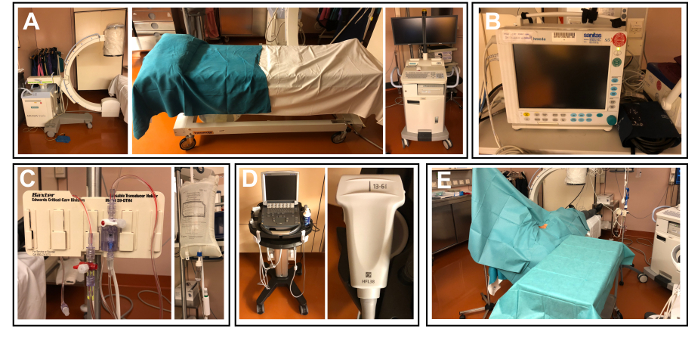
Figure 1: Equipment needed for a hepatic hemodynamic laboratory. (A) Room dedicated/approved for procedures using x-ray with a digital x-ray fluoroscope system. (B) Monitor system for vital signs, i.e., ECG, non-invasive blood pressure, and oxygen saturation. (C) Pressure transducer with pressurized sterile saline flush. (D) Ultrasound device for guiding vascular access. (E) Sterile working area. Please click here to view a larger version of this figure.
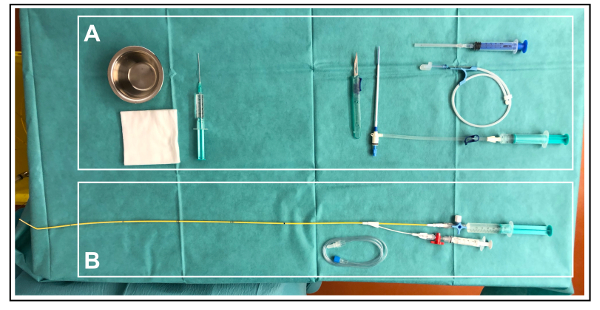
Figure 2: Sterile equipment needed for HVPG measurement. This figure shows the sterile working area prepared with the materials needed for (A) central venous access and (B) placement of the balloon catheter in a hepatic vein. Please click here to view a larger version of this figure.
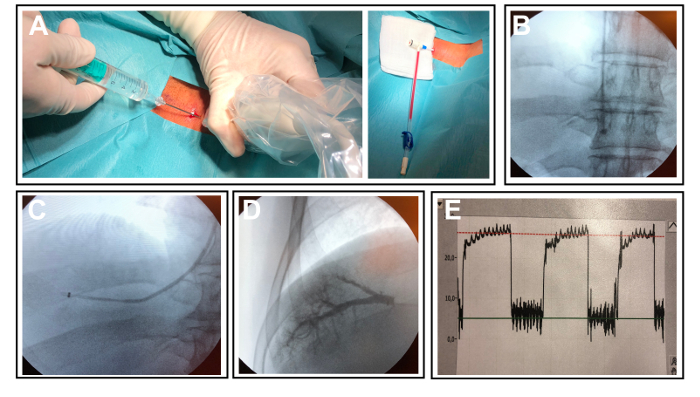
Figure 3: Placement of the catheter introducer sheath and correct positioning of the balloon catheter. (A) Catheter introducer sheath correctly placed in the right internal jugular vein. (B) Balloon cather advanced into the IVC. (C) Balloon catheter advanced into the right hepatic vein. (D) Balloon catheter with inflated balloon and hepatic vein visualized by contrast media injection. (E) Representative pressure tracing of the free and wedged hepatic pressure readings. Please click here to view a larger version of this figure.
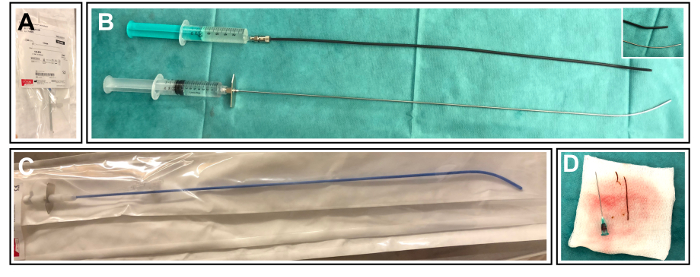
Figure 4. Equipment needed for transjugular liver biopsy. (A) 10 F transjugular liver biopsy set introducer sheath. (B) Transjugular aspiration biopsy system including the biopsy needle introducer sheath and the transjugular aspiration biopsy needle connected to a 10 mL Luer-lock syringe. (C) Transjugular core biopsy system including the needle introducer sheath with a side port and the core biopsy needle. (D) Liver specimen obtained by transjugular biopsy. Please click here to view a larger version of this figure.
Discussion
While HVPG measurements require considerable resources and trained personal with interventional skills and expertise in the reading of pressure tracings, it improves prognostication and might guide treatment decisions, and thus, facilitates personalized medicine. In addition, the opportunity to safely obtain liver biopsy specimens via the transjugular route in the same session is another argument in favor of implementing hepatic hemodynamic laboratories at tertiary care centers. Indeed, guidelines support the use of HVPG measurements in centers with adequate expertise and resources2,4. The safety of the procedures is largely related to the vascular access to the internal jugular vein. Once correctly placed, the risk of the remaining procedure is negligible and patient’s comfort is mostly limited by the duration of the procedure, if placement of the balloon catheter in the hepatic vein takes longer as expected. While a recently published study on patient-reported outcomes demonstrated that the HVPG procedure is well-tolerated41, low dose midazolam sedation (up to 0.02 mg/kg body weight) may be used to relief anxiety and to promote patient comfort42. However, general anesthesia and/or deep-sedation with propofol and remifentanil cannot be used for HVPG measurements, since this would impact on hemodynamic readouts43.
In case the right internal jugular vein cannot be used for venous access (e.g. in case of thrombosis), the left internal jugular vein or alternative vessels may be used instead. Importantly, HVPG can also be measured via the femoral veins given specialized catheters are used.
However, the most critical part of HVPG measurements is the correct recording of pressure tracings while the balloon is insufflated and deflated, ensuring that proper placement and sufficient time are assured to obtain the correct WHVP and FHVP. The waveforms obtained in the "free" position of the catheter might be slightly impacted by the heart beat or a physiologic tricuspid valve regurgitation during systole, however, should still follow a straight line. In contrast the "wedged" pressure curve obtained when the balloon is inflated should follow a fast increase during the first 3-5 s followed by a more slowly increase over 10-30 s. Finally, a straight and stable line should be obtained which reflects the correct sinusoidal pressure. Any inconsistencies occurring during triplicate measurements should prompt the operator to obtain additional pressure readings in order to identify the correct FHVP and WHVP.
The complication rate of HVPG measurement is low and the risks are almost exclusively related to the venous access usually performed at the right internal jugular vein11,13. Common side effects of the HVPG procedure that should be discussed with the patients prior to the procedure include pain at the insertion site or slight thoracic or abdominal discomfort when advancing the catheter through the vena cava system into the hepatic veins and while inflating the balloon. Specific but rare complications related to the venous access include hematomas at the access site, pneumothoraces requiring a chest tube and cardiac arrhythmias.
The four main indications for HVPG measurements are (i) to establish the diagnosis of intrahepatic portal hypertension, (ii) to identify patients at risk for hepatic decompensation by diagnosing CSPH (HVPG ≥10 mm Hg), (iii) to guide pharmacological therapy in primary or secondary prophylaxis of variceal bleeding, and (iv) assess the risk of hepatic failure after partial hepatectomy. While CSPH diagnosis and risk stratification might also be performed by imaging/laboratory studies or by endoscopy2,44, currently, there are no adequate alternative means to monitor the response to NSBB therapy. While some patients might be readily excluded from major hepatic resection by considering signs of hepatic impairment (i.e. ascites or jaundice)45, measurement of HVPG represents an important predictor of postsurgical morbidity and mortality in patients with otherwise well-preserved liver function (i.e. compensated patients)46.
HVPG correlates well with directly measured portal pressure (or more precisely, the pressure gradient throughout the liver), as it has been shown for patients with alcoholic and viral etiology of liver disease9. However, certain liver diseases (e.g. nodular regenerative hyperplasia) might also affect presinusoidal resistance which impacts on the severity of portal hypertension but is not adequately reflected by HVPG47. Furthermore, HVPG is also not able to detect the presence of (additional) prehepatic portal hypertension, as caused by portal vein thrombosis or mechanical compression of the portal vein. Thus, abdominal imaging with a special focus on the splenoportal vascular axis, on the mesenteric veins, as well as on spleen size and the presence of ascites should be performed in unclear cases and whenever a prehepatic component of portal hypertension is suspected48.
Finally, the use of transjugular liver biopsy has been demonstrated to be safe in patients with contraindications for percutaneous liver biopsy, e.g., due to inherited or acquired bleeding disorders or in case of severe ascites49,50. In addition, the development of core biopsy needles has increased the diagnostic yield of TJBX51,52. In case of acute liver failure of unknown etiology, or in case of suspected cirrhosis, transjugular biopsy should be favored over percutaneous liver biopsy for safety reasons in most cases. In decompensated patients, percutaneous liver biopsy is associated with considerable risks of severe bleeding or procedure-related complications, while in compensated patients, the respective risks are lower. Still, we prefer to perform TJBX in all patients with cirrhosis (including compensated patients) as important prognostic information through HVPG measurements can be simultaneously obtained.
Declarações
The authors have nothing to disclose.
Acknowledgements
The Vienna General Hospital and the Medical University of Vienna kindly provides the infrastructure for the Vienna Hepatic Hemodynamic Laboratory. Previous members of the Vienna Hepatic Hemodynamic Laboratory and coworkers should be acknoweledged for their valuable input that helped to continuously improve the methodology of HVPG measurement and transjugular liver biopsy at our institution. In addition, we thank the nurses of the Division of Gastroenterology and Hepatology who are an essential part of the Vienna Hemodynamic Laboratory and continuously provide patients with excellent care.
Materials
| 10 mL Luer-Lock syringe | Braun | REF 4617100V, LOT 17G03C8 | Luer-Lock Syringe for connection with the aspiration biopsy set |
| 10 mL Syringe 2x | Braun | REF 4606108V | Snonpyrogenic, nontoxic 10 mL syringe |
| 10 F liver biopsy introducer sheath set | Cook Medical | REF RCFW-10.0-38, REF G07600 | Percutaneous Sheath Introducer Set (TJBX), 10F Port, 13cm, Check-Flo Performer Introducer |
| 18 G needle for biopsy introducer sheat | Arrow International | REF AN-04318 | Introducer Needle for TJBX Set, 18 G, 6.35 cm |
| 21 G needle | Henke Sass Wolf | REF 0086, Fine-Ject 21Gx2" | Sterile injeciton needle, 21 Gx2", 0.8 x 50 mm, for local anesthesia |
| 3-way channels | Becton Dickinson | BD Connecta Luer-Lok, REF 39402 | Three way channel with Luer-Lok connection system |
| 7.5 F catheter introducer sheath set | Arrow International | REF SI_09875-E | Percutaneous Sheath Introducer Set, 7.5 F Port |
| Aspiration TJLBX set | Cook Medical | REF RMT-16-51.0-TJL, REF G20521 | TJ Liver Access and Biopsy Needle Set (Aspiration Set), 9 F-45 cm, 16 G-50.5 cm |
| Balloon catheter | Gerhard Pejcl Medizintechnik Austria | REF 500765B | Ferlitsch HVPG Catheter, 7F-65cm, Balloon:2.5mL, Pressure 50-90 kPa, GW: 0.032" |
| Blade 11 scalpel | Medi-Safe Surgicals | MS Safety Scalpel REF /Batch 18012424 | 11 blade safety scalpels, retractable, single use, 10 scalpels per package |
| Blunt tip fill needle | Becton Dickinson | REF 303129 | Sterile blunt tip fill needle, single use |
| Contrast media (dye) | Dr. Franz Köhler Chemie GmbH, Bensheim, GER | ZNR 1-24112 | Peritrast 300 mg Iod/mL, 50 mL, contrastmedia |
| Core TJLBX set | Cook Medical | REF RMT-14XT-50.5-LABS-100, REF G08285 | TJ Needle Introducer and Bx-Needle 7 F-53.5 cm, 14 G-53.5 cm/20 mm, 18 G-60 cm |
| Digital x-ray fluoroscope system | Siemens | Model No 07721710 | ARCADIS Varic, mobile x-ray fluoroscope system |
| Disinfectant solution | Gebro Pharma | 1-20413 | Isozid-H |
| Face mask | MSP Medizintechnik GmbH | REF HSO36984 | Surgical face mask from double fleece, with tie, 50 pieces |
| Guide wire for biopsy introducer sheat | Arrow International | REF AW-14732 | Marked Spring-Wire Guide, TJBX Set, 0.032", 0.81 mm, 68 cm |
| Infusion line | Rosstec Medical Products b Cardea GmbH & Co | REF 220010, 100m | Infusion line, Luer-Lok for connection of balloon catheter and pressure transducer |
| Lidocaine 2% | Gebro Pharma | Xylanaest, ZNR 17.792, 20mg/1mL (2%) | Sterile vials Xylanest including 2% Lidocain hydrochloride for local anesthesia |
| Midazolame | Roche | Dormicum, ZNr 1-18809, Midazolam 5mg/5mL | Sterile vials Dormicum including Midazolam for sedation |
| Monitor system | Datex-Ohmeda by GE | Type F-CMREC1 | Patient monitoring system |
| Patient bench | Silerlen-MAQET | Model No 7474.00A | Mobile patient bench for x-ray fluoroscopy |
| Pressure bag | Ethox Corp | REF 4005 | Pressure Infuser Bag 500 mL |
| Pressure recorder | Edwards Lifesciences | Ref T001631A, Lot 61202039 | TruWave 3 cc/150 cm |
| Pressure transducer | Edwards Lifesciences TM | REF T001631A | Pressure Monitoring Set (1x), 3 cc/150 cm, TruWave TM |
| Recording software | Datex Ohmeda by GE | Software S/5 is property of Instrumentarium Corp of Datex-Ohmeda TM | Datex-Ohmeda S/5TM Collect – Software to record pressure tracings of the patient monitor system |
| Sterile coat | Lohmann & Rauscher International GmbH & Co | REF 19351 | Surgical Gown, Different sizes, e.g. L-130 cm |
| Sterile gauze | Hartmann | REF 401798, 10x10cm gauze | 10 x 10 cm sterile gauze, 10 pieces per package |
| Sterile gloves | Meditrade | REF 9021 | Gentle Skin sterile gloves, different sizes, e.g. 7.5 |
| Sterile saline solution | Fresenius Kabi | NaCl 0.9%, B009827 REV 03 | Physiologic Saline Solution 0.9% NaCl, 309 mosmol/L, pH-Wert: 4.5-7.0 |
| Sterile saline vessel | KLS Martin | REF K8A, 18/10 Jonas | Sterilizable Metal Vessel for sterile saline |
| Sterile table cover | Hartmann | REF 2502208 | Table Cover, Foliodrape 150 x 100 cm |
| Sterile towel | BARRIER by Mölnlycke Health Care | REF 706900 | Adhesive OP-Towel, 100 x 100 cm |
| Sterile US probe cover sheath | Websinger | REF 07014 | Sterile ultrasound probe cover, 20 x 60 cm, inluding two sterie adhesive tapes |
| Stiff guidewire | Cook Medical | REF TSMG-35-180-4-LES, G46729 | Lunderquist Extra Stiff Wire Guide, 0.035"-.89 mm, 180 cm, 4 cm flexible tip |
| Surgical cap | BARRIER by Mölnlycke Health Care | REF 620500, PCS 100, Colour Green | Surgical Cap |
| Ultrasound device | FUJIFILM SonoSite | Model M-Turbo, REF P17000-17 | Mobile ultrasound system |
Referências
- Tsochatzis, E. A., Bosch, J., Burroughs, A. K. Liver cirrhosis. The Lancet. 383 (9930), 1749-1761 (2014).
- de Franchis, R., Baveno, V. I. F. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. Journal of Hepatology. 63 (3), 743-752 (2015).
- Ge, P. S., Runyon, B. A. Treatment of Patients with Cirrhosis. The New England Journal of Medicine. 375 (8), 767-777 (2016).
- Reiberger, T., et al. Austrian consensus guidelines on the management and treatment of portal hypertension (Billroth III). Wiener klinische Wochenschrift. 129, 135-158 (2017).
- Mandorfer, M., et al. Changes in Hepatic Venous Pressure Gradient Predict Hepatic Decompensation in Patients Who Achieved Sustained Virologic Response to Interferon-Free Therapy. Journal of Hepatology. 71 (3), 1023-1036 (2020).
- Mandorfer, M., et al. Von Willebrand factor indicates bacterial translocation, inflammation, and procoagulant imbalance and predicts complications independently of portal hypertension severity. Alimentary Pharmacology and Therapeutics. 47 (7), 980-988 (2018).
- Mandorfer, M., et al. Hepatic Venous Pressure Gradient Response in Non-Selective Beta-Blocker Treatment—Is It Worth Measuring?. Curr Hepatology Reports. 18 (2), 174-186 (2019).
- Groszmann, R. J., et al. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. The New England Journal of Medicine. 353 (21), 2254-2261 (2005).
- Thalheimer, U., et al. Assessment of the agreement between wedge hepatic vein pressure and portal vein pressure in cirrhotic patients. Digestive and Liver Disease. 37 (8), 601-608 (2005).
- Zipprich, A., Winkler, M., Seufferlein, T., Dollinger, M. M. Comparison of balloon vs. straight catheter for the measurement of portal hypertension. Alimentary Pharmacology and Therapeutics. 32 (11-12), 1351-1356 (2010).
- Ferlitsch, A., et al. Evaluation of a new balloon occlusion catheter specifically designed for measurement of hepatic venous pressure gradient. Liver International. 35 (9), 2115-2120 (2015).
- Silva-Junior, G., et al. The prognostic value of hepatic venous pressure gradient in patients with cirrhosis is highly dependent on the accuracy of the technique. Hepatology. 62 (5), 1584-1592 (2015).
- Abraldes, J. G., Sarlieve, P., Tandon, P. Measurement of portal pressure. Clinical Liver Disease. 18 (4), 779-792 (2014).
- Groszmann, R. J., Wongcharatrawee, S. The hepatic venous pressure gradient: anything worth doing should be done right. Hepatology. 39 (2), 280-282 (2004).
- Bosch, J., Abraldes, J. G., Berzigotti, A., Garcia-Pagan, J. C. The clinical use of HVPG measurements in chronic liver disease. Nature Reviews Gastroenterology & Hepatology. 6 (10), 573-582 (2009).
- Wang, L., et al. Diagnostic efficacy of noninvasive liver fibrosis indexes in predicting portal hypertension in patients with cirrhosis. PLoS One. 12 (8), 0182969 (2017).
- Berzigotti, A., et al. Elastography, spleen size, and platelet count identify portal hypertension in patients with compensated cirrhosis. Gastroenterology. 144 (1), 102-111 (2013).
- Berzigotti, A., et al. Prognostic value of a single HVPG measurement and Doppler-ultrasound evaluation in patients with cirrhosis and portal hypertension. Journal of Gastroenterology. 46 (5), 687-695 (2011).
- Reiberger, T., et al. Noninvasive screening for liver fibrosis and portal hypertension by transient elastography–a large single center experience. Wiener klinische Wochenschrift. 124 (11-12), 395-402 (2012).
- Colecchia, A., et al. Measurement of spleen stiffness to evaluate portal hypertension and the presence of esophageal varices in patients with HCV-related cirrhosis. Gastroenterology. 143 (3), 646-654 (2012).
- Reiberger, T., et al. Non-selective beta-blockers improve the correlation of liver stiffness and portal pressure in advanced cirrhosis. Journal of Gastroenterology. 47 (5), 561-568 (2012).
- Ripoll, C., et al. Hepatic venous pressure gradient predicts clinical decompensation in patients with compensated cirrhosis. Gastroenterology. 133 (2), 481-488 (2007).
- Merkel, C., et al. A placebo-controlled clinical trial of nadolol in the prophylaxis of growth of small esophageal varices in cirrhosis. Gastroenterology. 127 (2), 476-484 (2004).
- Groszmann, R. J., et al. Hemodynamic events in a prospective randomized trial of propranolol versus placebo in the prevention of a first variceal hemorrhage. Gastroenterology. 99 (5), 1401-1407 (1990).
- Feu, F., et al. Relation between portal pressure response to pharmacotherapy and risk of recurrent variceal haemorrhage in patients with cirrhosis. The Lancet. 346 (8982), 1056-1059 (1995).
- Hernandez-Gea, V., et al. Development of ascites in compensated cirrhosis with severe portal hypertension treated with beta-blockers. The American Journal of Gastroenterology. 107 (3), 418-427 (2012).
- Sharma, P., Kumar, A., Sharma, B. C., Sarin, S. K. Early identification of haemodynamic response to pharmacotherapy is essential for primary prophylaxis of variceal bleeding in patients with ‘high-risk’ varices. Alimentary Pharmacology and Therapeutics. 30 (1), 48-60 (2009).
- Villanueva, C., et al. Clinical trial: a randomized controlled study on prevention of variceal rebleeding comparing nadolol + ligation vs. hepatic venous pressure gradient-guided pharmacological therapy. Alimentary Pharmacology and Therapeutics. 29 (4), 397-408 (2009).
- Gonzalez, A., et al. Hemodynamic response-guided therapy for prevention of variceal rebleeding: an uncontrolled pilot study. Hepatology. 44 (4), 806-812 (2006).
- Reiberger, T., et al. Carvedilol for primary prophylaxis of variceal bleeding in cirrhotic patients with haemodynamic non-response to propranolol. Gut. 62 (11), 1634-1641 (2013).
- Sauerbruch, T., et al. Prevention of Rebleeding From Esophageal Varices in Patients With Cirrhosis Receiving Small-Diameter Stents Versus Hemodynamically Controlled Medical Therapy. Gastroenterology. 149 (3), 660-668 (2015).
- Villanueva, C., et al. A randomized trial to assess whether portal pressure guided therapy to prevent variceal rebleeding improves survival in cirrhosis. Hepatology. 65 (5), 1693-1707 (2017).
- Reiberger, T., et al. Sorafenib attenuates the portal hypertensive syndrome in partial portal vein ligated rats. Journal of Hepatology. 51 (5), 865-873 (2009).
- Pinter, M., et al. The effects of sorafenib on the portal hypertensive syndrome in patients with liver cirrhosis and hepatocellular carcinoma–a pilot study. Alimentary Pharmacology and Therapeutics. 35 (1), 83-91 (2012).
- Abraldes, J. G., et al. Simvastatin lowers portal pressure in patients with cirrhosis and portal hypertension: a randomized controlled trial. Gastroenterology. 136 (5), 1651-1658 (2009).
- Abraldes, J. G., et al. Simvastatin treatment improves liver sinusoidal endothelial dysfunction in CCl4 cirrhotic rats. Journal of Hepatology. 46 (6), 1040-1046 (2007).
- Schwarzer, R., et al. Randomised clinical study: the effects of oral taurine 6g/day vs placebo on portal hypertension. Alimentary Pharmacology and Therapeutics. 47 (1), 86-94 (2018).
- Garcia-Tsao, G., et al. Emricasan (IDN-6556) Lowers Portal Pressure in Patients With Compensated Cirrhosis and Severe Portal Hypertension. Hepatology. , (2018).
- Ripoll, C., et al. Hepatic venous pressure gradient predicts development of hepatocellular carcinoma independently of severity of cirrhosis. Journal of Hepatology. 50 (5), 923-928 (2009).
- Stremitzer, S., et al. Value of hepatic venous pressure gradient measurement before liver resection for hepatocellular carcinoma. British Journal of Surgery. 98 (12), 1752-1758 (2011).
- Casu, S., et al. A prospective observational study on tolerance and satisfaction to hepatic haemodynamic procedures. Liver International. 35 (3), 695-703 (2015).
- Steinlauf, A. F., et al. Low-dose midazolam sedation: an option for patients undergoing serial hepatic venous pressure measurements. Hepatology. 29 (4), 1070-1073 (1999).
- Reverter, E., et al. Impact of deep sedation on the accuracy of hepatic and portal venous pressure measurements in patients with cirrhosis. Liver International. 34 (1), 16-25 (2014).
- Abraldes, J. G., et al. Noninvasive tools and risk of clinically significant portal hypertension and varices in compensated cirrhosis: The “Anticipate” study. Hepatology. 64 (6), 2173-2184 (2016).
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. Journal of Hepatology. , (2018).
- Boleslawski, E., et al. Hepatic venous pressure gradient in the assessment of portal hypertension before liver resection in patients with cirrhosis. British Journal of Surgery. 99 (6), 855-863 (2012).
- Bissonnette, J., et al. Hepatic hemodynamics in 24 patients with nodular regenerative hyperplasia and symptomatic portal hypertension. Journal of Gastroenterology and Hepatology. 27 (8), 1336-1340 (2012).
- Escorsell, A., Garcia-Pagan, J. C., Bosch, J. Assessment of portal hypertension in humans. Clinical Liver Disease. 5 (3), 575-589 (2001).
- DiMichele, D. M., Mirani, G., Wilfredo Canchis, P., Trost, D. W., Talal, A. H. Transjugular liver biopsy is safe and diagnostic for patients with congenital bleeding disorders and hepatitis C infection. Haemophilia. 9 (5), 613-618 (2003).
- Kalambokis, G., et al. Transjugular liver biopsy–indications, adequacy, quality of specimens, and complications–a systematic review. Journal of Hepatology. 47 (2), 284-294 (2007).
- Cholongitas, E., Burroughs, A. K. Liver: Transjugular liver biopsy yields high-quality samples. Nature Reviews Gastroenterology & Hepatology. 9 (9), 491-492 (2012).
- Banares, R., et al. Randomized controlled trial of aspiration needle versus automated biopsy device for transjugular liver biopsy. Journal of Vascular and Interventional Radiology. 12 (5), 583-587 (2001).

