Production of High-Titer Infectious Influenza Pseudotyped Particles with Envelope Glycoproteins from Highly Pathogenic H5N1 and Avian H7N9 Viruses
Summary
This protocol describes an experimental process to produce high-titer infectious viral pseudotyped particles (pp) with envelope glycoproteins from two influenza A strains and how to determine their infectivity. This protocol is highly adaptable to develop pps of any other type of enveloped viruses with different envelope glycoproteins.
Abstract
The occasional direct transmission of the highly pathogenic avian influenza A virus H5N1 (HPAI H5N1) and H7N9 to humans and their lethality are serious public health issues and suggest the possibility of an epidemic. However, our molecular understanding of the virus is rudimentary, and it is necessary to study the biological properties of its envelope proteins as therapeutic targets and to develop strategies to control infection. We developed a solid viral pseudotyped particle (pp) platform to study avian influenza virus, including the functional analysis of its hemagglutinin (HA) and neuraminidase (NA) envelope glycoproteins, the reassortment characteristics of the HAs and NAs, receptors, tropisms, neutralizing antibodies, diagnosis, infectivity, for the purposes of drug development and vaccine design. Here, we describe an experimental procedure to establish pps with the envelope glycoproteins (HA, NA) from two influenza A strains (HAPI H5N1 and 2013 avian H7N9). Their generation is based on the capacity of some viruses, such as murine leukemia virus (MLV), to incorporate envelope glycoproteins into a pp. In addition, we also detail how these pps are quantified with RT-qPCR, and the infectivity detection of native and mismatched virus pps depending on the origin of the HAs and NAs. This system is highly flexible and adaptable and can be used to establish viral pps with envelope glycoproteins that can be incorporated in any other type of enveloped virus. Thus, this viral particle platform can be used to study wild viruses in many research investigations.
Introduction
The mission of a viral particle is to transport its genome from an infected host cell to a non-infected host cell and to deliver it into the cytoplasm or the nucleus in a replication-competent form1. This process is initially triggered by binding to host cell receptors, followed by fusion of virion and cellular membranes. For enveloped viruses, like influenza viruses, the spike glycoproteins are responsible for receptor binding and fusion1,2. Viral envelope glycoproteins (e.g., pyrogens, antigens), are involved in many important properties and events, such as virus lifecycle initiation (binding and fusion), viral pathogenesis, immunogenicity, host cell apoptosis and cellular tropism, the cellular endocytic pathway, as well as interspecies transmission and reassortment1,3,4,5,6,7. Research on viral envelope glycoproteins will help us understand many aspects of the viral infection process. Pseudotyped viral particles (pp), also termed pseudovirions or pseudoparticles, can be generated through a pseudotyping technique8,9,10. This technology has been used to develop pseudotyped particles of many viruses, including hepatitis C11,12, hepatitis B13, vesicular stomatitis virus (VSV)14,15, and influenza virus16,17,18,19. This technology is based on the Gag-Pol protein of lentiviruses or other retroviruses.
Pseudotyped viral particles can be obtained using a three-plasmid system by cotransfecting a viral envelope glycoprotein expression plasmid, a retroviral packaging plasmid missing the envelope env gene, and a separate reporter plasmid into pp producer cells. The retrovirus is assembled by its Gag protein, and it buds from an infected cell membrane that expresses the virus envelope protein1. Therefore, it is possible to obtain high titer influenza pps using the retrovirus Gag protein to produce buds on a cellular membrane expressing influenza HA and NA. In our previous studies, HAs/NAs in all combinations were functional and able to perform their corresponding functions in the viral life cycle16,17,18,20,21. These pps are used to investigate influenza biological characteristics, including hemagglutination, neuraminidase activity, HA-receptor binding tropism, and infectivity. Because HA and NA are both important surface functional proteins in the viral life cycle, mismatched HAs and NAs derived from different strains of influenza can partly demonstrate reassortment between them. Here, we generate eight types of influenza pps by combining two HAs and two NAs (derived from the HPAI H5N1 strain and the H7N9 stain), using a three-plasmid pseudotyping system. These eight types of pps include two native pps, H5N1pp, H7N9pp; two mismatched pps, (H5+N9)pp, (H7+N1)pp; and four pps only harboring a single glycoprotein (HA or NA), H5pp, N1pp, H7pp, N9pp. Studies on the influenza virus, such as H5N1 and H7N9, are limited by biosafety requirements. All studies of the wild influenza virus strains should be performed in a biosafety level 3 (BSL-3) laboratory. Pseudotyped viral particle technology can be used to package an artificial virion in a biosafety level 2 (BSL-2) setting. Therefore, pps represent a safer and useful tool to study the influenza virus processes depending on its two major glycoproteins: hemagglutinin (HA) and neuraminidase (NA).
This protocol describes the generation of these pps with a three-plasmid cotransfection strategy (overviewed in Figure 1), how to quantify pps, and infectivity detection. The pp production involves three kinds of plasmids (Figure 1). The gag-pol gene, which encodes the retrovirus Gag-Pol protein, was cloned from a retrovirus packaging kit and inserted into the pcDNA 3.1 plasmid and named pcDNA-Gag-Pol. The enhanced green fluorescent protein (eGFP) gene, which encodes Green Fluorescent Protein, was cloned from pTRE-EGFP vector, inserted into the pcDNA 3.1 plasmid, and called pcDNA-GFP. During cloning, a packaging signal (ψ) sequence was added via a primer. The HA and NA genes were cloned into a pVRC plasmid, named pVRC-HA and pVRC-NA, respectively. The last plasmid encodes the fusion protein and can be replaced with any other fusion protein of interest. Our pseudotyping platform includes two glycoprotein expression plasmids: pVRC-HA and pVRC-NA. This can simplify the research on reassortment between different virus strains in a BSL-2 setting.
Protocol
1. Day 1: Cell Culture and Seeding
- Cultivate human embryonic kidney (HEK) 293T/17 cells in 60 mm dishes with Dulbecco's modified essential medium (DMEM) supplemented with 10% fetal bovine serum (FBS) and 100 U/mL penicillin-streptomycin (DMEM Complete Medium, DCM) in a 37 °C, 5% carbon dioxide (CO2) incubator until about 80% confluent.
NOTE: HEK 293T/17 low passage cells are recommended. - Carefully wash the cells with 5 mL of phosphate buffered saline (PBS) 1x.
NOTE: Manual handling of the HEK 293T/17 cells must be very gentle, because they easily detach. - Remove PBS and dissociate the cells with 1 mL of 0.25% trypsin-ethylene diamine tetraacetic acid (EDTA) solution. Place the dish in a 37 °C, 5% CO2 incubator for no more than 5 min until the cells are dissociated.
- Deactivate trypsin by adding 5 mL of DCM. Disperse the cells into a single-cell suspension by pipetting up and down several times.
- Transfer the cell suspensions to a prechilled 15 mL centrifuge tube. Collect the cells by centrifugation at 250 x g for 5 min at 4 °C.
- Decant as much of the supernatant as possible. Resuspend the cell pellet with 6 mL of DCM medium and count the cells. Dilute the cells to 1 x 106 cells/mL with DCM medium.
- Seed the cells into a 6 well plate with 1 mL of cell suspension per well. Gently pat the plate to evenly distribute the cells. Incubate the plate overnight (14–16 h) in a 37 °C, 5% CO2 incubator.
2. Day 2: Four-plasmid Cotransfection Mediated by Lipofection
- Check the cell morphology and density under an inverted light microscope. Ideally, cells should be approximately 85% confluent at transfection. Replace the medium with 1 mL of serum-free DMEM medium per well, and then put the plate back into the incubator.
NOTE: Manual handling of the HEK 293T/17 cells must be very gentle, because they easily detach. - For each well of cultured cells to be transfected, dilute 8 µL of the transfection reagent to a volume of 150 µL with Reduced Serum Medium (tube 1). Mix gently and incubate for 5 min at room temperature (RT, approximately 20 °C).
NOTE: For each transfection sample, prepare two 1.5 mL microcentrifuge tubes, numbered 1 and 2. - In tube 2, dilute 2.5 µg of plasmid DNA into 150 µL of Reduced Serum Medium.
NOTE: In tube 2, dilute each plasmid DNA as shown in Table 1. A plasmid encoding vesicular stomatitis virus (VSV) G glycoprotein (plasmid pLP-VSVG) was used as a positive control, because VSV is able to infect a wide range of cells. Negative control particles that lack influenza envelope glycoproteins (Δenv pps) were generated using pcDNA-Gag-Pol and pcDNA-GFP plasmids. - After a 5 min incubation, combine the diluted DNA with diluted transfection reagent. Mix gently and incubate for another 15 min at RT.
- Add the DNA-lipid complex to the corresponding well containing the cells and serum-free medium. Mix gently by rocking the plate back and forth.
- After incubation for 4–6 h in a 37 °C, 5% CO2 incubator, remove the medium, and replace with 2 mL of DMEM. Incubate for another 36–48 h in a 37 °C, 5% CO2 incubator.
NOTE: Replace with serum-free and antibody-free DMEM. In this protocol, two HAs and two NAs can be used to generate eight types of pps (shown in Table 1).
3. Day 3: Susceptible Cells Seeding
- For the infectivity assay, seed each type of susceptible cells at 1 x 104 cells per well in a 96 well plate.
NOTE: Use two types of target cell to perform the infectivity assay in this article: an alveolar-derived human cell line (A549 cells) and the Madin-Darby Canine Kidney (MDCK) cells. MDCK cells are widely used in influenza research and can be a good control. This step is flexible. Any other target cell lines can be used according to the research requirements. - Incubate the plate overnight (14–16 h) in a 37 °C, 5% CO2 incubator.
4. Day 4: Pseudotyped Viral Particle Collection, Quantification, and Infectivity Assay
- Pseudotyped viral particle collection
- Check the color of the medium. Ideally, it should be light pink or slightly orange. Examine the cells with an inverted fluorescent biological microscope under 440–460 nm.
- At 36–48 h posttransfection, harvest the pps by passaging through a 0.45 µm polyvinylidene fluoride (PVDF) membrane filter to eliminate cell debris.
- Divide the pps into small volume aliquots.
- Store the pps at -80 °C.
NOTE: The protocol can be paused here. However, this is not encouraged, because the infectivity of the pps will sharply decline after freezing and thawing.
- Pseudotyped viral particle quantification
- Transfer 20 µL of purified pps to a 1.5 mL ribonuclease (RNase)-free microcentrifuge tube.
- Add 1 µL of 0.24 U/mL benzonase nuclease. Incubate at 37 °C for 1 h to eliminate any DNA and RNA contamination.
NOTE: Target RNA, commonly downregulated cytomegalovirus (CMV)-GFP RNA, is packaged in the pps and can avoid being degraded by benzonase nuclease. - Freeze the sample at -70 °C to inactivate the benzonase nuclease.
- Add 2 µL of proteinase K. Incubate at 50 °C for 30 min to digest the envelope proteins and release the CMV-GFP RNA. Inactivate the proteinase K at 100 °C for 3 min.
- Quantify the pps by real-time quantitative reverse-transcription (qRT)-PCR with a Universal Probe One-Step RT-qPCR Kit, using the forward primer 5'-AACAAAAGCTGGAGCTCGTTTAA-3', the reverse primer 5'-GGGTCTCCTCAGAGTGATTGACTAC-3', and the probe 5'-FAM-CCCCCAAATGAAAGACCCCCGAG-TAM-3', on a Real-Time PCR thermocycler. Normalize the pps for RNA copy number before infectivity.
- Infectivity assay
- Dilute each type of pps in terms of the qRT-PCR data to 4 x 105 copies/mL (pp normalization).
- Add Tosyl-Phenylalanine Chloromethyl-Ketone (TPCK)-trypsin to a final concentration of 40 µg/mL into pps that harbor H7N9 HA. Incubate at 37 °C for 1 h to form its functional subunits HA1 and HA2.
NOTE: There is no need to treat the pps that harbor H5 with TPCK-trypsin, because they have multiple arginine and lysine residues at the HA1-HA2 cleavage site. This multi-basic cleavage site can be cleaved by ubiquitous cellular proteases. - Mix normalized pps with DMEM medium (serum-free) at a 1:1 ratio (volume/volume).
- Bring the plate containing susceptible cells to the biosafety cabinet.
- Aspirate the supernatant and wash the cells once with 0.1 mL of prewarmed PBS.
- Add 0.1 mL of pps-DMEM mixture to one well. Triplicate the infectivity tests of each type of pps to one susceptible cell line (overviewed in Figure 2).
- Incubate the 96 well plate for 4–6 h in a 37 °C, 5% CO2 incubator.
- Aspirate the supernatant and replace with 0.1 mL of DCM.
- Incubate the 96 well plate for another 24–36 h in a 37 °C, 5% CO2 incubator.
5. Day 5 or 6: Infectivity Detection
- Bring the 96 well plate to the biosafety cabinet.
- Aspirate the supernatant and wash the cells 1x with 0.2 mL of prewarmed PBS.
- Remove PBS and dissociate the cells with 0.1 mL of 0.25% trypsin-EDTA solution.
- Place the dish in a 37 °C, 5% CO2 incubator for 3 min until the cells are dissociated.
NOTE: Avoid incubating for more than 5 min, because this will lead to cell clumping. - Deactivate trypsin by adding 0.4 mL of DCM.
- Disperse the cells into single-cell suspension by pipetting up and down several times.
- Transfer the cell suspensions to a chilled 1.5 mL microcentrifuge tube.
- Determine the GFP reporter-positive cells with Fluorescence Activated Cell Sorting (FACS).
NOTE: To determine the ratio of GFP reporter-positive target cells, set flow cytometer gates using the control samples (pps-untreated A549 cells or MDCK cells), and then count the GFP reporter-positive cells of 10,000 cells per sample.
Representative Results
Depending on the general procedure described above, we have generated 10 types of pps combining two group HAs/NAs or VSV-G glycoprotein or no-envelope glycoproteins (shown in Table 1). Seven of them are infectious. The pps that harbor no-envelope glycoprotein or only harbor NA did not show any infectivity here. The influenza pp production procedure is overviewed in Figure 1. Transmission electron micrographs of pps (e.g., H5N1pp) are shown in Figure 3. The results of infectivity assays of these pps are shown in Figure 4. The infectivity of the seven types of pps was evaluated at a genome copies per cell (GCP) [similar to multiplicity of infection (MOI)] value of 20. In the pps group harboring H5, the infectivity of H5N1, (H5+N9), and H5 was 90.05 ± 4.05%, 17.78 ± 1.58%, 10.15 ± 2.85% for cell line A549 and 40.37 ± 4.92%, 5.24 ± 1.32%, 4.88 ± 0.27% for MDCK, respectively. In the pps group harboring H7, the infectivity of H7N9, (H7+N1), and H7 was 10.45 ± 2.35%, 6.75 ± 1.37%, 1.23 ± 0.33% for cell line A549 and 7.61 ± 1.04%, 4.12 ± 1.29%, 1.08 ± 0.02% for MDCK, respectively. For the infectivity assays of the pps, especially HApp (H5pp, H7pp), exogenous neuraminidase was not added. In this infectivity assay, the MDCK cells were also used as the control cell line to test pps infectivity. The infectivity of VSVGpp was 20.9 ± 2.00% for A549 and 16.02 ± 2.41% for MDCK cells. The delta-envelope glycoproteins pp (Δenv pp) showed no infectivity in our study. These data also showed that HAs/NAs from diverse virus strains are capable of successfully generate infectious viral particles. Taken together, our pseudotyping platform can develop infectious pseudotyped viral particles used in influenza research.
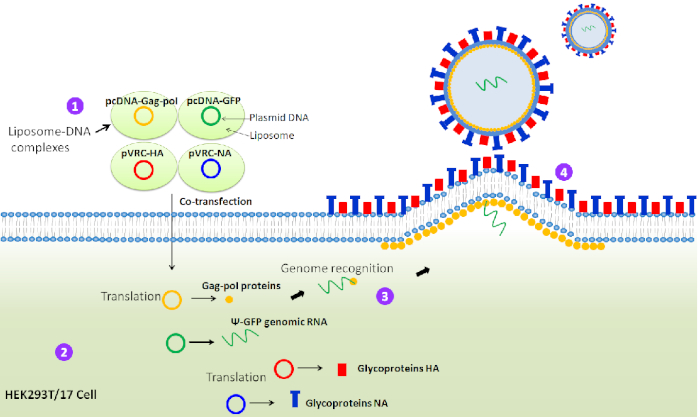
Figure 1: Overview of influenza pp production procedure. (A) The packaging plasmid pcDNA-Gag-pol, the reporter plasmid pcDNA-GFP, and the envelope glycoprotein expression plasmids pVRC-HA and pVRC-NA, are cotransfected into pp-producing HEK 293/17 cells. (B) In HEK 293/17 cells, the Gag-Pol polyproteins are synthesized and transported by an unknown mechanism to the cell membrane. Glycoproteins HA and NA are transported and anchored onto the cell membrane via the secretory pathway. Reporter plasmid pcDNA-GFP is transcribed into the single-stranded ψ-GFP genomic RNA. (C) During or after transport, the Gag-Pol protein recruits the single-stranded ψ-GFP genomic RNA via the psi-RNA packaging signals, thereby forming the pre-budding complexes. (D) The assembled Gag-pol-ψ-RNA complex induces membrane curvature, leading to the formation of a bud. During budding, the viral envelope glycoproteins HAs/NAs are incorporated into the nascent particles. Budding is completed as the particle pinches off from the cell membrane. Please click here to view a larger version of this figure.
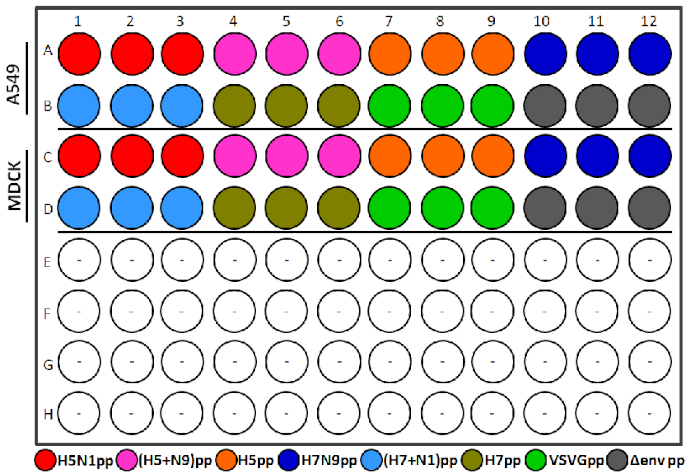
Figure 2: Overall arrangement in infectivity assay. The infectivity tests of each type of pps to one susceptible cell line were measured in triplicate. Alveolar-derived human cells A549 and MDCK are used as susceptible cells. Please click here to view a larger version of this figure.
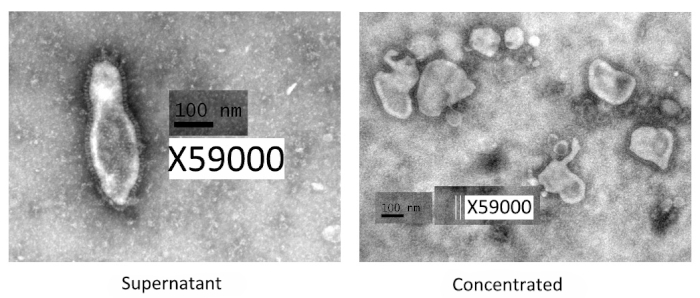
Figure 3: Transmission electron micrographs of pps. Unconcentrated (left) and concentrated (right) supernatant. Please click here to view a larger version of this figure.
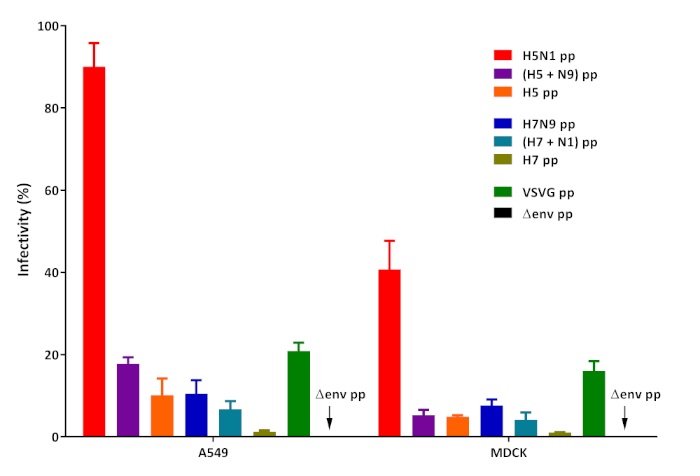
Figure 4: Infectivity of normalized pps. Infectivity is presented as the mean ± standard deviation (SD) percentage of infected cells (n = 3). Infectivity of pps was assessed in two cell lines, A549 and MDCK cells. Seven types of pps displayed various infectivity profiles in two target cells. Pps that only harbor NA are not shown here as they did not manifest any infectivity. Pps that harbor no-envelope glycoproteins (Δenv) also showed no infectivity in our study. The percent of infectivity denoted the ratio of GFP reporter-positive cells in 10,000 cells per sample. Please click here to view a larger version of this figure.
| plasmid preparations | ||||||||||
| plasmid (µL, 0.1 µg/µL) | H5N1 | (H5+N9) | H7N9 | (H7+N1) | H5 | N1 | H7 | N9 | VSVG | Δenv |
| pcDNA-Gag-pol | 10.53 | 10.53 | 10.53 | 10.53 | 11.43 | 11.43 | 11.43 | 11.43 | 11.43 | 12.5 |
| pcDNA-GFP | 10.53 | 10.53 | 10.53 | 10.53 | 11.43 | 11.43 | 11.43 | 11.43 | 11.43 | 12.5 |
| pVRC-HA | 1.98 | 1.98 | 1.98 | 1.98 | 2.14 | – | 2.14 | – | – | – |
| pVRC-NA | 1.98 | 1.98 | 1.98 | 1.98 | – | 2.14 | – | 2.14 | – | – |
| pcDNA-VSVG | – | – | – | – | – | – | – | – | 2.14 | – |
Table 1: Combinations of HA and NA proteins derived from H5N1 and H7N9 viruses and the required quantities (volume) of plasmid DNA for one well transfection of a 6 well plate. According to the concentration of plasmid preparations, calculate the required volume of each plasmid DNA. The total amount of plasmid DNA for tranfection of one well is 2.5 µg. To obtain the highest transfection efficiency and lowest non-specific effects, we optimized the transfection conditions by varying plasmid DNA and tranfection reagent concentrations. After optimizing, the ratio of the four plasmids quantities was set as 16:16:1:1. The volume of transfection reagent used in one well transfection of a 6 well plate is 8 µL (not shown in the table). Two HAs and two NAs from H5N1 and H7N9 viruses can be used to generate eight types of pps: H5N1pp, (H5 + N9)pp, H5pp, N1pp, H7N9pp, (H7 + N1)pp, H7pp and N9pp. The pps that harbor no-envelope glycoproteins (Δenv) or only harbor NA glycoproteins showed no infectivity in our study.
Discussion
In this protocol, we describe a method to produce influenza virus pseudotyped particles (pp) in a BSL-2 setting. The reporter plasmid pcDNA-GFP is incorporated into the pps and can be used to quantify pps by FACS in an infectivity assay. We chose two types of susceptible cell lines because they are widely used in influenza research. MDCK cells would provide a good control to the variable immortalized human cells used in these studies.
This protocol is based on the retrovirus MLV, which can incorporate a GFP reporter and produce buds on the cellular membrane. This technique has been widely developed for packaging influenza virus particles4,22,23,24. Some other systems are based on the lentiviral HIV-1 pseudotyping system19,25,26 or the baculovirus-insect cell expression system27,28,29. Many other reporter genes have also been used for pseudoparticle production, such as luciferase (luminescence)30,31,32,33, β-gal/LacZ (by colorimetry)34,35, and secreted alkaline phosphatase36,37. Millet et al. used the luciferase assay to quantify the infectivity of coronavirus pseudotyped particles33. Compared with luciferase, GFP's green fluorescence is easily observed with an inverted fluorescent biological microscope. This is a convenient way to check transfection and infection efficiencies. For this study, the infectivity can be determined directly by detecting the GFP-positive cells with FACS.
In this method, several steps critically affect the results. Optimized cell density is a critical factor for successful transfection. In this protocol, a cell density in the range of 80–90% confluent was found to be optimal for influenza virus pp production. Higher or lower cell density will result in lower transfection efficiency. Good physiological status of producer cells is also very important for high particle production. This is why lower cell passage HEK 293T/17 cells are recommended to produce pps in this protocol. Also, the volume of transfection reagent and the ratio of the four plasmids quantities can also affect the transfection efficiency. To obtain the highest transfection efficiency, it is recommended to optimize these factors by varying and testing their amount. We set the ratio of four plasmids quantities as 16:16:1:1 and the volume of transfection reagent as 8 µL for one well tranfection in a 6 well plate. Another issue is the handling of the cells. The HEK 293T/17producer cells are low-adhesion, so manual handling of the cells must be very gentle. Lipofection can lead to a cell permeability increase, and serum and antibodies in the medium may increase cytotoxicity. It is best to use serum-free and antibody-free DMEM to culture post-transfected HEK 293T/17 cells. Furthermore, collection time is important. At 36–48 h post-transfection, the color of the cell supernatant must be checked to make sure that it is pink or orange-pink before pp collection. Yellow supernatant indicates that the medium is too acidic to support cell growth and usually leads to poor pp yields.
We performed the transfection assay in a 6 well plate. To obtain more pp volume the number of transfection wells can be increased and supernatants that contain the same pps can be pooled together. Alternatively, some other kind of vessels can be used to increase pp yield. For instance, 18 µL of transfection reagent and 5.5 µg of plasmid DNA can be used to perform transfection with 2.2 x 106 cells in one 60 mm dish. Similarly, an infectivity assay can be carried out in a 24 well plate.
The success of this technique can be influenced by many factors. Therefore, the procedure should be optimized for particle packaging of different kinds of viruses.
In this protocol, pseudotyped viral particles of HPAI H5N1 and H7N9, as well as their reassortants, were generated. In this method, we use qRT-PCR of the GFP-RNA in the infectivity assay at the single-cell level (as genome copies per cell) instead of Tissue Culture Infectious Dose 50 (TCID50) or traditional MOI23,38,39. Virus infectivity titration methods are based on plaque assays or TCID50 assays, which are both time-consuming and labor-intensive. Both assays rely on the measurement of visible cytopathic effects (CPE) caused by virus infection in cell lines, so it may be hard to titrate viruses of low infectivity (i.e., H7pp in this study). We think it is a convenient, effective, and rapid method to normalize pps with qRT-PCR of the GFP RNA contained in influenza pps.
Taken together, our technique is safe and adaptable, and can be used to study enveloped viruses, including their receptors, tropisms, envelope glycoprotein function, neutralizing antibodies, antivirus drug development, diagnosis, and vaccine design and evaluation.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This work was supported by grants from Zhejiang Provincial Medicine and Health Science and Technology Plan (Grant Numbers, 2017KY538), Hangzhou Municipal Medicine and Health Science and Technology Plan (Grant Numbers, OO20190070), Hangzhou Medical Science and Technology key Project (Grant Numbers, 2014Z11) and Hangzhou municipal autonomous application project of social development and scientific research (Grant Numbers, 20191203B134).
Materials
| Benzonase Nuclease | Millipore | 70664 | Effective viscosity reduction and removal of nucleic acids from protein solutions |
| Clear Flat Bottom Polystyrene TC-treated Microplates (96-well) | Corning | 3599 | Treated for optimal cell attachment Sterilized by gamma radiation and certified nonpyrogenic Individual alphanumeric codes for well identification |
| Clear TC-treated Multiple Well Plates (6-wells) | Costar | 3516 | Individual alphanumerical codes for well identification Treated for optimal cell attachment Sterilized by gamma irradiation |
| Dulbecco's modified essential medium (DMEM) | Gibco | 11965092 | A widely used basal medium for supporting the growth of many different mammalian cells |
| Fetal bovine serum | Excell | FND500 | fetal bovine sera that can offer excellent value for basic cell culture, specialty research, and specific assays |
| Fluorescence Activated Cell Sorting (FACS) | Beckman coulter | cytoflex | |
| Human alveolar adenocarcinoma A549 cells | ATCC | CRM-CCL-185 | |
| Human embryonic kidney (HEK) HEK-293T/17 cells | ATCC | CRL-11268 | A versatile transfection reagent that has been shown to effectively transfect the widest variety of adherent and suspension cell lines |
| Inverted fluorescent biological microscope | Olympus | BX51-32P01-FLB3 | |
| Inverted light microscope | Olympus | CKX31-12PHP | |
| Lipofectamine 2000 Transfection Reagent | Invitrogen | 11668019 | Rapid, sensitive and precise probe-based qPCR detection and quantitation of target RNA targets. |
| Luna Universal Probe One-Step RT-qPCR Kit | NEB | E3006L | Will withstand up to 14,000 RCF RNase-/DNase-free Nonpyrogenic |
| Madin-Darby Canine Kidney (MDCK) cells | ATCC | CCL-34 | |
| MaxyClear Snaplock Microcentrifuge Tube (1.5 mL) | Axygen | MCT-150-C | 33 mm, gamma sterilized |
| Millex-HV Syringe Filter Unit, 0.45 µm, PVDF | Millipore | SLHV033RS | an improved Minimal Essential Medium (MEM) that allows for a reduction of Fetal Bovine Serum supplementation by at least 50% with no change in cell growth rate or morphology. Opti-MEM I medium is also recommended for use with cationic lipid transfection reagents, such as Lipofectamine reagent. |
| Opti-MEM I Reduced Serum Medium | Gibco | 11058021 | The antibiotics penicillin and streptomycin are used to prevent bacterial contamination of cell cultures due to their effective combined action against gram-positive and gram-negative bacteria. |
| penicillin-streptomycin | Gibco | 15140122 | Maximum RCF is 12,500 xg Temperature range from -80 °C to 120 °C RNase-/DNase-free Sterile |
| PP Centrifuge Tubes (15 mL) | Corning | 430791 | a stable and highly reactive serine protease |
| Proteinase K | Beyotime | ST532 | Treated for optimal cell attachment Sterilized by gamma radiation and certified nonpyrogenic |
| TC-treated Culture Dish (60mm) | Corning | 430166 | Trypsin from bovine pancreas TPCK Treated, essentially salt-free, lyophilized powder, ≥10,000 BAEE units/mg protein |
| TPCK-trypsin | Sigma | T1426 | This liquid formulation of trypsin contains EDTA and phenol red. Gibco Trypsin-EDTA is made from trypsin powder, an irradiated mixture of proteases derived from porcine pancreas. Due to its digestive strength, trypsin is widely used for cell dissociation, routine cell culture passaging, and primary tissue dissociation. The trypsin concentration required for dissociation varies with cell type and experimental requirements. |
| Trypsin-EDTA (0.25%), phenol red | Gibco | 25200056 |
References
- Knipe, D. M., Howley, P. M. . Fields Virology (6th). , (2013).
- White, J. M., Delos, S. E., Brecher, M., Schornberg, K. Structures and mechanisms of viral membrane fusion proteins: multiple variations on a common theme. Critical Reviews in Biochemistry and Molecular Biology. 43 (3), 189-219 (2008).
- Bright, R. A., et al. Cross-clade protective immune responses to influenza viruses with H5N1 HA and NA elicited by an influenza virus-like particle. PLoS One. 3 (1), 1501 (2008).
- Yang, J., et al. Reliability of pseudotyped influenza viral particles in neutralizing antibody detection. PLoS One. 9 (12), 113629 (2014).
- Wyatt, R., Sodroski, J. The HIV-1 envelope glycoproteins: fusogens, antigens, and immunogens. Science. 280 (5371), 1884-1888 (1998).
- Joe, A. K., Foo, H. H., Kleeman, L., Levine, B. The transmembrane domains of Sindbis virus envelope glycoproteins induce cell death. Journal of Virology. 72 (5), 3935-3943 (1998).
- Albecka, A., Laine, R. F., Janssen, A. F., Kaminski, C. F., Crump, C. M. HSV-1 Glycoproteins Are Delivered to Virus Assembly Sites Through Dynamin-Dependent Endocytosis. Traffic. 17 (1), 21-39 (2016).
- Huang, A. S., Palma, E. L., Hewlett, N., Roizman, B. Pseudotype formation between enveloped RNA and DNA viruses. Nature. 252 (5485), 743-745 (1974).
- Rubin, H. Genetic Control of Cellular Susceptibility to Pseudotypes of Rous Sarcoma Virus. Virology. 26, 270-276 (1965).
- Steffen, I., Simmons, G. Pseudotyping Viral Vectors With Emerging Virus Envelope Proteins. Current Gene Therapy. 16 (1), 47-55 (2016).
- Bartosch, B., Dubuisson, J., Cosset, F. L. Infectious hepatitis C virus pseudo-particles containing functional E1-E2 envelope protein complexes. Journal of Experimental Medicine. 197 (5), 633-642 (2003).
- Bian, T., Zhou, Y., Bi, S., Tan, W., Wang, Y. HCV envelope protein function is dependent on the peptides preceding the glycoproteins. Biochemical and Biophysical Research Communications. 378 (1), 118-122 (2009).
- Gudima, S., Meier, A., Dunbrack, R., Taylor, J., Bruss, V. Two potentially important elements of the hepatitis B virus large envelope protein are dispensable for the infectivity of hepatitis delta virus. Journal of Virology. 81 (8), 4343-4347 (2007).
- Yoshida, Y., Emi, N., Hamada, H. VSV-G-pseudotyped retroviral packaging through adenovirus-mediated inducible gene expression. Biochemical and Biophysical Research Communications. 232 (2), 379-382 (1997).
- Burns, J. C., Friedmann, T., Driever, W., Burrascano, M., Yee, J. K. Vesicular stomatitis virus G glycoprotein pseudotyped retroviral vectors: concentration to very high titer and efficient gene transfer into mammalian and nonmammalian cells. Proceedings of the National Academy of Sciences of the United States of America. 90 (17), 8033-8037 (1993).
- Zhang, F., et al. Characterization of pseudoparticles paired with hemagglutinin and neuraminidase from highly pathogenic H5N1 influenza and avian influenza A (H7N9) viruses. Virus Research. 253, 20-27 (2018).
- Zhang, F., et al. Infectivity of Pseudotyped Particles Pairing Hemagglutinin of Highly Pathogenic Avian Influenza a H5N1 Virus with Neuraminidases of The 2009 Pandemic H1N1 and a Seasonal H3N2. Journal of Bioterrorism & Biodefense. 2, 104 (2011).
- Wu, J., et al. Characterization of neuraminidases from the highly pathogenic avian H5N1 and 2009 pandemic H1N1 influenza A viruses. PLoS One. 5 (12), 15825 (2010).
- Nefkens, I., et al. Hemagglutinin pseudotyped lentiviral particles: characterization of a new method for avian H5N1 influenza sero-diagnosis. Journal of Clinical Virology. 39 (1), 27-33 (2007).
- Zhang, Y., et al. Hemagglutinin and neuraminidase matching patterns of two influenza A virus strains related to the 1918 and 2009 global pandemics. Biochemical and Biophysical Research Communications. 387 (2), 405-408 (2009).
- Lin, X., et al. Oseltamivir boosts 2009 H1N1 virus infectivity in vitro. Biochemical and Biophysical Research Communications. 390 (4), 1305-1308 (2009).
- McKay, T., Patel, M., Pickles, R. J., Johnson, L. G., Olsen, J. C. Influenza M2 envelope protein augments avian influenza hemagglutinin pseudotyping of lentiviral vectors. Gene Therapy. 13 (8), 715-724 (2006).
- Pan, H., et al. Autophagy mediates avian influenza H5N1 pseudotyped particle-induced lung inflammation through NF-kappaB and p38 MAPK signaling pathways. American Journal of Physiology-Lung Cellular and Molecular Physiology. 306 (2), 183-195 (2014).
- Szecsi, J., et al. Induction of neutralising antibodies by virus-like particles harbouring surface proteins from highly pathogenic H5N1 and H7N1 influenza viruses. Virology Journal. 3, 70 (2006).
- Garcia, J. M., Lagarde, N., Ma, E. S., de Jong, M. D., Peiris, J. S. Optimization and evaluation of an influenza A (H5) pseudotyped lentiviral particle-based serological assay. Journal of Clinical Virology. 47 (1), 29-33 (2010).
- Garcia, J. M., Lai, J. C. Production of influenza pseudotyped lentiviral particles and their use in influenza research and diagnosis: an update. Expert Review of Anti-infective Therapy. 9 (4), 443-455 (2011).
- Haynes, J. R., et al. Influenza-pseudotyped Gag virus-like particle vaccines provide broad protection against highly pathogenic avian influenza challenge. Vaccine. 27 (4), 530-541 (2009).
- Schmeisser, F., et al. Production and characterization of mammalian virus-like particles from modified vaccinia virus Ankara vectors expressing influenza H5N1 hemagglutinin and neuraminidase. Vaccine. 30 (23), 3413-3422 (2012).
- Liu, Y. V., et al. Chimeric severe acute respiratory syndrome coronavirus (SARS-CoV) S glycoprotein and influenza matrix 1 efficiently form virus-like particles (VLPs) that protect mice against challenge with SARS-CoV. Vaccine. 29 (38), 6606-6613 (2011).
- Moeschler, S., Locher, S., Conzelmann, K. K., Kramer, B., Zimmer, G. Quantification of Lyssavirus-Neutralizing Antibodies Using Vesicular Stomatitis Virus Pseudotype Particles. Viruses. 8 (9), 254 (2016).
- Lai, A. L., Millet, J. K., Daniel, S., Freed, J. H., Whittaker, G. R. The SARS-CoV Fusion Peptide Forms an Extended Bipartite Fusion Platform that Perturbs Membrane Order in a Calcium-Dependent Manner. Journal of Molecular Biology. 429 (24), 3875-3892 (2017).
- Millet, J. K., et al. Middle East respiratory syndrome coronavirus infection is inhibited by griffithsin. Antiviral Research. 133, 1-8 (2016).
- Millet, J. K., et al. Production of Pseudotyped Particles to Study Highly Pathogenic Coronaviruses in a Biosafety Level 2 Setting. Journal of Visualized Experiments. (145), e59010 (2019).
- Ma, M., et al. Murine leukemia virus pseudotypes of La Crosse and Hantaan Bunyaviruses: a system for analysis of cell tropism. Virus Research. 64 (1), 23-32 (1999).
- Wool-Lewis, R. J., Bates, P. Characterization of Ebola virus entry by using pseudotyped viruses: identification of receptor-deficient cell lines. Journal of Virology. 72 (4), 3155-3160 (1998).
- Chen, C. M., et al. Production and design of more effective avian replication-incompetent retroviral vectors. Developmental Biology. 214 (2), 370-384 (1999).
- Kaku, Y., et al. Second generation of pseudotype-based serum neutralization assay for Nipah virus antibodies: sensitive and high-throughput analysis utilizing secreted alkaline phosphatase. Journal of Virological Methods. 179 (1), 226-232 (2012).
- Rudiger, D., Kupke, S. Y., Laske, T., Zmora, P., Reichl, U. Multiscale modeling of influenza A virus replication in cell cultures predicts infection dynamics for highly different infection conditions. PLOS Computational Biology. 15 (2), 1006819 (2019).
- Petiot, E., et al. Influenza viruses production: Evaluation of a novel avian cell line DuckCelt(R)-T17. Vaccine. 36 (22), 3101-3111 (2018).

