Isolation of Cerebral Capillaries from Fresh Human Brain Tissue
Summary
Isolated brain capillaries from human brain tissue can be used as a preclinical model to study barrier function under physiological and pathophysiological conditions. Here, we present an optimized protocol to isolate brain capillaries from fresh human brain tissue.
Abstract
Understanding blood-brain barrier function under physiological and pathophysiological conditions is critical for the development of new therapeutic strategies that hold the promise to enhance brain drug delivery, improve brain protection, and treat brain disorders. However, studying the human blood-brain barrier function is challenging. Thus, there is a critical need for appropriate models. In this regard, brain capillaries isolated from human brain tissue represent a unique tool to study barrier function as close to the human in vivo situation as possible. Here, we describe an optimized protocol to isolate capillaries from human brain tissue at a high yield and with consistent quality and purity. Capillaries are isolated from fresh human brain tissue using mechanical homogenization, density-gradient centrifugation, and filtration. After the isolation, the human brain capillaries can be used for various applications including leakage assays, live cell imaging, and immune-based assays to study protein expression and function, enzyme activity, or intracellular signaling. Isolated human brain capillaries are a unique model to elucidate the regulation of the human blood-brain barrier function. This model can provide insights into central nervous system (CNS) pathogenesis, which will help the development of therapeutic strategies for treating CNS disorders.
Introduction
The blood-brain barrier is a tightly controlled interface between the blood and brain that determines what goes into and comes out of the brain. Anatomically, endothelial cells compose the blood-brain barrier and forms a complex, continuous capillary network. Physiologically, this capillary network supplies the brain with oxygen and nutrients while simultaneously disposing of carbon dioxide and metabolic waste products. Importantly, evidence supports that the changes to the barrier contribute to numerous pathologies, including Alzheimer's disease, epilepsy, and stroke1,2,3,4,5,6,7. Brain endothelial cells also serve as a barrier to treatment by blocking drug uptake into the brain, e.g., chemotherapy of glioblastoma multiforme following tumor resection8,9,10. In this regard, isolated human brain capillaries represent a unique ex vivo blood-brain barrier model that closely resembles barrier properties in vivo, which allows for the study of barrier function and dysfunction in health and disease. In this article, we provide a protocol to isolate brain capillaries from human brain at a consistently high capillary quality and yield to study the blood-brain barrier.
In 1969, Siakotos et al.11 were the first to report the isolation of brain capillaries from bovine and human brain tissue using density gradient centrifugation and glass bead column separation. Later, Goldstein et al.12 improved this method by adding multiple filtration steps to decrease the amount of tissue needed to study brain capillaries isolated from rats, while maintaining the metabolic activity of glucose transport. Since then, researchers optimized the capillary isolation procedure numerous times, improving the method and brain capillary model with each iteration13,14,15. For example, Pardridge et al.16 isolated bovine capillaries using enzymatic digestion rather than mechanical homogenization, and then subsequently passed a capillary suspension through a 210 µm mesh filter and a glass bead column. These modifications improved the trypan blue exclusion stain of isolated brain capillaries, and thus, increased endothelial cell viability. In the early 1990s, Dallaire et al.17 isolated bovine and rat capillaries that were clear of neuronal contamination and maintained metabolic activity of γ-glutamyl transpeptidase (γ-GTase) and alkaline phosphatase. In 2000, Miller et al.18, used isolated rat and porcine brain capillaries in combination with confocal microscopy to show the accumulation of transport substrates into the lumen of capillaries. Subsequently, our laboratory has continued to optimize the brain capillary isolation procedure and we have established transport assays to determine P-glycoprotein (P-gp)19,20,21, breast cancer resistance protein (BCRP)22,23, and multi-drug resistance protein 2 (Mrp2)24 transport activity. In 2004, we published two reports where we used isolated rat brain capillaries to investigate various signaling pathways. In Hartz et al.21, we found that the peptide endothelin-1 rapidly and reversibly reduced P-gp transport function in brain capillaries by acting through the endothelin receptor B (ETB) receptor, nitric oxide synthase (NOS), and protein kinase C (PKC). In Bauer et al.19, we demonstrated expression of the nuclear receptor pregnane X receptor (PXR) and showed PXR-modulation of P-gp expression and transport function in brain capillaries. In experiments with transgenic humanized PXR mice, we expanded this line of research and showed in vivo tightening of the barrier by upregulating P-gp through hPXR activation25. In 2010, Hartz et al.26 used this approach to restore P-gp protein expression and transport activity in transgenic human amyloid precursor protein (hAPP) mice that overexpress hAPP. Moreover, restoring P-gp in hAPP mice significantly reduced amyloid beta (Aβ)40and Aβ42brain levels.
In addition to studying signaling pathways, isolated brain capillaries can be used to determine changes in capillary permeability which we refer to as capillary leakage. In particular, the Texas Red leakage assay is used to assess leakage of the fluorescent dye Texas Red from the capillary lumen over time and these data are then used to analyze leakage rates. Increased capillary leakage rates compared to those from control capillaries indicate changes in the physical integrity of the blood-brain barrier2. This is valuable because there are numerous disease states associated with barrier disruption, e.g., epilepsy, multiple sclerosis, Alzheimer's disease, and traumatic brain injury27,28,29,30. Other groups have also utilized isolated capillaries to discern signaling pathways that regulate protein expression and transport activity of proteins31,32,33,34,35,36,37. Finally, we have continued to optimize this method for the isolation of human brain capillaries and, recently, we showed increased P-gp expression at the human blood-brain barrier in patients with epilepsy compared to seizure-free control individuals38. Taken together, these developments demonstrate that isolated brain capillaries can serve as a versatile model to study barrier function.
Various in vivo, ex vivo, and in vitro blood-brain barrier models have been used in basic research and industrial drug screening, mainly with the goal of testing drug delivery to the brain39,40,41,42,43,44. In addition to isolated ex vivo brain capillaries, current blood-brain barrier models include in silico models, in vitro cell culture of isolated brain capillary endothelial cells or immortalized cell lines from various species, in vitro culture of human pluripotent stem cells (hPSC) that differentiate into brain capillary endothelial cells, and microfluidic models on a chip.
In silico models are most commonly used in drug development for selecting drug candidates based on predicted absorption, distribution, metabolism, and excretion (ADME) properties. Methods such as quantitative structure-property relationship (QSPR) models and quantitative structure-activity relationship (QSAR) models are popular methods used in high-throughput screening of libraries to predict brain penetration of drug candidates45,46. These models are useful to screen molecules for barrier penetration properties.
Betz et al.47 established monolayers of cultured brain capillary endothelial cells as an in vitro blood-brain barrier model system. In vitro cell culture models using fresh tissue or immortalized endothelial cell lines such as human cerebral microvessel endothelial cells (hCMECs) can be another high-throughput screening tool for brain penetration or mechanistic studies. However, brain capillary endothelial cell culture models lack the physiologic shear stress of blood flow inside the capillary lumen, are limited in overall biologic complexity, and undergo changes in expression and localization of important barrier components such as tight junction proteins, surface receptors, transporters, enzymes, and ion channels48,49,50. Conversely, endothelial monolayers derived from hPSCs, have low sucrose permeability compared to hCMEC/D3 cultures and contain polarized expression of some blood-brain barrier transporters, adhesion molecules, and tight junctions51,52. However, these cells are also subject to changing properties in the culture, and the system must be validated for its recapitulation of in vivo barrier properties52.
Newer trends in blood-brain barrier research include utilizing 3D tissue culture systems to create artificial capillaries, using the organ-on-chip technology to generate microfluidic devices, or utilizing the hollow fiber technology53,54,55. Artificial capillaries, however, have significantly larger diameters (100–200 µm) than brain capillaries (3–7 µm). Hence, the shear forces in vitro do not fully resemble the in vivo situation. This is addressed in "blood-brain-barrier-on-a-chip" microfluidic devices, where artificial membranes form "blood" and "brain" compartments and fluids are pumped through these devices generating microfluidic shear forces. Similarly, co-cultures of endothelial cells in various combinations with astrocytes and vascular smooth muscle cells have also been used with the hollow fiber technology to recreate rheological parameters present under in vivo conditions56,57,58. However, it is unclear how well this model reflects other properties of the blood-brain barrier such as transport, metabolism, signaling, and others. These artificial capillary and chip models are suitable for high-throughput screening of drugs, but the cells used to generate these models are also subject to change during culture.
Frozen and fixed brain slices or primary brain capillary endothelial cell cultures are additional models that can be used tostudy the human microvasculature5,59,60,61. For example, immunohistochemistry of fixed brain tissue is used to determine protein localization and expression in healthy compared to diseased tissue.
In addition to tissue slices and the in vitro models described above, freshly isolated brain capillaries can be utilized to study blood-brain barrier function. Limitations of this isolated capillary model include the difficulty to obtain fresh human brain tissue, absence of astrocytes and neurons, and a relatively time-consuming isolation process. An advantage of the isolated brain capillary model is that this model closely resembles the in vivo situation and, therefore, can be used to characterize barrier function and dysfunction. Importantly, it can also be used to discern signaling mechanisms using a multitude of assays and molecular techniques3,19,62,63.
Our laboratory has access to both fresh and frozen human brain tissue through the Sanders-Brown Center on Aging (IRB #B15-2602-M)64. In this context, autopsies follow a standard protocol, brains are obtained in <4 h, and all procedures conform to NIH Biospecimen Best Practice Guidelines65. Given this unique access to human brain tissue, we established and optimized a protocol to isolate brain capillaries from human brain tissue that results in a high yield of intact, viable human brain capillaries. Two common endpoints of interest are to determine the protein expression and activity. In this regard, we and others have established various assays that can be used with isolated brain capillaries to study protein expression and activity levels. These assays include Western blotting, Simple Western assay, enzyme-linked immunosorbent assay (ELISA), reverse transcription polymerase chain reaction (RT-PCR), quantitative polymerase chain reaction (qPCR), zymography, transport activity assays, and capillary leakage assays. These assays allow researchers to study changes in barrier function in human pathologic conditions, determine pathways that govern protein expression and activity, and identify pharmacologic targets for the treatment of blood-brain barrier associated diseases.
Taken together, freshly isolated brain capillaries can serve as a robust and reproducible model of the blood-brain barrier. Especially, this model can be combined with many different assays to determine a wide array of endpoints to study barrier function.
Protocol
The information below is based on current safety and regulatory standards at the University of Kentucky, Lexington, KY, USA. As a safety precaution, refer to the institution's biological safety program and the most current regulations and recommendations before working with human tissue.
CAUTION: Human tissue can be a source of blood-borne pathogens, including human immunodeficiency virus (HIV), hepatitis B virus (HBV), hepatitis C virus (HCV), and others. Working with human tissue poses the risk of infection from blood-borne pathogens. Therefore, certain regulatory and safety considerations are imperative when working with human tissue to protect laboratory personnel. Working with human tissue in the US requires a biosafety level 2 laboratory as well as safety precautions and training in accordance with NIH Section IV-B-7, OSHA Act of 1970 Clause 5(a)(1) and the user's institutional biological safety program. In general, Institutional Biosafety Committee and/or Institutional Review Board approval must be obtained prior to conducting any research involving human materials (tissue, body fluids). The training is required for all personnel working with human materials and includes basic laboratory safety training, e.g., Chemical Hygiene and Laboratory Safety, as well as specific training on biological safety, hazardous waste, and human blood-borne pathogens. All personnel working with human materials are highly recommended to obtain Hepatitis B vaccinations, prior to working with human materials. Personnel are required to wear specific personal protective equipment while working with human materials, e.g., a cuffed lab coat and a face shield, and wear gloves at all times. All work is performed in a biosafety cabinet (class 2). All equipment that comes in contact with human materials and any waste from human materials is handled appropriately to prevent contamination and/or infection of personnel. All equipment and surfaces are cleaned with 10% bleach and 75% ethanol following each procedure involving human materials. A spill with human materials must be immediately cleaned up. Glassware is autoclaved after each use. Waste, including unfixed human tissue, is collected in a labeled biohazard waste bag and autoclaved. Sharps are collected in a puncture- and leak-proof container labeled as biohazardous. All waste from human materials is disposed according to the institution's biological safety regulations.
NOTE: Our laboratory obtains fresh frontal cortex samples from deceased individuals through the Sanders-Brown Center on Aging (IRB #B15-2602-M). Inclusion criteria are: enrollment in the UK-ADC longitudinal autopsy cohort study and a Post-Mortem Interval (PMI) ≤4 h64. Autopsies follow a standard protocol and all procedures conform to NIH Biospecimen Best Practice Guidelines65. A short PMI of less than 4 h is of highest importance to ensure capillary viability after isolation. Both fresh and frozen tissue can be used. If freezing is necessary, freshly obtained human brain tissue should be shock-frozen in liquid nitrogen and stored at -80 °C. Fresh or thawed tissue should be stored in isolation buffer (see below) and processed quickly. We find that 10 g of fresh human tissue yields about 100 mg of brain capillaries (wet weight).
1. Setup
- Buffer preparation
NOTE: The volume of buffer needed depends on the amount of tissue. All buffer volumes in the following protocol are based on 10 g of human brain cortex tissue.- L Isolation Buffer: Use 1.5 L of Dulbecco's phosphate-buffered saline (DPBS; 2.7 mM KCl, 1.47 mM KH2PO4, 136.9 mM NaCl, 8.1 mM Na2HPO4, 0.9 mM CaCl2, 0.49 mM MgCl2) and supplement with 5 mM D-glucose (1.35 g) and 1 mM sodium pyruvate (0.165 g). After adding the glucose and pyruvate, adjust to pH 7.4 with sodium hydroxide. Cool and store the buffer to 4 °C prior to use.
- Bovine Serum Albumin (BSA): Add 10 g of BSA powder to 1 L of isolation buffer to a final BSA concentration of 1%. Stir slowly to avoid bubbles, adjust to pH 7.4, and store at 4 °C overnight. Immediately prior to use, gently stir; avoid forming bubbles to avoid albumin denaturation.
- density gradient medium: Weigh 18 g of density gradient medium into a glass bottle and add a magnetic stir bar. Add 60 mL of isolation buffer and shake vigorously for 5 min until all powder is suspended. Store overnight at 4 °C to allow the density gradient medium to dissolve. Stir for 10 min right before use.
- Store all buffers at 4 °C; keep all tools and buffers on ice during the entire isolation procedure. Stir all buffers before use.
- Experimental setup
- Mount the pestle of the Potter-Elvehjem tissue grinder onto the electronic overhead stirrer. Place the Potter-Elvehjem tissue grinder and the Dounce homogenizer with pestle on ice under the hood. Prepare a 300 µm filter mesh (5 x 5 cm2), fold it to a cone, and insert and attach it to a 50 mL Falcon tube with tape (Figure 1A).
- Place connecting rings and cell strain filters (pore size: 30 µm) on 50 mL Falcon tubes. Prepare biohazardous waste bags. Place all required equipment in the biosafety cabinet (see Table of Materials).
2. Brain Sample Preparation
NOTE: Figure 1A shows the workflow chart of the entire isolation procedure described below. Human brain tissue can stem from any part of the cortex and can be used fresh or frozen. Frozen brain tissue can be thawed at room temperature (no buffer; ~30 min for 10 g). To achieve comparable results, the brain tissue should be obtained from the same brain region for each experiment. This protocol is optimized for fresh (PMI <4 h) human cerebral cortex that has not been frozen.
- Preparation of human brain tissue: Document the weight of the brain tissue. All numbers in the following protocol are appropriate for 10 g of fresh human brain tissue. Place the brain tissue in a 100 mm Petri dish. Carefully remove all the meninges with forceps. Use a scalpel to cut off the white matter.
- Mincing of the human brain tissue: Carefully cut up the brain tissue and mince it with a scalpel. Mince for about 5 min (2–3 mm pieces). Transfer the brain tissue to the Potter-Elvehjem tissue grinder. Add 30 mL of isolation buffer.
NOTE: The minced tissue pieces are difficult to see since the brain tissue turns into mush through the mincing process.
3. Homogenization
- Potter-Elvehjem tissue grinder (clearance: 150–230 µm): Homogenize each sample with 100 strokes at a homogenizer speed of 50 rpm. Document the time every 25 strokes and the total time needed for 100 strokes. See Table 1 for a proposed homogenization protocol; the total time for homogenizing 10 g of human frontal cortex is about 22 min. Do not stir in air to prevent bubbles.
- Dounce homogenizer (clearance: 80–130 µm): Transfer the homogenate to a Dounce homogenizer on ice. Homogenize the suspension with 20 strokes (~6 s/stroke, total of ~2 min). Avoid bubbles.
4. Centrifugation
- Distribute the brain homogenate equally into four 50 mL centrifugation tubes and document the total volume of the homogenate. Distribute 50 mL of density gradient buffer into the centrifugation tubes (12.5 mL per tube). Use 10 mL of isolation buffer to rinse the pestle and homogenizer, and distribute into the four centrifugation tubes (~2.5 mL per tube).
- Tightly close the centrifuge tubes with caps. Mix the homogenate, density gradient medium, and buffer by vigorously shaking the tubes. Centrifuge at 5,800 x g for 15 min at 4 °C (fixed angle rotor); select a medium deceleration speed to keep the pellet attached to the tube. Discard the supernatant and resuspend each pellet in 2 mL of 1% BSA.
5. Filtration
NOTE: To separate the capillaries from red blood cells and other cell debris, several filtration steps are necessary.
- 300 µm mesh: After re-suspending the pellet, filter the suspension through the 300 µm mesh. Capillaries are filtered through the mesh, whereas larger vessels and larger brain debris remain on the mesh. Carefully wash the mesh with up to 50 mL of 1% BSA. Discard the mesh.
NOTE: This filtration step clears the capillary suspension from any larger vessels or chunks of brain debris. - 30 µM cell strain filter
NOTE: This filtration step separates capillaries from red blood cells and other brain debris.- Distribute the capillary filtrate from step 6.1 over the five 30 µm cell strain filters (about 10 mL of capillary filtrate per cell strain filter). Capillaries are held back by this filter, whereas red blood cells, other single cells, and small brain debris pass through the filter and are collected in the filtrate.
- Wash each filter with 25 mL of 1% BSA. Afterwards, pour all filtrates over the sixth filter to increase the yield. Wash each filter with 50 mL of 1% BSA; keep the cell strain filters with containing the capillaries and discard the filtrate.
6. Capillary Collection
- Turn the filters upside down and wash the capillaries with 50 mL of 1% BSA for each filter into 50 mL tubes. Gently apply pressure with the pipet tip of a 5 mL pipettor and move it across the filter to wash off the brain capillaries.
- Make sure to wash off all brain capillaries, especially from the rim of the filter. Avoid bubbles since this makes the filtration process more difficult and increases the chance of capillary loss.
7. Washing
- After collecting the capillaries, centrifuge all samples at 1,500 x g for 3 min at 4 °C (swinging bucket rotor). Remove the supernatant and re-suspend the pellet in approximately 3 mL of isolation buffer. Combine all resuspended pellets from one sample in a 15 mL conical tube and fill it with isolation buffer. Centrifuge again at 1,500 x g for 3 min at 4 °C and wash two more times.
- Document the capillary purity with a microscope (100X magnification) and camera (Figure 1B).
NOTE: The brain capillary yield from 10 g of human brain tissue is usually about 100 mg. The isolated brain capillaries can now be used for experiments, processed (e.g., lysate, membrane isolation), or be flash-frozen and stored at -80 °C in cryotubes for a minimum of 6–12 months (avoid multiple freeze-thaw cycles).
Representative Results
The isolations from human brain tissue yield a suspension enriched in human brain capillaries (Figure 1B) with small amounts of larger vessels, red blood cells, other single cells, and some cell debris. Some capillaries are branched, and, in some, red blood cells are entrapped in the capillary lumens. The typical capillary has a 3–7 µm diameter and is approximately 100-200 µm long with open lumens; most capillary ends are collapsed. Using confocal microscopy, isolated human brain capillaries reveal a tubular, intact structure and morphology. Figure 2A shows a representative transmitted light image of a human brain capillary with an attached pericyte and a red blood cell in the lumen. All of the findings regarding diameter, size, and morphology are in accordance with previous reports on the structure of isolated brain capillaries12,17,18. The isolated human brain capillary in Figure 2B was immunostained for P-gp (green) using C219 as the primary antibody (1 µg/mL); nuclei were counterstained with DAPI (1 µg/mL).
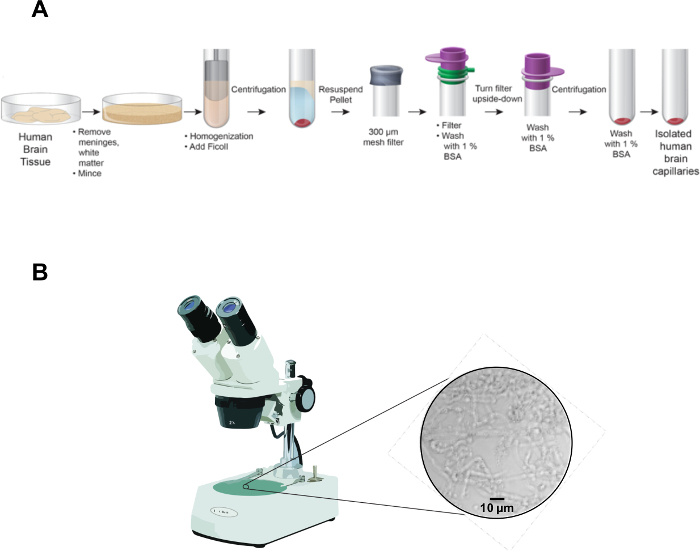
Figure 1: Flowchart for capillary isolation. (A) The pictogram illustrates major steps of the procedure to isolate brain capillaries from fresh human tissue. (B) The picture shows isolated human brain capillaries under a light microscope directly after isolation (100X magnification). Please click here to view a larger version of this figure.
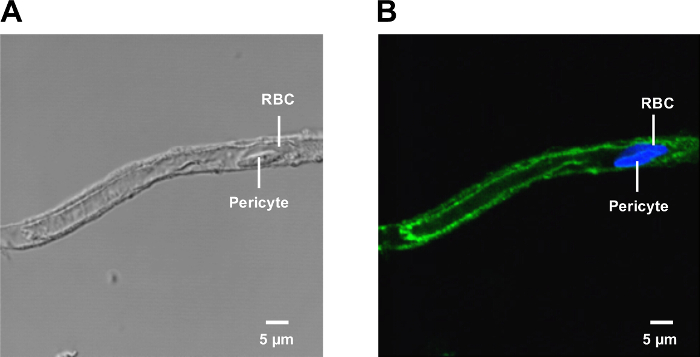
Figure 2: Isolated human brain capillary. (A) A transmitted light image of an isolated human brain capillary. (B) The confocal microscope image shows an isolated human brain capillary immunostained for P-gp (green; C219 1 µg/mL); nuclei were counterstained with DAPI (blue; 1 µg/mL). Please click here to view a larger version of this figure.
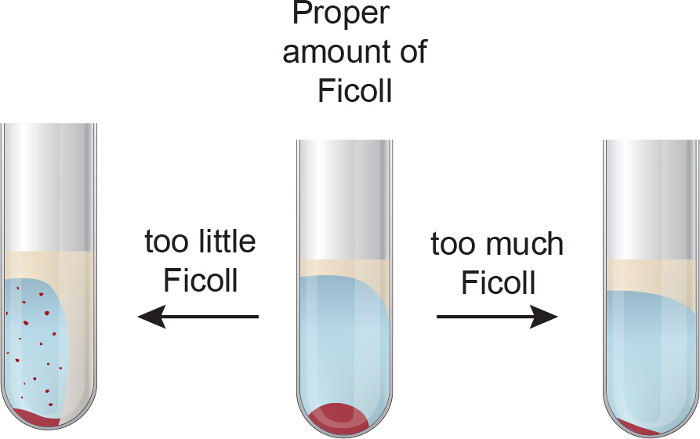
Figure 3: Troubleshooting density centrifugation. The pictogram shows the preparation after the density gradient centrifugation. It highlights the effects of too much and too little density gradient medium and how this affects the separation and the resulting capillary pellet. Please click here to view a larger version of this figure.
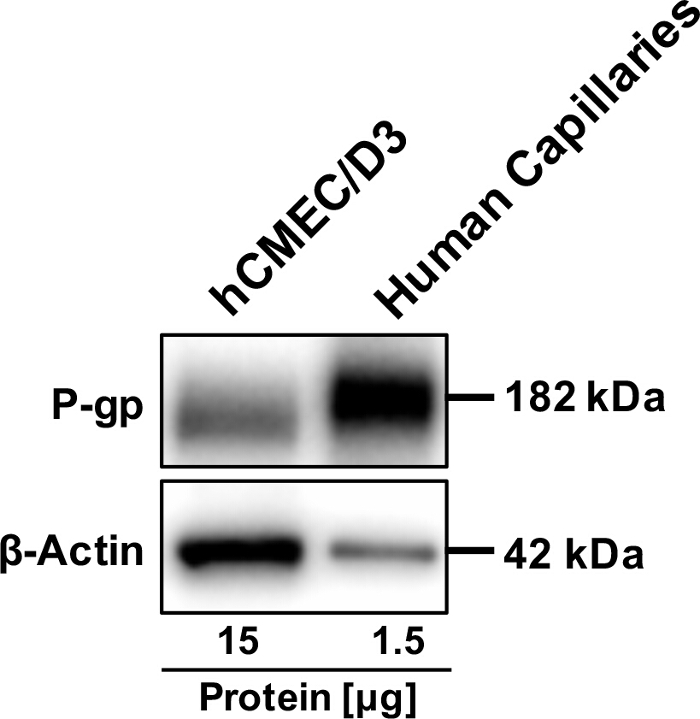
Figure 4: P-gp protein expression in isolated human brain capillaries. The Western blot shows strong bands for P-gp (1 µg/mL) in isolated human capillaries compared to hCMECD3 cells. β-Actin was used as a loading control (1 µg/µL). Please click here to view a larger version of this figure.
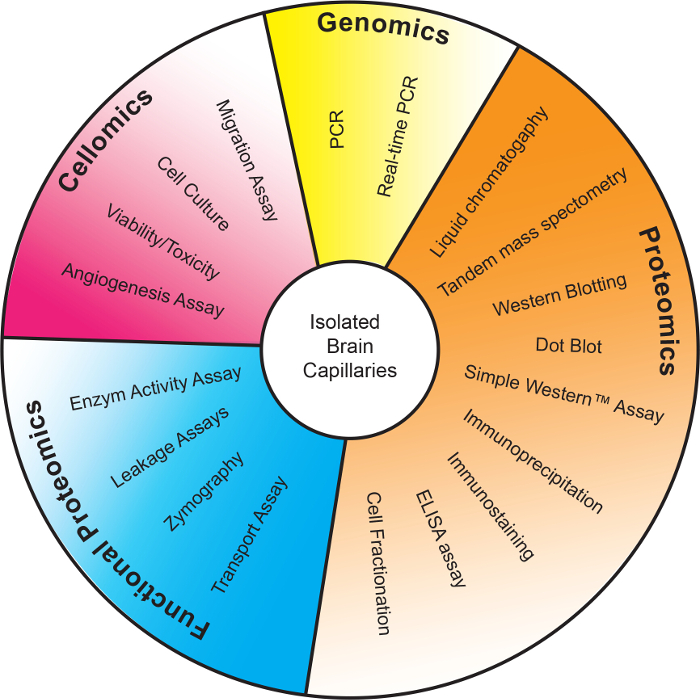
Figure 5: Applications for isolated human brain capillaries. An overview of the most common applications for isolated brain capillaries published in the literature. Isolated capillaries have been used for: 1) Genomics85,86, 2) Proteomics3,38,87,88,89,90,91,92,94,95,96, 3) Functional Proteomics2,38, and 4) Cellomics82,83,84,97,98,99. Please click here to view a larger version of this figure.
| Strokes | Time [min] |
| 1–25 | 7–7.5 |
| 26–50 | 5–5.5 |
| 51–75 | 5–5.5 |
| 76–100 | 5–5.5 |
| Total Time: | 22–24 min |
Table 1: Homogenization protocol. The homogenization protocol for the Potter-Elvehjem tissue grinder to homogenize 10 g of human frontal cortex at a homogenization speed of 50 rpm. Note that the first several strokes require additional time to homogenize the minced tissue. After this initial homogenization, each stroke is 12 s in duration (6 s for downward movement, 6 s for upward movement). Thus, after the initial homogenization, 5 strokes can be accomplished in 1 min, or 25 strokes in 5 min.
| Problem | Potential Cause | Solution |
| No Capillary Pellet | 1) Incorrect Ficoll concentration | 1) Adjust Ficoll concentration |
| 2) Incorrect centrifugation speed | 2) Adjust centrifugation speed | |
| 3) Incorrect acceleration and/or deceleration speed | 3) Adjust acceleration and/or deceleration speed | |
| Low Capillary Yield | 1) Meninges blocking filtration steps | 1) Remove ALL meninges prior to filtration |
| 2) Too many capillaries lost during isolation procedure | 2) Calculate buffer concentration correctly, rinse pipette tips | |
| 3) Washing capillaries off PluriStrainer filters was insufficient | 3) Turn filters over and carefully inspect for capillaries (use microscope) | |
| 4) Excess bubbles during resuspensions | 4) Pipette slowly to avoid bubbles | |
| Non-Viable Capillaries | 1) Extended post-mortem interval | 1) Reduce interval if possible or use snap-frozen brains |
| 2) Using frozen tissue for the isolation | 2) Use fresh tissue | |
| 3) Time of isolation procedure too long | 3) Optimize workflow | |
| 4) Equipment/buffers were not kept on ice during the isolation procedure | 4) Keep equipment and buffers on ice during the isolation |
Table 2: Troubleshooting of common problems. A list of the most common errors and problems that occur during the isolation procedure and how they can be resolved.
Discussion
The present protocol describes the isolation of intact and viable human brain capillaries from fresh tissue. In this section, we discuss in detail the following: 1) modifications to the protocol, 2) troubleshooting of common errors, 3) limitations of the technique, 4) the significance of the model with respect to existing and alternative blood-brain barrier models, and 5) potential applications for isolated human brain capillaries.
The protocol described here is optimized for 10 g of fresh human frontal cortex tissue. However, it is relatively simple to modify this procedure for: 1) more or less than 10 g of tissue, 2) frozen brain tissue, or 3) brain tissue from a brain region other than the frontal cortex. First, with more or less than 10 g of brain tissue, the necessary volume of the buffers can simply be scaled up or down to the available amount of tissue. Thus, if only 5 g of brain tissue is available, the volume of the buffers should be reduced by half. Second, we describe a capillary isolation that used fresh brain tissue, but frozen tissue may be used if fresh tissue is unavailable38. Third, we used fresh brain tissue taken from the frontal cortex, but capillaries may be isolated from other cortical brain regions if there is enough available tissue. It is also possible to isolate capillaries from non-cortical brain regions (e.g., white matter), but these regions have a different cell composition and capillary density 66,67,68. Thus, using tissue from a different brain region would likely require the protocol to be adjusted (e.g., buffer volume, gradient medium density, centrifugation speed, and/or number of filtration steps).
The capillary isolation procedure, while not complex per se, is sensitive to small perturbations or alterations in the protocol. Modifications may result in a diminished capillary yield or reduced capillary viability. Table 2 outlines the most common errors and problems that are encountered during the isolation and lists tips to avoid these errors and solutions for troubleshooting if they occur. The most common problem associated with the procedure is a low capillary yield. The loss of capillaries is often the cumulative sum of small losses at each step and is due to small deviations across the procedure. A critical step in which a large amount of capillaries may be lost is the density centrifugation. An incorrect concentration in the buffer results in an incorrect density to separate the capillaries from cellular debris that reduces the volume of the capillary pellet. Figure 3 shows the consequences of too little or too much density gradient medium in the centrifugation step relative to brain homogenate. Adjusting to the correct the concentration may solve this problem. Note that the acceleration and deceleration speed of the centrifuge can also affect the formation of the brain capillary pellet. Capillaries may also be lost during steps 6–7 if part of the capillary material sticks to the pipette tips. This issue can be addressed by thoroughly rinsing each pipet tip before changing it. During step 7, washing off the capillaries from the cell strain filter may be incomplete and/or capillaries may stick to the rim of the filter. This can be avoided by checking the filter under the microscope followed by additional washing steps. Losing capillaries during each step of the isolation procedure can result in a negligible capillary pellet or not enough capillary material for further processing and experimentation.
Isolating brain capillaries from fresh human tissue represents a unique blood-brain barrier model that closely resembles the in vivo situation. However, several limitations of the technique exist. One challenge is the availability of fresh human tissue. As the optimal PMI is ≤4 h, brain tissue collected at a significantly longer PMI will not be fresh enough for some downstream applications. In some cases, it may be difficult to obtain tissue amounts that are large enough for multiple experimental groups, thereby restricting downstream applications. Thus, isolating fresh capillaries from rodent19, canine69, bovine42, or porcine70 brain tissue may be more suitable to model the blood-brain barrier. Factors that determine the variability of human brain tissue such as age, sex, ethnicity, disease state, medication history, brain region of sample, and PMI should be taken into consideration when interpreting and publishing data. On an experimental level it is important to note that isolated capillaries still include pericytes, but astrocytic endfeet are removed by the procedure44. It needs to be taken into consideration that the model presented here serves as an ex vivo model of the blood-brain barrier (i.e., capillary endothelial cells) but not as a model of the neurovascular unit.
Working with any human tissue always presents an inherent safety risk and researchers must take appropriate precautions during the isolation procedure to avoid infection. Specifically, in the U.S., work with human tissue requires designated laboratory space that is BSL 2-certified and includes a biosafety cabinet (class A2). In addition, staff must use personal protective equipment (i.e., lab coat, gloves, and face shield) and designated equipment for work with human tissue and implement biohazardous waste handling. Implementing these safety measures is time-consuming, cost-intensive, and increases the difficulty of the procedure, especially for inexperienced laboratory personnel.
The blood-brain barrier is highly conserved among organisms with a well-defined CNS71. Modeling the human blood-brain barrier is difficult because there is complex neurovascular coupling among the cells of the neurovascular unit. An adult human brain has been estimated to have in average about 86 billion neurons and it is thought that almost every neuron has its own capillary in the vicinity to ensure proper supply with oxygen and nutrients72,73. Capillary endothelial cells constitute the largest surface area of the blood-brain interface (12–18 m2 for a healthy adult human). Tight junctions represent an impediment to a wide array of pharmacotherapeutics by blocking paracellular diffusion of solutes. In addition, numerous studies describe barrier dysfunction in neurodegenerative disorders, e.g., Alzheimer's disease74, stroke75, epilepsy38,76, multiple sclerosis77, and traumatic brain injury28,78. Thus, it is imperative to establish models that closely represent the human blood-brain barrier and allow for a better understanding of barrier function in health and disease.
Numerous in vitro cell culture models of the blood-brain barrier exist; for expert reviews on the subject see 41,49,51,69,79,80. Briefly, both freshly isolated brain capillary endothelial cells for primary culture and immortalized brain capillary endothelial cell lines are available. Primary cultures of cerebral microvessel endothelial cells are mostly used from mouse, rat, pig, and cow. However, primary cell cultures are labor-intensive since cells must be freshly isolated. Immortalized brain capillary endothelial cell lines are available from mouse, rat, and human and are less labor-intensive because they can be passaged for longer-term use. However, even immortalized cell lines have a limit on how often they can be passaged before losing their endothelial characteristics. Both primary cells as well as immortalized cells lines are often cultured on plates to model the brain capillary endothelium and measure the barrier permeability and drug transport across the cell monolayer, thereby mimicking blood-to-brain transport41,81,82. The culture media in these models may also be modified or supplemented with astrocytes, pericytes, or other physiologically relevant factors like cAMP41,83,84.
The advantage of immortalized cell lines is their relatively easy access and availability. While cultured endothelial cells can reach confluence, they lose endothelial cell properties as they grow side-by-side in a monolayer. For example, cultured hCMECs display reduced expression of transporters like P-gp, tight junction proteins, and display variable permeability to xenobiotics41. Figure 4 shows a Western blot for P-gp protein expression in hCMEC/D3 cells compared to freshly isolated human capillaries. Despite a 10-fold lower amount of total protein, the signal for P-gp is stronger in isolated human capillaries compared to hCMEC/D3 cells. This indicates that hCMEC/D3 cells lost a significant amount of P-gp protein expression in culture. Moreover, differences in culture media, environment, and equipment affect key measures of barrier integrity, i.e., TEER measurements in Transwell plate assays. Some of these issues can be overcome by utilizing the isolated brain capillary model that more closely represents the human blood-brain barrier in vivo.
Isolated brain capillaries have been used for a wide range of studies, including genomics, proteomics, functional proteomics, and cellomics studies (Figure 5). In addition, many techniques and methods exist to analyze isolated brain capillaries within each of these fields. Notably, the experimental techniques shown in Figure 5 can be used on brain capillaries isolated from a number of sources, including human, bovine, rodent, and porcine tissue, which may facilitate translational research. For example, Li et al.85 studied the genomics of the blood-brain barrier using suppression subtractive hybridization by purifying mRNA isolated from rat brain capillaries. Additionally, Ott et al.86 used RT-PCR and qRT-PCR to study the regulation of P-gp by PXR. Many proteomic studies utilize Western blotting3, Dot Blot analysis87, Simple Western assays3,38, ELISA88,89, immunoprecipitation3, and immunostaining3,90,91. To discern transporter trafficking in the brain endothelium, McCaffrey et al.92 used subcellular fractionation of isolated brain capillaries. Sánchez del Pino et al.93used isolated bovine endothelial membrane vesicles to discern transporter location and transport direction across the blood-brain barrier. In other proteomic studies, researchers used liquid chromatography and tandem mass spectrometry to quantify transporter proteins94,95,96. Functional proteomic studies have utilized transporter and leakage assays2,38. Hartz et al.2 used zymography to determine enzyme activity in isolated brain capillaries. In addition, vast cellomic research using cell culture has generated numerous endothelial cell lines and models of the blood-brain barrier82,83,84. With these models, common assays used include migration assays97,98, viability and toxicity assays99, and angiogenesis assays98.
Isolated brain capillaries allow for accurate characterization of protein expression and activity and description of signaling pathways at the blood-brain barrier. This is due, in part, to the capillary content of the brain, which is only approximately 1% (v/v). Thus, using whole brain homogenate or brain slices as a substitute for purified capillary endothelial cells will most likely result in a poor signal-to-noise ratio24. In addition, after isolation, brain capillaries are viable for at least 6 h (unpublished data from mouse and rat), which allows studies to discern specific signaling pathways. It is recommended to include a control group from the same preparation.
Representative and translational models of the blood-brain barrier, such as the isolated capillary model discussed in this report, are needed to study barrier function in health and disease. Here we present a protocol to obtain isolated human brain capillaries at a good yield and high quality that can serve as an ex vivo model of the blood-brain barrier. Isolated capillaries retain their original structure and function, which allows using them for a number of post-isolation molecular, biochemical, and physiological assays. Care should be taken when handling human tissue samples, preferably in a BSL 2 or higher setting.
Disclosures
The authors have nothing to disclose.
Acknowledgements
We thank and acknowledge Dr. Peter Nelson and Sonya Anderson at the UK-ADC Brain Tissue Bank for providing all human brain tissue samples (NIH grant number: P30 AG028383 from the National Institute on Aging). We thank Matt Hazzard and Tom Dolan, Information Technology Services, Academic Technology and Faculty Engagement, University of Kentucky for graphical assistance. This project was supported by grant number 1R01NS079507 from the National Institute of Neurological Disorders and Stroke (to B.B.) and by grant number 1R01AG039621 from the National Institute on Aging (to A.M.S.H.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke or the National Institute on Aging. The authors declare no competing financial interests.
Materials
| Personal Protective Equipment (PPE) | |||
| Diamond Grip Plus Latex Gloves, Microflex Medium | VWR, Radnor, PA, USA | 32916-636 | PPE |
| Disposable Protective Labcoats | VWR, Radnor, PA, USA | 470146-214 | PPE; due to the nature of the human source material, the use of a disposable lab coat is recommended |
| Face Shield, disposable | Thermo Fisher Scientific, Pittsburgh, PA, USA | 19460102 | PPE; due to the nature of the human source material, the use of a disposable face shield is recommended |
| Safety Materials | |||
| Clavies High-Temperature Autoclave Bags 8X12 | Thermo Fisher Scientific, Pittsburgh, PA, USA | 01-815-6 | |
| Versi Dry Bench Paper 18" x 20" | Thermo Fisher Scientific, Pittsburgh, PA, USA | 14-206-32 | to cover working areas |
| VWR Sharps Container Systems | Thermo Fisher Scientific, Pittsburgh, PA, USA | 75800-272 | for used scalpels |
| Bleach 8.2% Clorox Germicidal 64 oz | UK Supply Center, Lexington, KY, USA | 323775 | |
| Equipment | |||
| 4°C Refrigerator | Thermo Fisher Scientific, Pittsburgh, PA, USA | 13-986-148 | |
| Accume BASIC AB15 pH Meter | Thermo Fisher Scientific, Pittsburgh, PA, USA | AB15 | |
| Heidolph RZR 2102 Control | Heidolph, Elk Grove Village, IL, USA | 501-21024-01-3 | |
| Sorvall LEGEND XTR Centrifuge | Thermo Fisher Scientific, Pittsburgh, PA, USA | 75004521 | |
| Leica L2 Dissecting Microscope | Leica Microsystems Inc, Buffalo Grove IL, USA | used to remove meninges | |
| POLYTRON PT2500 Homogenizer | Kinematica AG, Luzern, Switzerland | 9158168 | |
| Scale P-403 | Denver Instrument, Bohemia, NY, USA | 0191392 | |
| Standard mini Stir | Thermo Fisher Scientific, Pittsburgh, PA, USA | 1151050 | |
| Thermo-Flasks Liquid Nitrogen Dewar | Thermal Scientific, Mansfiled, TX, USA | 11-670-4C | used to freeze the tissue? |
| Voyager Pro Analytical Balance | OHAUS, Parsippany, NJ, USA | VP214CN | |
| ZEISS Axiovert Microcope | Carl Zeiss, Inc Thornwood, NY, USA | used to check isolated capillaries | |
| Tools and Glassware | |||
| Finnpipette II Pipette 1-5mL | Thermo Fisher Scientific, Pittsburgh, PA, USA | 21377823T1 | wash capillaries off filter |
| Finnpipette II Pipette 100-1000 µL | Thermo Fisher Scientific, Pittsburgh, PA, USA | 21377821T1 | resuspend pellet in BSA |
| Pipet Boy | Integra, Hudson, NH, USA | 739658 | |
| 50mL Falcon tubes 25/rack – 500/cs | VWR, Radnor, PA, USA | 21008-951 | |
| EISCO Scalpel Blades | Thermo Fisher Scientific, Pittsburgh, PA, USA | S95938C | to mince brain tissue |
| PARAFILM | VWR, Radnor, PA, USA | 52858-000 | to cover beaker and volumetric flask |
| Thermo Scientific Finntip Pipet Tips 5 ml | Thermo Fisher Scientific, Pittsburgh, PA, USA | 21-377-304 | to wash capillaries off filter |
| 60 ml syringe with Luer-Lok | Thermo Fisher Scientific, Pittsburgh, PA, USA | BD309653 | used with connector ring to filter capillaries |
| Scalpel Handle #4 | Fine Science Tools, Foster City, CA, USA | 10060-13 | used for mincing |
| Dumont Forceps #5 | Fine Science Tools, Foster City, CA, USA | 11251-10 | used to remove meninges |
| Potter-Elvehjem Tissue Grinder | Thomas Scientific, Swedesboro, NJ, USA | 3431E25 | 50 ml volume, clearance: 150-230 μm |
| Dounce Homogenizer | VWR, Radnor PA USA | 62400-642 | 15 ml volume, clearance: 80-130 μm |
| Spectra/Mesh Woven Filters (300 µm) | Spectrum Laboratories, Rancho Dominguez, CA, USA | 146424 | Used to filter capillary suspension to remove any meninges that may be left |
| pluriStrainers (pore size: 30 µm) | pluriSelect Life Science, Leipzig, Germany | 43-50030-03 | |
| Connector Ring | pluriSelect Life Science, Leipzig, Germany | 41-50000-03 | reuse multiple time |
| 1 l Volumetric Flask | for preparation of Isolation Buffer | ||
| 1 l Beaker | for preparation of 1% BSA | ||
| Stir Bar | for preparation of 1% BSA and Ficoll® | ||
| Schott Bottle (60 ml) | for preparation of Ficoll® | ||
| Ice Bucket | to keep everything cold | ||
| 100 mm Petri Dish | for mincing of brain tissue | ||
| Tissue Culture Cell Scraper | VWR, Radnor, PA, USA | 89260-222 | to remove supernatant after centrifugation |
| Chemicals | |||
| BSA Fraction V, A-9647 | Sigma-Aldrich, St. Louis, MO, USA | A9647-500g | prepare in DPBS with Ca2+ & Mg2+ the day before. Avoid bubbles during preparation. Store in the refrigerator. Slowly stir for 10 min before use. |
| DPBS with Ca2+ & Mg2+ | Hyclone | SH30264.FS | DPBS – part of the Isolation Buffer |
| Ficoll PM400 | Sigma-Aldrich, St. Louis, MO, USA | F4375 | Exact measurement is important here. Weigh out in bottle with stir bar. Shake vigurously after adding DPBS. Keep in the fridge O/N. It will be clear in the morning. Stir gently for 10-15 min before use. Keep on ice until use. |
| Glucose (D-(+) Dextrose) | Sigma-Aldrich, St. Louis, MO, USA | G7528 | Glucose (D-(+) Dextrose) Concentration: 5 mM |
| Sodium Hydroxide Standard Solution | Sigma-Aldrich, St. Louis, MO, USA | 71474 | to adjust pH of the DPBS |
| Sodium Pyruvate | Sigma-Aldrich, St. Louis, MO, USA | P2256 | Concentration: 1 mM |
References
- Aronica, E., et al. Expression and cellular distribution of multidrug resistance-related proteins in the hippocampus of patients with mesial temporal lobe epilepsy. Epilepsia. 45 (5), 441-451 (2004).
- Hartz, A. M., et al. Amyloid-β contributes to blood-brain barrier leakage in transgenic human amyloid precursor protein mice and in humans with cerebral amyloid angiopathy. Stroke. 43 (2), 514-523 (2012).
- Hartz, A. M., et al. Aβ40 Reduces P-Glycoprotein at the Blood-Brain Barrier through the Ubiquitin-Proteasome Pathway. J Neurosci. 36 (6), 1930-1941 (2016).
- Kassner, A., Merali, Z. Assessment of Blood-Brain Barrier Disruption in Stroke. Stroke. 46 (11), 3310-3315 (2015).
- Lauritzen, F., et al. Monocarboxylate transporter 1 is deficient on microvessels in the human epileptogenic hippocampus. Neurobiol Dis. 41 (2), 577-584 (2011).
- Tishler, D. M., et al. MDR1 gene expression in brain of patients with medically intractable epilepsy. Epilepsia. 36 (1), 1-6 (1995).
- van Assema, D. M., et al. Blood-brain barrier P-glycoprotein function in Alzheimer’s disease. Brain. 135 (Pt 1), 181-189 (2012).
- Oberoi, R. K., et al. Strategies to improve delivery of anticancer drugs across the blood-brain barrier to treat glioblastoma. Neuro Oncol. 18 (1), 27-36 (2016).
- Parrish, K. E., et al. Efflux transporters at the blood-brain barrier limit delivery and efficacy of cyclin-dependent kinase 4/6 inhibitor palbociclib (PD-0332991) in an orthotopic brain tumor model. J Pharmacol Exp Ther. 355 (2), 264-271 (2015).
- Thomas, A. A., Brennan, C. W., DeAngelis, L. M., Omuro, A. M. Emerging therapies for glioblastoma. JAMA Neurol. 71 (11), 1437-1444 (2014).
- Siakotos, A. N., Rouser, G., Fleische, S. Isolation Of Highly Purified Human And Bovine Brain Endothelial Cells And Nuclei And Their Phospholipid Composition. Lipids. 4 (3), 234-239 (1969).
- Goldstein, G. W., Wolinsky, J. S., Csejtey, J., Diamond, I. ISOLATION OF METABOLICALLY ACTIVE CAPILLARIES FROM RAT-BRAIN. Journal of Neurochemistry. 25 (5), 715-717 (1975).
- Joo, F., Karnushina, I. A procedure for the isolation of capillaries from rat brain. Cytobios. 8 (29), 41-48 (1973).
- Joo, F., Rakonczay, Z., Wollemann, M. Camp-Mediated Regulation Of Permeability In Brain Capillaries. Experientia. 31 (5), 582-584 (1975).
- Panula, P., Joo, F., Rechardt, L. EVIDENCE FOR PRESENCE OF VIABLE ENDOTHELIAL CELLS IN CULTURES DERIVED FROM DISSOCIATED RAT-BRAIN. Experientia. 34 (1), 95-97 (1978).
- Pardridge, W. M., Eisenberg, J., Yamada, T. Rapid Sequestration And Degradation Of Somatostatin Analogs By Isolated Brain Microvessels. Journal of Neurochemistry. 44 (4), 1178-1184 (1985).
- Dallaire, L., Tremblay, L., Beliveau, R. Purification And Characterization Of Metabolically Active Capillaries Of The Blood-Brain-Barrier. Biochemical Journal. 276, 745-752 (1991).
- Miller, D. S., et al. Xenobiotic transport across isolated brain microvessels studied by confocal microscopy. Molecular Pharmacology. 58 (6), 1357-1367 (2000).
- Bauer, B., Hartz, A. M., Fricker, G., Miller, D. S. Pregnane X receptor up-regulation of P-glycoprotein expression and transport function at the blood-brain barrier. Mol Pharmacol. 66 (3), 413-419 (2004).
- Bauer, B., Hartz, A. M., Miller, D. S. Tumor necrosis factor alpha and endothelin-1 increase P-glycoprotein expression and transport activity at the blood-brain barrier. Mol Pharmacol. 71 (3), 667-675 (2007).
- Hartz, A. M., Bauer, B., Fricker, G., Miller, D. S. Rapid regulation of P-glycoprotein at the blood-brain barrier by endothelin-1. Mol Pharmacol. 66 (3), 387-394 (2004).
- Hartz, A. M., Madole, E. K., Miller, D. S., Bauer, B. Estrogen receptor beta signaling through phosphatase and tensin homolog/phosphoinositide 3-kinase/Akt/glycogen synthase kinase 3 down-regulates blood-brain barrier breast cancer resistance protein. J Pharmacol Exp Ther. 334 (2), 467-476 (2010).
- Hartz, A. M., Mahringer, A., Miller, D. S., Bauer, B. 17-β-Estradiol: a powerful modulator of blood-brain barrier BCRP activity. J Cereb Blood Flow Metab. 30 (10), 1742-1755 (2010).
- Bauer, B., et al. Coordinated nuclear receptor regulation of the efflux transporter, Mrp2, and the phase-II metabolizing enzyme, GSTpi, at the blood-brain barrier. J Cereb Blood Flow Metab. 28 (6), 1222-1234 (2008).
- Bauer, B., et al. In vivo activation of human pregnane X receptor tightens the blood-brain barrier to methadone through P-glycoprotein up-regulation. Mol Pharmacol. 70 (4), 1212-1219 (2006).
- Hartz, A. M., Miller, D. S., Bauer, B. Restoring blood-brain barrier P-glycoprotein reduces brain amyloid-beta in a mouse model of Alzheimer’s disease. Mol Pharmacol. 77 (5), 715-723 (2010).
- Erickson, M. A., Banks, W. A. Blood-brain barrier dysfunction as a cause and consequence of Alzheimer’s disease. J Cereb Blood Flow Metab. 33 (10), 1500-1513 (2013).
- Marchi, N., et al. Consequences of repeated blood-brain barrier disruption in football players. PLoS One. 8 (3), e56805 (2013).
- Rempe, R. G., Hartz, A. M., Bauer, B. Matrix metalloproteinases in the brain and blood-brain barrier: Versatile breakers and makers. J Cereb Blood Flow Metab. 36 (9), 1481-1507 (2016).
- van Vliet, E. A., et al. Blood-brain barrier leakage may lead to progression of temporal lobe epilepsy. Brain. 130, 521-534 (2007).
- Banks, W. A., et al. Tau Proteins Cross the Blood-Brain Barrier. J Alzheimers Dis. 55 (1), 411-419 (2017).
- Chan, G. N., et al. et al. In vivo induction of P-glycoprotein expression at the mouse blood-brain barrier: an intracerebral microdialysis study. J Neurochem. 127 (3), 342-352 (2013).
- Mesev, E. V., Miller, D. S., Cannon, R. E. Ceramide 1-Phosphate Increases P-Glycoprotein Transport Activity at the Blood-Brain Barrier via Prostaglandin E2 Signaling. Mol Pharmacol. 91 (4), 373-382 (2017).
- Ronaldson, P. T., Demarco, K. M., Sanchez-Covarrubias, L., Solinsky, C. M., Davis, T. P. Transforming growth factor-beta signaling alters substrate permeability and tight junction protein expression at the blood-brain barrier during inflammatory pain. J Cereb Blood Flow Metab. 29 (6), 1084-1098 (2009).
- Seelbach, M. J., Brooks, T. A., Egleton, R. D., Davis, T. P. Peripheral inflammatory hyperalgesia modulates morphine delivery to the brain: a role for P-glycoprotein. J Neurochem. 102 (5), 1677-1690 (2007).
- Sugiyama, D., et al. Functional characterization of rat brain-specific organic anion transporter (Oatp14) at the blood-brain barrier: high affinity transporter for thyroxine. J Biol Chem. 278 (44), 43489-43495 (2003).
- Wang, X., et al. Nrf2 upregulates ATP binding cassette transporter expression and activity at the blood-brain and blood-spinal cord barriers. J Neurosci. 34 (25), 8585-8593 (2014).
- Hartz, A. M., et al. P-gp Protein Expression and Transport Activity in Rodent Seizure Models and Human Epilepsy. Mol Pharm. 14 (4), 999-1011 (2017).
- Pardridge, W. M., Eisenberg, J., Yamada, T. Rapid sequestration and degradation of somatostatin analogues by isolated brain microvessels. J Neurochem. 44 (4), 1178-1184 (1985).
- Goldstein, G. W., Betz, A. L., Bowman, P. D. Use of isolated brain capillaries and cultured endothelial cells to study the blood-brain barrier. Fed Proc. 43 (2), 191-195 (1984).
- Pardridge, W. M., Triguero, D., Yang, J., Cancilla, P. A. Comparison of in vitro and in vivo models of drug transcytosis through the blood-brain barrier. J Pharmacol Exp Ther. 253 (2), 884-891 (1990).
- Audus, K. L., Bartel, R. L., Hidalgo, I. J., Borchardt, R. T. The use of cultured epithelial and endothelial cells for drug transport and metabolism studies. Pharm Res. 7 (5), 435-451 (1990).
- Abbott, N. J., Hughes, C. C., Revest, P. A., Greenwood, J. Development and characterisation of a rat brain capillary endothelial culture: towards an in vitro blood-brain barrier. J Cell Sci. 103 (Pt 1), 23-37 (1992).
- Miller, D. S., et al. Xenobiotic transport across isolated brain microvessels studied by confocal microscopy. Mol Pharmacol. 58 (6), 1357-1367 (2000).
- Dolgikh, E., et al. QSAR Model of Unbound Brain-to-Plasma Partition Coefficient, Kp,uu,brain: Incorporating P-glycoprotein Efflux as a Variable. J Chem Inf Model. 56 (11), 2225-2233 (2016).
- Narayanan, R., Gunturi, S. B. In silico ADME modelling: prediction models for blood-brain barrier permeation using a systematic variable selection method. Bioorg Med Chem. 13 (8), 3017-3028 (2005).
- Betz, A. L., Firth, J. A., Goldstein, G. W. Polarity of the blood-brain barrier: distribution of enzymes between the luminal and antiluminal membranes of brain capillary endothelial cells. Brain Res. 192 (1), 17-28 (1980).
- Cucullo, L., Hossain, M., Puvenna, V., Marchi, N., Janigro, D. The role of shear stress in Blood-Brain Barrier endothelial physiology. BMC Neurosci. 12, 40 (2011).
- He, Y., Yao, Y., Tsirka, S. E., Cao, Y. Cell-culture models of the blood-brain barrier. Stroke. 45 (8), 2514-2526 (2014).
- Urich, E., Lazic, S. E., Molnos, J., Wells, I., Freskgård, P. O. Transcriptional profiling of human brain endothelial cells reveals key properties crucial for predictive in vitro blood-brain barrier models. PLoS One. 7 (5), e38149 (2012).
- Helms, H. C., et al. In vitro models of the blood-brain barrier: An overview of commonly used brain endothelial cell culture models and guidelines for their use. J Cereb Blood Flow Metab. 36 (5), 862-890 (2016).
- Stebbins, M. J., et al. Differentiation and characterization of human pluripotent stem cell-derived brain microvascular endothelial cells. Methods. 101, 93-102 (2016).
- Booth, R., Kim, H. Characterization of a microfluidic in vitro model of the blood-brain barrier (µBBB). Lab Chip. 12 (10), 1784-1792 (2012).
- Brown, J. A., et al. Recreating blood-brain barrier physiology and structure on chip: A novel neurovascular microfluidic bioreactor. Biomicrofluidics. 9 (5), 054124 (2015).
- Griep, L. M., et al. BBB on chip: microfluidic platform to mechanically and biochemically modulate blood-brain barrier function. Biomed Microdevices. 15 (1), 145-150 (2013).
- Cucullo, L., Hossain, M., Tierney, W., Janigro, D. A new dynamic in vitro modular capillaries-venules modular system: cerebrovascular physiology in a box. BMC Neurosci. 14, 18 (2013).
- Neuhaus, W., et al. A novel flow based hollow-fiber blood-brain barrier in vitro model with immortalised cell line PBMEC/C1-2. J Biotechnol. 125 (1), 127-141 (2006).
- Stanness, K. A., et al. A new model of the blood–brain barrier: co-culture of neuronal, endothelial and glial cells under dynamic conditions. Neuroreport. 10 (18), 3725-3731 (1999).
- Ghosh, C., et al. Pattern of P450 expression at the human blood-brain barrier: roles of epileptic condition and laminar flow. Epilepsia. 51 (8), 1408-1417 (2010).
- Jeynes, B., Provias, J. An investigation into the role of P-glycoprotein in Alzheimer’s disease lesion pathogenesis. Neurosci Lett. 487 (3), 389-393 (2011).
- Wijesuriya, H. C., Bullock, J. Y., Faull, R. L., Hladky, S. B., Barrand, M. A. ABC efflux transporters in brain vasculature of Alzheimer’s subjects. Brain Res. 1358, 228-238 (2010).
- Pekcec, A., et al. Targeting prostaglandin E2 EP1 receptors prevents seizure-associated P-glycoprotein up-regulation. J Pharmacol Exp Ther. 330 (3), 939-947 (2009).
- Zibell, G., et al. Prevention of seizure-induced up-regulation of endothelial P-glycoprotein by COX-2 inhibition. Neuropharmacology. 56 (5), 849-855 (2009).
- Nelson, P. T., et al. Clinicopathologic correlations in a large Alzheimer disease center autopsy cohort: neuritic plaques and neurofibrillary tangles "do count" when staging disease severity. J Neuropathol Exp Neurol. 66 (12), 1136-1146 (2007).
- Vaught, J., et al. The ISBER Best Practices: Insight from the Editors of the Third Edition. Biopreserv Biobank. 10 (2), 76-78 (2012).
- Gjedde, A., Kuwabara, H., Hakim, A. M. Reduction of functional capillary density in human brain after stroke. J Cereb Blood Flow Metab. 10 (3), 317-326 (1990).
- Karbowski, J. Scaling of brain metabolism and blood flow in relation to capillary and neural scaling. PLoS One. 6 (10), e26709 (2011).
- Lokkegaard, A., Nyengaard, J. R., West, M. J. Stereological estimates of number and length of capillaries in subdivisions of the human hippocampal region. Hippocampus. 11 (6), 726-740 (2001).
- Gerhart, D. Z., Broderius, M. A., Drewes, L. R. Cultured human and canine endothelial cells from brain microvessels. Brain Res Bull. 21 (5), 785-793 (1988).
- Tontsch, U., Bauer, H. C. ISOLATION, CHARACTERIZATION, AND LONG-TERM CULTIVATION OF PORCINE AND MURINE CEREBRAL CAPILLARY ENDOTHELIAL-CELLS. Microvascular Research. 37 (2), 148-161 (1989).
- Abbott, N. J. Dynamics of CNS barriers: Evolution, differentiation, and modulation. Cellular and Molecular Neurobiology. 25 (1), 5-23 (2005).
- Herculano-Houzel, S., Kaas, J. H., de Oliveira-Souza, R. Corticalization of motor control in humans is a consequence of brain scaling in primate evolution. J Comp Neurol. 524 (3), 448-455 (2016).
- Pardridge, W. M. Molecular biology of the blood-brain barrier. Mol Biotechnol. 30 (1), 57-70 (2005).
- Cirrito, J. R., et al. P-glycoprotein deficiency at the blood-brain barrier increases amyloid-beta deposition in an Alzheimer disease mouse model. J Clin Invest. 115 (11), 3285-3290 (2005).
- Rosenberg, G. A., Estrada, E. Y., Dencoff, J. E. Matrix metalloproteinases and TIMPs are associated with blood-brain barrier opening after reperfusion in rat brain. Stroke. 29 (10), 2189-2195 (1998).
- van Vliet, E. A., et al. Blood-brain barrier leakage may lead to progression of temporal lobe epilepsy. Brain. 130 (Pt 2), 521-534 (2007).
- Kermode, A. G., et al. Breakdown Of The Blood-Brain-Barrier Precedes Symptoms And Other Mri Signs Of New Lesions In Multiple-Sclerosis – Pathogenetic And Clinical Implications. Brain. 113, 1477-1489 (1990).
- Shlosberg, D., Benifla, M., Kaufer, D., Friedman, A. Blood-brain barrier breakdown as a therapeutic target in traumatic brain injury. Nat Rev Neurol. 6 (7), 393-403 (2010).
- Cecchelli, R., et al. Modelling of the blood-brain barrier in drug discovery and development. Nat Rev Drug Discov. 6 (8), 650-661 (2007).
- Wilhelm, I., Fazakas, C., Krizbai, I. A. In vitro models of the blood-brain barrier. Acta Neurobiol Exp (Wars). 71 (1), 113-128 (2011).
- Hatherell, K., Couraud, P. O., Romero, I. A., Weksler, B., Pilkington, G. J. Development of a three-dimensional, all-human in vitro model of the blood-brain barrier using mono-, co-, and tri-cultivation Transwell models. J Neurosci Methods. 199 (2), 223-229 (2011).
- Rubin, L., et al. A cell culture model of the blood-brain barrier. The Journal of cell biology. 115 (6), 1725-1735 (1991).
- Gaillard, P. J., et al. Establishment and functional characterization of an in vitro model of the blood-brain barrier, comprising a co-culture of brain capillary endothelial cells and astrocytes. European journal of pharmaceutical sciences. 12 (3), 215-222 (2001).
- Nakagawa, S., et al. A new blood-brain barrier model using primary rat brain endothelial cells, pericytes and astrocytes. Neurochemistry international. 54 (3), 253-263 (2009).
- Li, J. Y., Boado, R. J., Pardridge, W. M. Blood-brain barrier genomics. Journal of Cerebral Blood Flow & Metabolism. 21 (1), 61-68 (2001).
- Ott, M., Fricker, G., Bauer, B. Pregnane X receptor (PXR) regulates P-glycoprotein at the blood-brain barrier: functional similarities between pig and human PXR. J Pharmacol Exp Ther. 329 (1), 141-149 (2009).
- Méresse, S., Delbart, C., Fruchart, J. C., Cecchelli, R. Low-density lipoprotein receptor on endothelium of brain capillaries. Journal of neurochemistry. 53 (2), 340-345 (1989).
- Hartz, A. M., Bauer, B., Block, M. L., Hong, J. S., Miller, D. S. Diesel exhaust particles induce oxidative stress, proinflammatory signaling, and P-glycoprotein up-regulation at the blood-brain barrier. FASEB J. 22 (8), 2723-2733 (2008).
- Moser, K. V., Reindl, M., Blasig, I., Humpel, C. Brain capillary endothelial cells proliferate in response to NGF, express NGF receptors and secrete NGF after inflammation. Brain research. 1017 (1), 53-60 (2004).
- Carrano, A., et al. ATP-binding cassette transporters P-glycoprotein and breast cancer related protein are reduced in capillary cerebral amyloid angiopathy. Neurobiol Aging. 35 (3), 565-575 (2014).
- Deane, R., et al. RAGE mediates amyloid-beta peptide transport across the blood-brain barrier and accumulation in brain. Nat Med. 9 (7), 907-913 (2003).
- McCaffrey, G., et al. P-glycoprotein trafficking at the blood-brain barrier altered by peripheral inflammatory hyperalgesia. Journal of neurochemistry. 122 (5), 962-975 (2012).
- Sanchez del Pino, M. M., Hawkins, R. A., Peterson, D. R. Biochemical discrimination between luminal and abluminal enzyme and transport activities of the blood-brain barrier. J Biol Chem. 270 (25), 14907-14912 (1995).
- Agarwal, S., et al. Quantitative proteomics of transporter expression in brain capillary endothelial cells isolated from P-glycoprotein (P-gp), breast cancer resistance protein (Bcrp), and P-gp/Bcrp knockout mice. Drug metabolism and disposition. 40 (6), 1164-1169 (2012).
- Kamiie, J., et al. Quantitative atlas of membrane transporter proteins: development and application of a highly sensitive simultaneous LC/MS/MS method combined with novel in-silico peptide selection criteria. Pharmaceutical research. 25 (6), 1469-1483 (2008).
- Uchida, Y., et al. Quantitative targeted absolute proteomics of human blood-brain barrier transporters and receptors. Journal of neurochemistry. 117 (2), 333-345 (2011).
- Lee, B. -. C., Lee, T. -. H., Avraham, S., Avraham, H. K. Involvement of the Chemokine Receptor CXCR4 and Its Ligand Stromal Cell-Derived Factor 1α in Breast Cancer Cell Migration Through Human Brain Microvascular Endothelial Cells. Molecular Cancer Research. 2 (6), 327-338 (2004).
- Zagzag, D., et al. Hypoxia-inducible factor 1 and VEGF upregulate CXCR4 in glioblastoma: implications for angiogenesis and glioma cell invasion. Lab Invest. 86 (12), 1221-1232 (2006).
- Preston, J. E., Hipkiss, A. R., Himsworth, D. T. J., Romero, I. A., Abbott, J. N. Toxic effects of beta-amyloid(25-35) on immortalised rat brain endothelial cell: protection by carnosine, homocarnosine and beta-alanine. Neuroscience Letters. 242 (2), 105-108 (1998).

