Assay for Phosphorylation and Microtubule Binding Along with Localization of Tau Protein in Colorectal Cancer Cells
Summary
This manuscript describes standard protocols for measuring tau hyperphosphorylation, measuring tau binding to microtubules, and localization of intracellular tau following drug treatments. These protocols can be used repetitively for screening drugs or other compounds that target tau hyperphosphorylation or microtubule binding.
Abstract
The microtubule-associated protein tau is a neuronal protein that localizes mostly in axons. Generally tau is essential for normal neuronal functioning because it is involved in microtubule assembly and stabilization. Besides neurons, tau is expressed in human breast, prostate, gastric, colorectal, and pancreatic cancers where it shows nearly similar structure and exerts similar functions as the neuronal tau. The amount of tau and its phosphorylation can change its function as a stabilizer of microtubules, and lead to the development of paired helical filaments in different neurodegenerative disorders, such as Alzheimer's disease. Determining the phosphorylation state of tau and its microtubule-binding characteristics is important. In addition, examining the intracellular localization of tau is important in different diseases. This manuscript details standard protocols for measuring tau phosphorylation and tau binding to microtubules in colorectal cancer cells with or without curcumin and LiCl treatment. These treatments can be used to stop cancer cell proliferation and development. Intracellular localization of tau is examined by using immunohistochemistry and confocal microscopy while using low amounts of antibodies. These assays can be used repetitively for screening compounds that affect tau hyperphosphorylation or microtubule binding. Novel therapeutics used for different tauopathies or related anticancer agents can potentially be characterized using these protocols.
Introduction
Tau was originally identified as a heat-stable microtubule-associated protein that was co-purified with tubulin1. Tau is exclusively expressed in higher eukaryotes2,3,4. The main function of tau is to control microtubule assembly1,5,6. It also contributes to polymerization of microtubules7, axonal transport8, changes in axonal diameter9, formation of neuroma polarity, and neurodegeneration10. Tau also acts as a protein scaffold to control some signaling pathways. Rat brain studies suggest that tau is neuron-specific and that it primarily localizes in axons11. Because tau is essential for microtubule polymerization and neuronal development, tau was hypothesized to play a major role in axonal development in the central nervous system; this hypothesis was later verified by in vitro and in vivo experiments. In addition to neurons, tau is expressed in different non-neuronal cells, including liver, kidney, and muscle cells12,13. Tau is expressed also in human breast, prostate, colorectal, gastric, and pancreatic cancer cell lines and tissues14,15,16,17,18,19. Tau is also found in inclusion-body myositis as twisted tubulofilaments in inclusion bodies20.
Tau may carry several post-translational modifications. Of all post-translational modifications, phosphorylation is the most common. Increased tau phosphorylation decreases its affinity for microtubules, finally destabilizing the cytoskeleton. Eighty-five phosphorylation sites have been described in tau protein isolated from human Alzheimer's disease brain tissues. Of these sites, 53% constitute serine, 41% threonine, and only 6% tyrosine residues21,22,23. Tau phosphorylation affects its localization, function, binding, solubility, and its susceptibility to other post-translational modifications. Also tau phosphorylation to more than the normal extent (or fully saturated with phosphate groups) is known as hyperphosphorylation that replicates structural and functional characteristics of Alzheimer's disease24. Tau maintains proper functioning of the axonal microtubules and ensures normal neuronal functioning under physiological conditions. However, hyperphosphorylated tau fails to maintain a well-organized microtubule binding, causing neuronal loss because of microtubule disassembly. Normal levels of tau phosphorylation are required for proper tau functioning, but tau fails to function normally if its characteristic phosphorylation level is altered and if it is hyperphosphorylated25. In Alzheimer's disease and some other age-related neurodegenerative disorders, tau becomes hyperphosphorylated and forms the paired helical filaments and neurofibrillary tangles26,27. Thus, methods for determining tau phosphorylation and microtubule binding are important.
Colorectal cancer, an ageing-associated cancer, is the third most frequently diagnosed cancer and the third prominent death-causing cancer for both men and women28. Colorectal cancer is one of the main death-causing cancers in the Western world29. Because both colorectal cancer and Alzheimer's disease are associated with ageing and both happen mainly in the developed countries where people enjoy similar dietary habits, the two diseases may somehow be correlated. In addition, tau-positive and tau-negative cancer cells respond differently to chemotherapeutic agents, e.g., paclitaxel16.
Curcumin is one of the main derivatives of Curcuma longa, the Indian spice turmeric30. For centuries, South Asian populations have consumed turmeric in their diets on a daily basis. Curcumin is used to treat different diseases, including colorectal cancer, Alzheimer's disease, diabetes, cystic fibrosis, inflammatory bowel disease, arthritis, hyperlipidemia, atherosclerosis, and ischemic heart disease31,32,33,34,35,36,37,38. Lithium can also kill colorectal cancer cells or prevent their proliferation39. Lithium can also be used for treating Alzheimer's disease40 as it decreases tau aggregation and prevents its hyperphosphorylation as observed in a transgenic mouse model41,42,43,44.
This manuscript aims to: 1) measure the total tau and phospho-tau expression levels in treated cells; 2) describe a phosphatase assay to measure overall tau phosphorylation; 3) examine microtubule-binding of tau; and 4) localize tau by confocal microscopy in colorectal cancer cell lines treated with curcumin or LiCl. Results reveal that cell treatment with curcumin, which is a supposedly good chemotherapeutic agent for colon cancer, and treatment with LiCl can reduce expression of both total tau and phosphorylated tau in colorectal cancer cell lines. These treatments can also cause nuclear translocation of tau. However, unexpectedly, curcumin fails to improve binding of tau to microtubules.
Protocol
1. Preparation of Reagents
- Add 10 µL of (1 mM) phenylmethylsulfonyl fluoride solution, 10 µL (1x from 100x stock) of protease inhibitor cocktail solution, and 10 µL (1x from 100x stock) of phosphatase inhibitor cocktail solution to 1 mL of 1x radioimmunoprecipitation assay (RIPA) buffer to prepare the complete RIPA lysis buffer.
- Prepare 10x general tubulin buffer (PEM) buffer.
- Add 800 mM (6.0474 g) piperazine-N-N'-bis-2-ethanesulfonic acid, 10 mM (95.1 mg) ethylene glycol-bis(β-aminoethyl ether)-N,N,N',N'-tetraacetic acid, 10 mM (51 mg) MgCl2, and 1.25 M (3 mL of 10 M) NaOH in a 50-mL tube, mix with 15 mL distilled water, and dissolve by using a vortex. Check the pH (should be 6.9). If pH > 6.9, discard the buffer and remake a fresh lot.
NOTE: NaOH should be below 1.25 M to ensure that pH does not overshoot 6.9. It is not advised to use HCl for adjusting pH >6.9. - Add NaOH dropwise until pH is 6.9. Add distilled water to make up to 25 mL of 10X PEM buffer. Finally, filter using a syringe and a 0.2 µm syringe filter. Divide this buffer into aliquots in 1.5 mL tubes and store at 4 °C.
- Add 800 mM (6.0474 g) piperazine-N-N'-bis-2-ethanesulfonic acid, 10 mM (95.1 mg) ethylene glycol-bis(β-aminoethyl ether)-N,N,N',N'-tetraacetic acid, 10 mM (51 mg) MgCl2, and 1.25 M (3 mL of 10 M) NaOH in a 50-mL tube, mix with 15 mL distilled water, and dissolve by using a vortex. Check the pH (should be 6.9). If pH > 6.9, discard the buffer and remake a fresh lot.
- Prepare 5x sample buffer with reducing agent and dye.
- Mix 300 µL (60 mM) of 1 M Tris-HCl (pH 6.8), 2.5 mL (25%) of 50% glycerol, 1 mL (2%) of 10% sodium dodecyl sulfate (SDS), and 1.2 mL distilled water to make up 5 mL of 5x SDS sample buffer. Store at −20 °C.
NOTE: Because glycerol is viscous, measuring 1.25 mL glycerol is difficult. One mL of 100% glycerol weighs 1.26 g. Thus, weigh 1.575 g of 100% glycerol (which equals 1.25 mL of 100% or 2.5 mL of 50% glycerol) in a 15 mL tube first; mix well with the other components.
- Mix 300 µL (60 mM) of 1 M Tris-HCl (pH 6.8), 2.5 mL (25%) of 50% glycerol, 1 mL (2%) of 10% sodium dodecyl sulfate (SDS), and 1.2 mL distilled water to make up 5 mL of 5x SDS sample buffer. Store at −20 °C.
2. Cell Culture, Treatment with Curcumin or LiCl Treatment, and Examination of Protein Expression
- Add ~1 x 106 HCT 116 cells into 100 mm tissue-culture dishes containing the Minimum Essential Media (MEM) supplemented with 10% fetal bovine serum (FBS) and 1% penicillin-streptomycin. After one day of culturing, cells will reach 60-70% confluence.
NOTE: The number of plates needed depends on the number of treatments described below. - When cells reach ~65% confluence (approximated using microscopy), remove the MEM supplemented medium and add serum-free MEM with 5 µM, 10 µM, and 30 µM curcumin or 25 mM, 50 mM, and 100 mM LiCl. Incubate at 37 °C for 24 h in a humidified atmosphere containing 5% CO2.
- 24 h after treatment, wash the cells with 1 mL ice-cold phosphate-buffered saline (PBS), and scrape the cells using a cell scraper. Transfer the scraped cells into 1.5 mL centrifuge tubes and centrifuge for 4 min at 1,800 x g at 4 °C to obtain cell pellets.
- Lyse the cells by suspending the pellets in 100 µL of complete RIPA buffer at 4 °C for 20 min while regularly tapping the tubes. Sonicate the samples briefly.
- Centrifuge the cell homogenates in a benchtop centrifuge at 22,570 x g for 20 min at 4 °C. Transfer the supernatants to other labeled tubes using a pipette.
- Measure the protein concentration in the supernatants by the Bradford assay45 using commercial protein-assay kits.
- Prepare samples of equal protein concentration (10 µg protein/13 µL sample) of cell lysates with 4X SDS gel-loading buffer. Prepared 4x SDS gel-loading buffer fresh containing 400 mM dithiothreitol (DTT).
NOTE: At this stage, samples can be stored at −20 °C if needed. - Incubate the samples on a heat block at 100 °C for 5 min. Mix the samples by using a vortex and wait to cool them for ~10-15 min.
- Assemble an electrophoresis system.
- Load 10 µg protein (13 µL sample) per well on a 10% SDS-polyacrylamide gel for electrophoresis (SDS-PAGE). Load the molecular-weight ladder onto the gel to one lane.
NOTE: As electrophoresis starts, the protein ladder will resolve into protein bands of apparent molecular weights. Use these bands to estimate the molecular weights of the unknown protein bands. - After loading the samples, connect the positive and negative electrodes of the electrophoresis system to a power source to maintain a constant voltage. Initially, start at 70 V for 20 min to move the protein samples from the stacking gel into the resolving gel. Then, increase the voltage to 125 V for approximately 70-120 min until samples and protein ladder reach the end of the gel.
- After completion of electrophoresis, transfer the gel to a polyvinylidene difluoride (PVDF) membrane using a wet electroblotting system. Transfer for ~100 min at 100 V. Block the membrane in 4% bovine serum albumin (BSA) blocking buffer for 90 min at room temperature of around 25 °C.
- Load 10 µg protein (13 µL sample) per well on a 10% SDS-polyacrylamide gel for electrophoresis (SDS-PAGE). Load the molecular-weight ladder onto the gel to one lane.
- Mark the blot by cutting it on the side with the molecular-weight ladder. Use a transparent plastic sheet and a sharp cutter for cutting the blot. Prepare the primary-antibody solutions (anti-tau at 1:5,000; anti-phospho-tau at 1:4,000) and incubate the blot in this solution at 4 °C overnight.
- After overnight incubation, wash the blot for 7 min four times in phosphate-buffered saline-Tween-20 (PBST) solution.
- Prepare the relevant secondary-antibody solutions (goat anti-rabbit or anti-mouse IgG at 1:5,000), and incubate the blot in this solution for 90 min at room temperature of around 25 °C. Wash in PBST four times, 7 min each.
- Develop the blot using a chemiluminescence kit according to the manufacturer's recommendations. Cover the blot using a transparent plastic wrap. Acquire images by a chemiluminescence imaging system for chemiluminescence with relevant software.
3. Phosphatase Assay
- Treat the cell lysates (from step 2.5) with alkaline phosphatase in the alkaline phosphatase buffer.
- For both control and treated samples, prepare 20 µL samples containing 20 µg total protein. Add the volume of cell lysates that contains 20 µg total protein, followed by 2 µL alkaline phosphatase buffer and 10 µL alkaline phosphatase. Add distilled water to make up 20 µL.
- Incubate the samples at 37 °C for 1 h. Stop the reaction by adding ethylenediaminetetraacetic acid (EDTA) at a final concentration of 50 mM, or by adding sodium orthovanadate (Na3VO4) at a final concentration of 10 mM. The reaction can also be stopped by heating at 75 °C for 5 min.
- Before the incubation of samples with phosphatase finishes, prepare samples of the same concentration without adding phosphatase for comparison with phosphatase-treated samples.
- Add the freshly prepared 4X SDS gel-loading buffer containing 400 mM DTT.
- Incubate the samples on a heat block at 100 °C for 5 min. Mix the samples using a vortex. Cool at room temperature for ~ 10-15 min.
- Assemble an electrophoresis system for running a 10% polyacrylamide gel by SDS-PAGE.
- Load 10 µg protein (13 µL sample) per well on a 10% polyacrylamide gel. Load the molecular-weight ladder.
- After loading the sample, connect the positive and negative electrodes of the electrophoresis system to a power source to maintain a constant voltage. Initially, start at 70 V for 20 min to move the protein samples from the stacking gel into the resolving gel. Then, increase the voltage to 125 V and run the gel for approximately 70-120 min until samples and protein ladder reach the end of the gel.
- After completion of electrophoresis, transfer the gel onto a PVDF membrane using a wet electroblotting system. Transfer for ~100 min at 100 V.
- Mark the blot by making a small cut on the side the molecular-weight ladder. Use a transparent plastic sheet and a sharp cutter for cutting the blot.
- Block the membrane in 4% BSA blocking buffer for 90 min at room temperature.
- Incubate the blot in primary-antibody solution (anti-tau at 1:5,000) at 4 °C overnight. Wash the blot in PBST four times, for 7 min each.
- Prepare the relevant secondary-antibody solution (goat anti-mouse IgG at 1:5,000), and incubate the blot for 90 min at room temperature. Wash in PBST four times, for 7 min each.
- Develop the blot using a chemiluminescence kit according to the manufacturer's recommendations. Cover the blot within a transparent plastic wrap. Acquire images by a chemiluminescence imaging system for chemiluminescence with relevant software.
4. Microtubule-binding Assay
- For the microtubule binding assay, repeat steps 2.1-2.6.
- Prepare 1X (2 mL) PEM buffer from 10X PEM buffer stored at 4 °C by adding 20 µM (40 µL) paclitaxel and 1 mM (20 µL) GTP. Take the microtubule (MT) stock from −80 °C freezer and the E. coli tau working stock from −20 °C freezer.
- Prepare samples as per Table 1.
- Incubate at 37 °C for 30 min. Ultracentrifuge at 25 °C for 60 min at 100,000 x g.
- Transfer 120 µL of supernatants containing unbound tau, to clean and labeled tubes.
- Add 120 µL (same volume as supernatant) of 5X sample buffer to the pellet containing bound tau and mix thoroughly. Transfer the solution to clean labeled tubes and mix thoroughly.
- Measure the protein concentration (see step 2.6).
NOTE: While preparing samples, use the volume of solution (step 4.6) for preparing both the pellet and supernatant samples. - Prepare samples of equivalent protein concentration and add freshly prepared 4x SDS gel-loading buffer containing DTT (400 mM).
NOTE: Samples can be stored at −20 °C at this stage. - Repeat steps 3.5-3.10.
| Sample | Name | Microtubule needed | Main Protein needed | PEM-GTP-PTX | ||||
| 1 | HCT 116-Control (6.21 μg/μl) | 2 μl | 9.66 μl (60 μg) | 108.34 μl | ||||
| 2 | HCT 116-Curcumin 10 μM (4.81 μg/μl) | 2 μl | 16.63 μl (80 μg ) | 101.37 μl | ||||
| 3 | HCT 116-Curcumin 20 μM (3.28 μg/μl) | 2 μl | 30.49 μl (100 μg) | 87.51 μl | ||||
| 4 | HCT 116-LiCl 25 mM (5.43 μg/μl) | 2 μl | 18.42 μl (100 μg) | 99.58 μl | ||||
| 5 | E. coli tau | 2 μl | 1 μl tau-352 | 117 μl | ||||
| 6 | MT Only | 2 μl | X | 118 μl | ||||
| 120 μl each | ||||||||
Table 1: Sample preparation for microtubule-binding assay.
5. Localization and Expression of Tau after Treatment of Cells with Curcumin
- Clean a coverslip using 70% ethanol and dry it using a laboratory tissue. Insert a single coverslip in each well of a labeled 6-well tissue-culture plate. Place the plate on a biological safety cabinet and switch on a UV light for at least 3 h.
- Subculture the cells and seed them into the relevant wells of the 6-well plate at 2.5 x 105 cells/well in recommended culture medium.
- After ~24 h, examine the cells using an inverted microscope by using both the 10X and 40X objectives to check for cellular morphological changes. Record photos if needed.
- Rinse the cells twice using PBS. Fix the cells in 3.7% formaldehyde in a 37 °C incubator in the dark.
NOTE: Fixation by formaldehyde at room temperature works well, too. Wear appropriate personal protective equipment when handling formaldehyde. - Wash the cells in PBS. Fix cells in ice-cold methanol at −20 °C for 15 min. Permeabilize the cells by incubating them in 3% BSA and 0.1% Triton X-100 in PBS on ice for 10 min. Wash the cells with PBS.
- Incubate the cells in blocking buffer (3% BSA and 0.1% Tween-20 in PBS solution) for 1 h at room temperature.
NOTE: Incubation for 2 h at 4 °C works well, too. - Prepare the primary-antibody (anti-tau at 1:200) solution in 3% BSA and 0.1% Tween-20 in PBS (e.g., 2 µL tau-13 antibody in 0.4 mL buffer).
- Cut small pieces of a PVDF membrane so that the pieces fit properly within each well of the 6-well plate; soak them in water for 5 min. Place the cut PVDF in each well.
- Add 60 µL of primary antibody solution to the cut PVDF pieces in each well. Place the coverslips such that the cells can touch the primary-antibody solution. Incubate at 4 °C in a dark, humid chamber overnight. Wash in PBS four times.
- Prepare the secondary-antibody solution (fluorescein-conjugated 594 anti-mouse IgG at 1:400) in 3% BSA and 0.1% Tween-20 in PBS.
- Cut small pieces of a PVDF membrane so that the pieces fit properly within each well of the 6-well plate, and soak them in water for 5 min. Place the cut PVDF in each well.
- Add 80 µL of the secondary-antibody solution to each of the PVDF pieces in the 6-well plate. Place the coverslip such that the cells can touch the secondary-antibody solution. Incubate in a dark, humid chamber at room temperature for 2 h. Wash with PBS four times.
- Mount samples in the mounting medium with 4',6-diamidino-2-phenylindole (DAPI) and fix the coverslips on glass slides.
- Add one drop of the mounting medium with DAPI on glass slides. Remove the coverslips from each well and place them on the glass slides containing the mounting medium with DAPI. Ensure that the surface of each coverslip containing stained cells touches the mounting medium on the corresponding glass slide.
- Apply nail polish all around each coverslip to seal and fix them airtight on the glass slides. If needed, do this step twice.
- Incubate for 1.5 h at room temperature in a dark chamber.
- Examine the slides using a confocal microscope by using immersion oil on the coverslip in a dark room.
Representative Results
Expression of total tau and phospho-tau was examined after treating the cells with different concentrations of curcumin or LiCl (Figure 1). Treatment of cells with the three different concentrations of curcumin decreased tau expression levels; however, phospho-tau expression increased upon treatment with low concentration of curcumin but decreased upon treating cells with higher curcumin concentrations. Anti-phospho-tau (Ser396) was used for detection of phospho-tau. Levels of both total tau and phospho-tau decreased upon treatment of the cells with the three different concentrations of LiCl (Figure 1). Previous research had shown that tau expression levels vary in different cancer types and at different sites of the same cancer types. Previous data on colorectal cancer showed that tau was expressed in two cell lines (HCT 116 and SW480) of colorectal cancer that were also phosphorylated19. Phospho-tau levels in cells treated with 5 µM curcumin were higher than those in untreated cells. Phospho-tau levels were higher than total tau in cells treated with the same concentration of curcumin. Treatment of cells with 10 µM curcumin decreased phospho-tau levels compared with untreated cells but phospho-tau expression was still more than total tau expression levels. Treatment of cells with 30 µM curcumin lowered phospho-tau expression compared with phospho-tau in untreated cells and total tau levels in the same treated cells.
This manuscript established an easy protocol for assessing the phosphorylation status of tau by a phosphatase assay (Figure 2). Following curcumin treatment, overall tau phosphorylation did not change significantly and phosphorylation at specific amino acid residues was significant (Figure 1). Overall tau phosphorylation was stopped in cells treated with LiCl as compared with untreated cells. Phosphatase-treated samples electrophoresed faster than untreated samples, verifying that untreated samples were more hyperphosphorylated than phosphatase-treated samples. Curcumin-treated cells showed nearly the same results, indicating that treatment of colorectal cancer cell lines did not reduce tau phosphorylation as shown in Figure 1. Both phosphatase-treated and untreated samples electrophoresed at nearly the same range in samples of cells treated with LiCl, indicating that tau phosphorylation in these cells was reduced (Figure 2). Here, high concentrations (20 µM or 30 µM) of curcumin-treated samples were taken to compare overall phosphorylation status, as low concentration treatment showed higher site-specific phosphorylation revealed by specific phospho-tau (S396) antibody.
Moreover, in this lab, the microtubule binding assay of cell samples was established successfully using tau-352 as a positive control and only MT as a negative control (Figure 3). For both curcumin and LiCl treatment, microtubule-binding activity was inhibited, as demonstrated by the microtubule binding assay. In this experiment, curcumin treatment did not show microtubule binding capabilities but inhibited the binding similar to that in previous studies46,47, whereas it was effective to inhibit site-specific tau phosphorylation at higher concentration. In Figure 1, 10 µM curcumin treatment resulted in minimal expression of phospho-tau compared with control but higher expression than total tau. However, microtubule-binding capacity of colorectal cancer tau after curcumin treatment as well as low concentration of LiCl treatment was decreased in the untreated sample. Site-specific tau phosphorylation effects microtubule binding and self-aggregation48. Tau phosphorylation at proline-rich region impeded microtubule-binding properties whereas C-terminal region increased these properties, and both regions along with MT-binding region lessened its binding properties by about 70% and disordered the microtubules48. Some other factors as well as other site-specific phosphorylation of tau might be involved for this microtubule destabilization of colorectal cancer tau treated with curcumin or LiCl.
A straightforward protocol using small amounts of primary and secondary antibodies enabled localization of tau in colorectal cancer cell lines following curcumin treatment (Figure 4). Results showed that tau had translocated to the nucleus following curcumin treatment, a finding similar to earlier studies reporting that nuclear tau is a key player in neuronal DNA protection in neurodegenerative diseases such as Alzheimer's disease49,50.
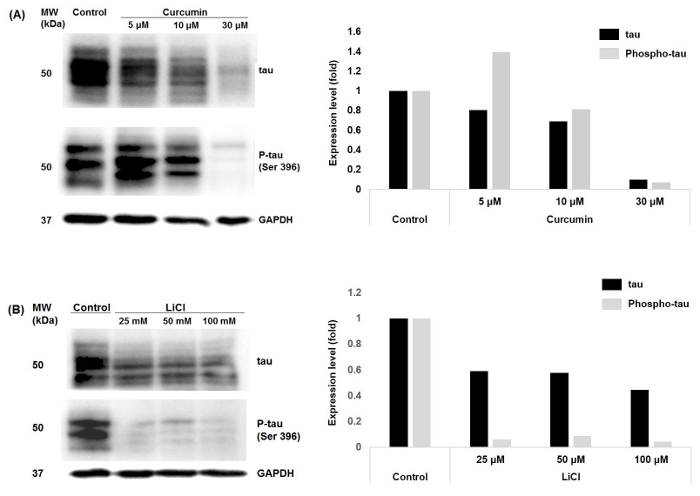
Figure 1: Tau and phospho-tau expression in colorectal cancer cells following curcumin or LiCl treatment. Samples extracted from control cells or cells treated for 24 h with three different concentrations of (A) curcumin and (B) LiCl were resolved on 10% polyacrylamide gels by SDS-PAGE and probed with anti-tau or anti-phospho-tau antibody. Densitometry analyses of the Western blot results are presented on the right panel. Please click here to view a larger version of this figure.
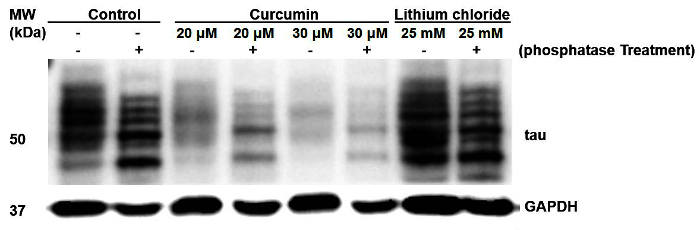
Figure 2: Overall phosphorylation of tau in untreated or differentially treated cell samples detected by the phosphatase assay. Odd lanes show control cell extracts, whereas even lanes show phosphatase treatment of curcumin-treated or LiCl-treated samples. Phosphatase treatment made the tau electrophoretic mobility faster than untreated samples, which contained phosphorylated tau. Please click here to view a larger version of this figure.
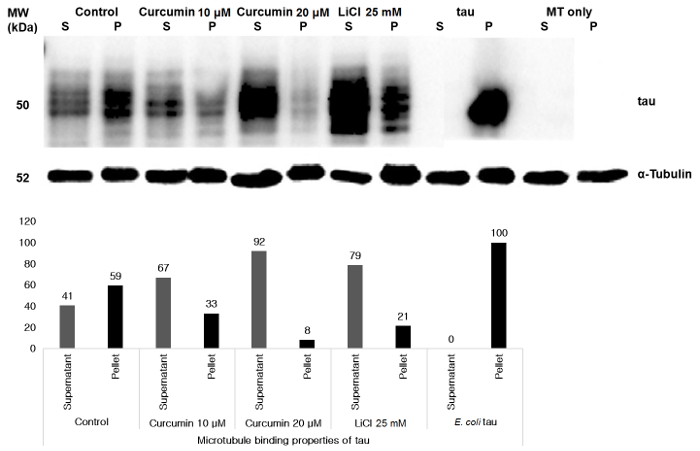
Figure 3: Microtubule binding of tau in colorectal cancer cells detected by the microtubule-binding assay. Control HCT 116 cell samples, curcumin-treated, or LiCl-treated cell samples and E. coli tau were incubated with microtubules as detailed in protocol section 4. Equivalent amounts of supernatant (S) and pellet (P) fractions were immunoblotted with an anti-tau antibody. Negative control lanes containing only MT were run to confirm that MT did not contain any bound endogenous tau. Lower panel shows densitometry analyses of Western blots of individual samples enabling comparison between supernatant (unbound tau) and pellet (bound tau) fractions. Please click here to view a larger version of this figure.
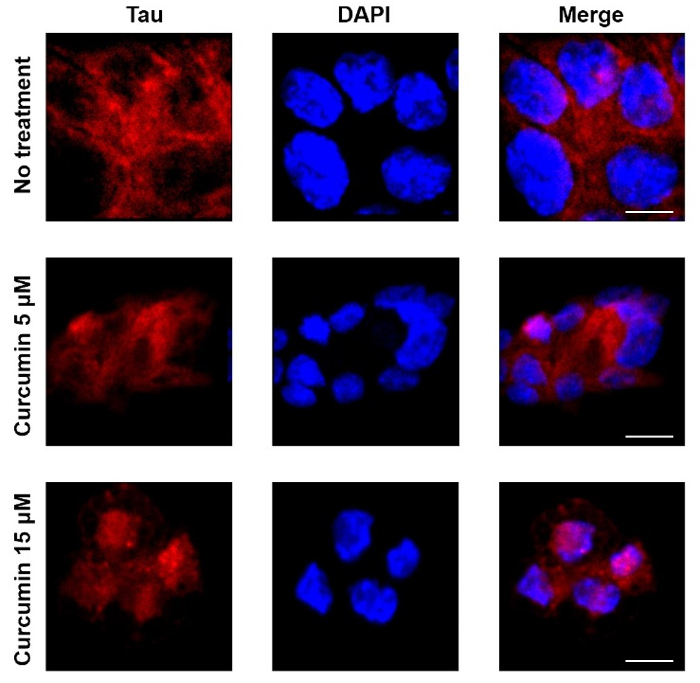
Figure 4: Tau protein localization examined by confocal microscopy.
Tau localized peripherally to the nucleolus in colorectal cancer cells. Left panels show tau localization detected using the anti-tau monoclonal antibody whereas middle panels show nucleus staining by DAPI. Representative examples of treated cells showing tau translocation into the nucleus are also shown. Control cells showed tau mainly around and outside the nuclei, whereas tau in treated cells localized also inside the nuclei. Scale bar = 20 µm. Please click here to view a larger version of this figure.
Discussion
This manuscript established different procedural conditions for detecting total tau and phosphorylated tau in colorectal cancer cells treated with curcumin and LiCl. To assess the overall phosphorylation status of tau in protein samples, a phosphatase assay was described. This assay can potentially be used to examine the phosphorylation status of any protein.
This assay is based on the principle that phosphorylated protein moves slower than its non-phosphorylated state. Alkaline phosphatase and alkaline phosphatase buffer are used in this protocol. After adding the assay components to the cell lysates, samples should be incubated for a specific optimal duration at a specific temperature. After incubation, samples should be boiled in the SDS sample buffer to stop the reaction. Previously, different experimental protocols may have been used to assess the binding of tau to microtubules. The microtubule-binding assay presented here is easy to perform while including both positive and negative controls to provide quality assurance using supernatant and pellet fractions. The MT-only negative control was used to verify that MT does not contain any bound endogenous tau. In addition, pure human tau-352, a microtubule-binding tau was used as the positive control. To separate the microtubule-binding fraction (pellet) from the non-binding fraction (supernatant) ultra-speed centrifugation was used; this procedure can be a limitation because such an ultracentrifuge is expensive and not widely available. In addition, because low quantities of samples are used, long, thin centrifuge tubes with adaptors are needed for use in the ultracentrifuge rotor. Though it is possible to re-use such tubes, single-use is advisable to avoid cross-contamination. Finally, an advantage of the tau-localization protocol is that only small quantities of primary and secondary antibodies are needed. After fixation, permeabilization, and blocking of the cells adherent to coverslips, a small drop of antibody was deposited on a small piece of PVDF, which was then placed inside the wells of a 6-well plate. The coverslips were kept such that the antibody could access the cells. By using this protocol, the amount of antibodies used can be minimized.
Some precautions should be kept in mind to ensure reliable and quantifiable results. Firstly, strict aseptic techniques should be used to avoid contamination in cell cultures and cell extracts. The complete RIPA lysis buffer should be prepared fresh. In the phosphatase assay, it is important to boil the samples for 3 min and start SDS-PAGE immediately after incubation of phosphatase-treated and untreated samples. Tau-352 should be divided into small aliquots and kept on ice after removal from the −20 °C freezer and deposited back into the freezer immediately after use. After removal from the −80 °C, MT stocks should be kept on ice if reused within 72 h; otherwise, keep them at room temperature. The PEM buffer should be prepared as a 10x concentrated solution because the 1x buffer needs to be freshly made when GTP and paclitaxel are added.
Tau functions are regulated by the extent of its phosphorylation. Tau hyperphosphorylation does not occur in normal adult brain tau similar to tau-352, which was used as positive control in the microtubule-binding assay. However, tau hyperphosphorylation occurs in neurodegenerative diseases. This protocol and subsequent results demonstrate that human colorectal cancer cell lines also carry phosphorylated tau similarly to that in Alzheimer's disease brains. Treatment with high-dose curcumin and especially LiCl can minimize tau phosphorylation. Thus, a good correlation between neurodegenerative diseases, such as Alzheimer's disease, and colorectal cancer may exist in regards to tau hyperphosphorylation, and curcumin or LiCl can be used to treat both colorectal cancer and Alzheimer's disease. Lastly, studying tau phosphorylation and tau microtubule binding is significantly relevant not only for neurodegenerative diseases but also for some chemotherapeutics because agents that modify tau microtubule binding are dynamically studied as cancer therapeutics51. The protocols presented here will potentially help the discovery and development of new therapeutic agents to treat different tauopathies and cancers.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This research was performed as part of the project titled 'Development and industrialization of high value cosmetic raw materials from marine microalgae', funded by the Ministry of Oceans and Fisheries, Korea, and was supported by an intramural grant (2Z04930) from KIST Gangneung Institute of Natural Products.
Materials
| HCT 116 cell | ATCC | CCL-247 | |
| MEM (EBSS) | Hyclone | SH30024.01 | |
| Fetal Bovine Serum (FBS) | ThermoFisher (Gibco) | 16000044 | Store at -20 °C |
| penicillin-streptomycin | Hyclone | SV30010 | |
| Trypsin-EDTA solution | WelGene | LS 015-01 | |
| 100 mm dish | Corning | 430161 | |
| 6 well plate | Corning | Coster 3516 | |
| Anti-Tau 13 antibody | abcam | ab19030 | |
| Dithiothreitol (DTT) | Roche | 10 708 984 001 | Storage Temperature 2–8 °C |
| Microlitre Centrifuges | Hettich Zentrifugen | MIKRO 200 R | |
| Paclitaxel | Sigma-Aldrich | T1912 | Storage Temperature 2–8 °C |
| Curcumin | Sigma-Aldrich (Fluka) | 78246 | Storage Temperature 2–8 °C |
| Microtubules (MT) | Cytoskeleton | MT001 | Store at 4 °C (desiccated) |
| Mounting Medium with DAPI | Vector Laboratories | H-1200 | Store at 4 °C in the dark |
| Sodium hydroxide | Sigma | 72068 | |
| Magnesium Chloride | Sigma-Aldrich | M2670 | |
| GTP | Sigma-Aldrich | G8877 | Store at -20 °C |
| DPBS | WelGene | LB 001-02 | |
| Sonic Dismembrator | Fisher Scientific | Model 500 | |
| Ultracentrifuge | Beckman Coulter | Optima L-100 XP | |
| PIPES | Sigma | P1851 | |
| Bovine serum Albumin (BSA) | Sigma | A7906 | |
| Molecular Imager | Bio-Rad | ChemiDoc XRS+ | Store at 4 °C |
| Protein assay dye reagent | Bio-Rad | 500-0006 | |
| α-tubulin (11H10) Rabbit mAb | Cell signalling | 2125 | |
| GAPDH (14C10) Rabbit mAb | Cell signalling | 2118 | |
| Anti-Tau (phospho S396) antibody | abcam | ab109390 | |
| EGTA | Sigma | E3889 | Store at room temperature |
| FastAP Thermosensitive Alkaline Phosphatase | Thermo Scientific | EF0651 | Store at -20 °C |
| PMSF | Sigma | P7626 | Store at room temperature |
| Phosphatase Inhibitor Cocktail | Cell Signalling | 5870 | Store at 4 °C |
| Protease Inhibitor Cocktail | Cell Signalling | 5871 | Store at 4 °C |
| RIPA Buffer | Sigma | R 0278 | Storage Temperature 2–8 °C |
| Tau-352 human | Sigma | T 9950 | Store at -20 °C |
| Triton X-100 | Sigma-Aldrich | X – 100 | Store at around 25 °C |
| PVDF membrane | Bio-Rad | 162-0177 | |
| Goat anti-mouse IgG Secondary Antibody | ThermoFisher | A-11005 | Store at 4 °C in the dark |
| Confocal Microscopy | Leica Microsystem | Leica TCS SP5 | |
| Sodium Dodecyl Sulfate (SDS) | Affymetrix | 75819 | |
| Protein Assay | Bio-Rad | 500-0006 | Store at 4 °C |
References
- Weingarten, M. D., Lockwood, A. H., Hwo, S. Y., Kirschner, M. W. A protein factor essential for microtubule assembly. Proc Natl Acad Sci U S A. 72, 1858-1862 (1975).
- Cambiazo, V., Gonzalez, M., Maccioni, R. B. DMAP-85: a tau-like protein from Drosophila melanogaster larvae. J Neurochem. 64, 1288-1297 (1995).
- Goedert, M., et al. PTL-1, a microtubule-associated protein with tau-like repeats from the nematode Caenorhabditis elegans. J Cell Sci. 109 (Pt 11), 2661-2672 (1996).
- Goedert, M., Spillantini, M. G., Jakes, R., Rutherford, D., Crowther, R. A. Multiple isoforms of human microtubule-associated protein tau: sequences and localization in neurofibrillary tangles of Alzheimer’s disease. Neuron. 3, 519-526 (1989).
- Cleveland, D. W., Hwo, S. Y., Kirschner, M. W. Purification of tau, a microtubule-associated protein that induces assembly of microtubules from purified tubulin. J Mol Biol. 116, 207-225 (1977).
- Fellous, A., Francon, J., Lennon, A. M., Nunez, J. Microtubule assembly in vitro. Purification of assembly-promoting factors. Eur J Biochem. 78, 167-174 (1977).
- Witman, G. B., Cleveland, D. W., Weingarten, M. D., Kirschner, M. W. Tubulin requires tau for growth onto microtubule initiating sites. Proc Natl Acad Sci U S A. 73, 4070-4074 (1976).
- Dixit, R., Ross, J. L., Goldman, Y. E., Holzbaur, E. L. Differential regulation of dynein and kinesin motor proteins by tau. Science. 319, 1086-1089 (2008).
- Harada, A., et al. Altered microtubule organization in small-calibre axons of mice lacking tau protein. Nature. 369, 488-491 (1994).
- Caceres, A., Kosik, K. S. Inhibition of neurite polarity by tau antisense oligonucleotides in primary cerebellar neurons. Nature. 343, 461-463 (1990).
- Binder, L. I., Frankfurter, A., Rebhun, L. I. The distribution of tau in the mammalian central nervous system. J Cell Biol. 101, 1371-1378 (1985).
- Gu, Y. J., Oyama, F., Ihara, Y. tau is widely expressed in rat tissues. J Neurochem. 67, 1235-1244 (1996).
- Kenner, L., et al. Expression of three- and four-repeat tau isoforms in mouse liver. Hepatology. 20, 1086-1089 (1994).
- Souter, S., Lee, G. Microtubule-associated protein tau in human prostate cancer cells: isoforms, phosphorylation, and interactions. J Cell Biochem. 108, 555-564 (2009).
- Sangrajrang, S., et al. Estramustine resistance correlates with tau over-expression in human prostatic carcinoma cells. Int J Cancer. 77, 626-631 (1998).
- Rouzier, R., et al. Microtubule-associated protein tau: a marker of paclitaxel sensitivity in breast cancer. Proc Natl Acad Sci U S A. 102, 8315-8320 (2005).
- Mimori, K., et al. Reduced tau expression in gastric cancer can identify candidates for successful paclitaxel treatment. Brit J Cancer. 94, 1894-1897 (2006).
- Jimeno, A., et al. Development of two novel benzoylphenylurea sulfur analogues and evidence that the microtubule-associated protein tau is predictive of their activity in pancreatic cancer. Mol Cancer Ther. 6, 1509-1516 (2007).
- Huda, M. N., Kim, D. H., Erdene-Ochir, E., Kim, Y. S., Pan, C. H. Expression, phosphorylation, localization, and microtubule binding of tau in colorectal cell lines. Appl Biol Chem. 59, 807-812 (2016).
- Askanas, V., Engel, W. K., Bilak, M., Alvarez, R. B., Selkoe, D. J. Twisted tubulofilaments of inclusion body myositis muscle resemble paired helical filaments of Alzheimer brain and contain hyperphosphorylated tau. The American journal of pathology. 144, 177-187 (1994).
- Buee, L., Bussiere, T., Buee-Scherrer, V., Delacourte, A., Hof, P. R. Tau protein isoforms, phosphorylation and role in neurodegenerative disorders. Brain Res Brain Res Rev. 33, 95-130 (2000).
- Hanger, D. P., Anderton, B. H., Noble, W. Tau phosphorylation: the therapeutic challenge for neurodegenerative disease. Trends Mol Med. 15, 112-119 (2009).
- Sergeant, N., et al. Biochemistry of Tau in Alzheimer’s disease and related neurological disorders. Expert Rev Proteomics. 5, 207-224 (2008).
- Fath, T., Eidenmuller, J., Brandt, R. Tau-mediated cytotoxicity in a pseudohyperphosphorylation model of Alzheimer’s disease. J Neurosci. 22, 9733-9741 (2002).
- Kolarova, M., Garcia-Sierra, F., Bartos, A., Ricny, J., Ripova, D. Structure and pathology of tau protein in Alzheimer disease. Int J Alzheimers Dis. 2012, 731526 (2012).
- Kosik, K. S., Joachim, C. L., Selkoe, D. J. Microtubule-associated protein tau (tau) is a major antigenic component of paired helical filaments in Alzheimer disease. Proc Natl Acad Sci U S A. 83, 4044-4048 (1986).
- Wood, J. G., Mirra, S. S., Pollock, N. J., Binder, L. I. Neurofibrillary tangles of Alzheimer disease share antigenic determinants with the axonal microtubule-associated protein tau (tau). Proc Natl Acad Sci U S A. 83, 4040-4043 (1986).
- Jemal, A., et al. Cancer statistics, 2003. CA Cancer J Clin. 53, 5-26 (2003).
- Patel, V. B., Misra, S., Patel, B. B., Majumdar, A. P. Colorectal cancer: chemopreventive role of curcumin and resveratrol. Nutr Cancer. 62, 958-967 (2010).
- Lim, G. P., et al. The curry spice curcumin reduces oxidative damage and amyloid pathology in an Alzheimer transgenic mouse. J Neurosci. 21, 8370-8377 (2001).
- Venkatesan, N. Curcumin attenuation of acute adriamycin myocardial toxicity in rats. Br J Pharmacol. 124, 425-427 (1998).
- Srinivasan, M. Effect of curcumin on blood sugar as seen in a diabetic subject. Indian J Med Sci. 26, 269-270 (1972).
- Deodhar, S. D., Sethi, R., Srimal, R. C. Preliminary study on antirheumatic activity of curcumin (diferuloyl methane). Indian J Med Res. 71, 632-634 (1980).
- Rao, C. V., Rivenson, A., Simi, B., Reddy, B. S. Chemoprevention of colon carcinogenesis by dietary curcumin, a naturally occurring plant phenolic compound. Cancer Res. 55, 259-266 (1995).
- Araujo, C. C., Leon, L. L. Biological activities of Curcuma longa L. Mem Inst Oswaldo Cruz. 96, 723-728 (2001).
- Lim, T. G., et al. Curcumin suppresses proliferation of colon cancer cells by targeting CDK2. Cancer Prev Res (Phila). 7, 466-474 (2014).
- Ringman, J. M., Frautschy, S. A., Cole, G. M., Masterman, D. L., Cummings, J. L. A potential role of the curry spice curcumin in Alzheimer’s disease. Curr Alzheimer Res. 2, 131-136 (2005).
- Li, H., et al. Lithium chloride suppresses colorectal cancer cell survival and proliferation through ROS/GSK-3beta/NF-kappaB signaling pathway. Oxid Med Cell Longev. , 241864 (2014).
- Forlenza, O. V., De-Paula, V. J., Diniz, B. S. Neuroprotective effects of lithium: implications for the treatment of Alzheimer’s disease and related neurodegenerative disorders. ACS Chem Neurosci. 5, 443-450 (2014).
- Noble, W., et al. Inhibition of glycogen synthase kinase-3 by lithium correlates with reduced tauopathy and degeneration in vivo. Proc Natl Acad Sci U S A. 102, 6990-6995 (2005).
- Perez, M., Hernandez, F., Lim, F., Diaz-Nido, J., Avila, J. Chronic lithium treatment decreases mutant tau protein aggregation in a transgenic mouse model. J Alzheimers Dis. 5, 301-308 (2003).
- Engel, T., Goni-Oliver, P., Lucas, J. J., Avila, J., Hernandez, F. Chronic lithium administration to FTDP-17 tau and GSK-3beta overexpressing mice prevents tau hyperphosphorylation and neurofibrillary tangle formation, but pre-formed neurofibrillary tangles do not revert. J Neurochem. 99, 1445-1455 (2006).
- Caccamo, A., Oddo, S., Tran, L. X., LaFerla, F. M. Lithium reduces tau phosphorylation but not A beta or working memory deficits in a transgenic model with both plaques and tangles. Am J Pathol. 170, 1669-1675 (2007).
- Bradford, M. M. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 72, 248-254 (1976).
- Gupta, K. K., Bharne, S. S., Rathinasamy, K., Naik, N. R., Panda, D. Dietary antioxidant curcumin inhibits microtubule assembly through tubulin binding. FEBS J. 273, 5320-5332 (2006).
- Lee, J. W., Park, S., Kim, S. Y., Um, S. H., Moon, E. Y. Curcumin hampers the antitumor effect of vinblastine via the inhibition of microtubule dynamics and mitochondrial membrane potential in HeLa cervical cancer cells. Phytomedicine. 23, 705-713 (2016).
- Liu, F., et al. Site-specific effects of tau phosphorylation on its microtubule assembly activity and self-aggregation. Eur J Neurosci. 26, 3429-3436 (2007).
- Sultan, A., et al. Nuclear tau, a key player in neuronal DNA protection. J Biol Chem. 286, 4566-4575 (2011).
- Bukar Maina, M., Al-Hilaly, Y. K., Serpell, L. C. Nuclear Tau and Its Potential Role in Alzheimer’s Disease. Biomolecules. 6, 9 (2016).
- Dumontet, C., Jordan, M. A. Microtubule-binding agents: a dynamic field of cancer therapeutics. Nat Rev Drug Discov. 9, 790-803 (2010).

