An Experimental Paradigm for the Prediction of Post-Operative Pain (PPOP)
Summary
Diffuse noxious inhibitory control, temporal summation and wound hyperalgesia testing are demonstrated in the obstetric patient. These tests evaluate inhibitory and excitatory mechanisms of pain processing and are here utilized to evaluate endogenous analgesia at different time-points during pregnancy and the peripartum period to help reveal individual s risk for persistent pain.
Abstract
Many women undergo cesarean delivery without problems, however some experience significant pain after cesarean section. Pain is associated with negative short-term and long-term effects on the mother. Prior to women undergoing surgery, can we predict who is at risk for developing significant postoperative pain and potentially prevent or minimize its negative consequences? These are the fundamental questions that a team from the University of Washington, Stanford University, the Catholic University in Brussels, Belgium, Santa Joana Women’s Hospital in São Paulo, Brazil, and Rambam Medical Center in Israel is currently evaluating in an international research collaboration. The ultimate goal of this project is to provide optimal pain relief during and after cesarean section by offering individualized anesthetic care to women who appear to be more ‘susceptible’ to pain after surgery.
A significant number of women experience moderate or severe acute post-partum pain after vaginal and cesarean deliveries. 1 Furthermore, 10-15% of women suffer chronic persistent pain after cesarean section. 2 With constant increase in cesarean rates in the US 3 and the already high rate in Brazil, this is bound to create a significant public health problem. When questioning women’s fears and expectations from cesarean section, pain during and after it is their greatest concern. 4 Individual variability in severity of pain after vaginal or operative delivery is influenced by multiple factors including sensitivity to pain, psychological factors, age, and genetics. The unique birth experience leads to unpredictable requirements for analgesics, from ‘none at all’ to ‘very high’ doses of pain medication. Pain after cesarean section is an excellent model to study post-operative pain because it is performed on otherwise young and healthy women. Therefore, it is recommended to attenuate the pain during the acute phase because this may lead to chronic pain disorders. The impact of developing persistent pain is immense, since it may impair not only the ability of women to care for their child in the immediate postpartum period, but also their own well being for a long period of time.
In a series of projects, an international research network is currently investigating the effect of pregnancy on pain modulation and ways to predict who will suffer acute severe pain and potentially chronic pain, by using simple pain tests and questionnaires in combination with genetic analysis. A relatively recent approach to investigate pain modulation is via the psychophysical measure of Diffuse Noxious Inhibitory Control (DNIC). This pain-modulating process is the neurophysiological basis for the well-known phenomenon of ‘pain inhibits pain’ from remote areas of the body. The DNIC paradigm has evolved recently into a clinical tool and simple test and has been shown to be a predictor of post-operative pain.5 Since pregnancy is associated with decreased pain sensitivity and/or enhanced processes of pain modulation, using tests that investigate pain modulation should provide a better understanding of the pathways involved with pregnancy-induced analgesia and may help predict pain outcomes during labor and delivery. For those women delivering by cesarean section, a DNIC test performed prior to surgery along with psychosocial questionnaires and genetic tests should enable one to identify women prone to suffer severe post-cesarean pain and persistent pain. These clinical tests should allow anesthesiologists to offer not only personalized medicine to women with the promise to improve well-being and satisfaction, but also a reduction in the overall cost of perioperative and long term care due to pain and suffering. On a larger scale, these tests that explore pain modulation may become bedside screening tests to predict the development of pain disorders following surgery.
Protocol
PRE-OPERATIVE METHODS: QUESTIONNAIRES, mTS & DNIC
Part 1: Demographic, Psychosocial & Pain-related Personality Questionnaires
- First, a demographic questionnaire is administered to collect data related to women s medical history, including pain preceding pregnancy and recent history during pregnancy and up to their delivery.
- Psychosocial questionnaires are administered before the DNIC procedure and during two 5-minute breaks that fall within the DNIC procedure. The Spielberger’s State-Trait Anxiety Inventory is administered before the procedure, the Fear of Pain Questionnaire-III is administered during the first 5-minute break and the Pain Catastrophizing Scale questionnaire is administered during the second 5-minute break. The Spielberger’s State-Trait Anxiety Inventory states emotional conditions and assesses first the level of state anxiety and then assesses the level of trait anxiety. The Fear of Pain Questionnaire-III contains descriptions of severe pain, minor pain, and medical pain. The Pain Catastrophizing Scale includes items that represent the three components of pain catastrophizing: rumination, magnification, and helplessness.
- Lastly, the Short-Form McGill Pain Questionnaire 2 may be administered at any convenient time point pre-operatively to quantify the degree of neuropathic and non-neuropathic pain a subject experiences.
Part 2: Mechanical Temporal Summation (mTS) Assessment
- On the woman s forearm, the researcher applies a 180 gram von Frey filament once or twice to familiarize with the pinprick sensation. Then it is applied 11 times within a 1 cm diameter circle. After one touch, the woman is asked to rate the pinprick pain on a 0-100 verbal numerical pain scale. Then ten consecutive touches are applied at random locations with a 1 second interstimulus interval and the subject is asked to rate the pain of the 10th application.
Part 3: Diffuse Noxious Inhibitory Control (DNIC) Assessment
- In a private exam room, the pregnant woman is seated in a comfortable position with a pillow placed in her lap. Women are told that small-talk and conversation will not take place during the test in order to obtain consistent results. Women are asked to concentrate as best they can on the instructions that are described to them. The researcher follows a script to administer instructions. First, the 11-point verbal numerical pain scale is explained and then the test is briefly explained.
- The heat thermode is carefully placed on the inside part of the woman’s dominant volar forearm and is secured with a Velcro strap. The woman is asked to relax her arm while keeping the thermode in the same position.
- The first part of the test involves familiarizing the woman with two distinct heat sensations and getting her used to rating the painful sensation upon request. The thermode increases and decreases at 8°C/sec from 32°C to 43°C and then again from 32°C to 44°C. Each target temperature, first 43°C and 44°C, remains for 7 seconds. The interstimulus interval is set to 2 seconds. The increasing/decreasing rate and interstimulus interval settings remain at 8°C/sec and 2 seconds, respectively, throughout the entire procedure. When not activated, the thermode rests at a baseline temperature of 32°C. The subject is asked to rate the pain on an 11-point verbal numerical pain scale six seconds after the thermode reaches the target temperature.
- The next part of the test involves applying three consecutive temperatures to determine the temperature the woman reports with a pain intensity of 6 on the 0-10 scale. This is done by first heating the thermode to 45, 46 and 47˚C in random order. Depending on the responses of the woman for each temperature, the range of the three temperatures will be increased or decreased by 1˚C. The thermode is not able to reach temperatures above 48˚C.
- The pain-6 temperature is then confirmed.
- Now the thermode is removed from the woman s forearm for at least 5 minutes. This is a good time for a subject to complete questionnaires and paperwork.
- After at least 5 minutes, the thermode is placed in the same position on the woman s forearm.
- The next part of the test involves the thermode heating up to the pain-6 temperature for 30 seconds. The woman is asked to rate the pain at 0, 10, 20, and 30 seconds during the test stimulus. This 30 second heat stimulus is the first test stimulus.
- Again, the thermode is removed from the woman s forearm for at least 5 minutes, during which time more questionnaires and paperwork may be completed.
- After at least 5 minutes, the thermode is placed once again in the same position on the woman s forearm.
- For the last part of the test, the DNIC pathway will be tested with the hot water bath conditioning stimulus. The water in the water bath is kept at a constant 46.5˚C. The woman submerges her entire hand (the non-dominant one) until the wrist in the water for a full minute and during the last 30 seconds of the minute the thermode heats up to the same pain-6 temperature. For the first 30 seconds, the woman is asked to rate every 10 seconds the painful sensation generated by the hand in the water bath. Then, for the last 30 seconds, she is asked to rate the painful sensation caused by the thermode (at 40, 50 and 60 seconds time points).
Part 4: Calculation of DNIC and mTS
- Mechanical temporal summation is calculated by subtracting the pain rating after the 1st touch from the pain rating after the 10th touch.
- To calculate a DNIC score, the average of the last three pain ratings or the last pain rating of the unconditioned test stimulus is subtracted from the average of the last three pain ratings or the last pain rating of the conditioned test stimulus, respectively.
PERI-PARTUM DATA
Part 5: Delivery Information
Mode of delivery, analgesia for labor and delivery or standardized spinal anesthesia for cesarean section and obstetrical and neonatal demographics are recorded.
Part 6: Clinical Pain Ratings and Pain Medication
Pain ratings on an 11-point numerical pain scale are collected during the time of labor and delivery and 12, 24 and 48 hours post-operatively. For women with a scheduled cesarean section, pain ratings are recorded at the time of the incision, the delivery of the baby, and the time skin staples or sutures are placed. Post-operatively, pain ratings around the incision are recorded while resting, sitting and in general from her uterus cramping.
The time points and doses of any opioids, acetaminophen, and non-steroidal anti-inflammatory drugs consumed 0 to 48 hours postpartum for post-operative pain are documented. Information regarding the duration of the epidural effect is recorded.
Part 7: Blood sample
Peripheral blood is obtained (EDTA vacutainer, 3ml) for DNA extraction.
POST-CESAREAN DELIVERY
Part 8: 48-hour Wound Hyperalgesia
- Dynamic and static hyperalgesia are assessed 48 hours after cesarean delivery.
- First, the area of dynamic hyperalgesia for punctate mechanical stimuli around the surgical incision is measured around the scar according to the method described by Stubhaug et al. (1997). In brief, stimulation with a 180 gram von Frey Filament is started from outside the hyperalgesic area where no pain sensation is experienced and moved toward the incision until the woman reports a distinct change in perception. The first point where a painful, sore, or sharp feeling appears is marked, and the distance to the incision is measured. If no change in sensation appears, stimulation is stopped at 0.5 cm from the incision. The area of secondary hyperalgesia is determined by testing along radial lines separated by 2.5 cm around the incision. The observations are translated onto graph paper, and the surface is calculated as the sum of the distances to the incision from points of hyperalgesia in cm divided by the cm length of the incision.
- Next, the pain threshold for mechanical static punctate stimuli is assessed using an electronic von Frey device. In brief, women are instructed to close their eyes during the procedure. An electronic von Frey filament is applied to the designated point on the skin (1 cm above the abdominal incision) and applications are separated by at least 30 seconds. Tactile pain threshold is defined as the smallest force (g/mm2) that is perceived as painful. Three determinations are made for each assessment and a mean is calculated.
LONG-TERM FOLLOW-UP METHODS: 2, 6 AND 12-MONTH PAIN QUESTIONNAIRE
Part 9: Follow-up Pain Questionnaire via Telephone Interview 2, 6 & 12 Months Postpartum
Lastly, a researcher calls subjects 2, 6 and 12 months after her cesarean section to administer the Short-form McGill Pain Questionnaire 2 and a customized questionnaire, which assesses post-operative pain experiences. This telephone interview usually takes no longer than 5 minutes.
Part 10: Representative Results
To date, we performed mTS and DNIC pre-operatively in 75 women (n=38 in Brazil and n=37 in UWMC Seattle). Figure 1 shows graphic representation of pre-cesarean DNIC score.
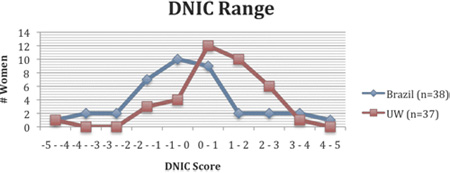
Figure 1. DNIC score in Brazilian and North-American women scheduled for elective cesarean deliveries. Efficient endogenous analgesia is represented by positive DNIC score (0 to +5). Lack of endogenous analgesia is represented by negative DNIC score (0 to -5).
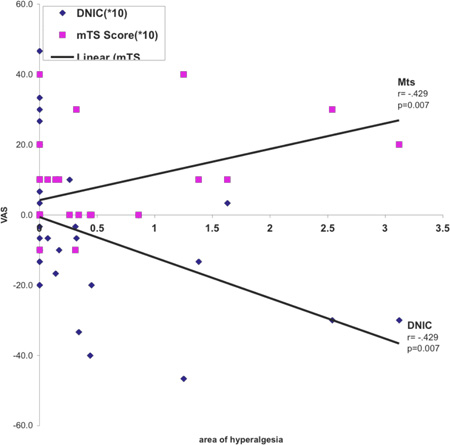
Figure 2. Correlation between pre-operative DNIC score/mTS and 48h wound hyperalgesia.
Discussion
Preliminary data reveals that mTS and DNIC may be correlated with greater post-cesarean hyperalgesia. If pre-operative mTS, DNIC, genetic testing and psychosocial questionnaires can predict individual susceptibility to develop severe post-operative pain and persistent pain, patients may be stratified to different risk groups. In return, different treatments including preemptive multimodal analgesia may have different outcomes in each subset of patients.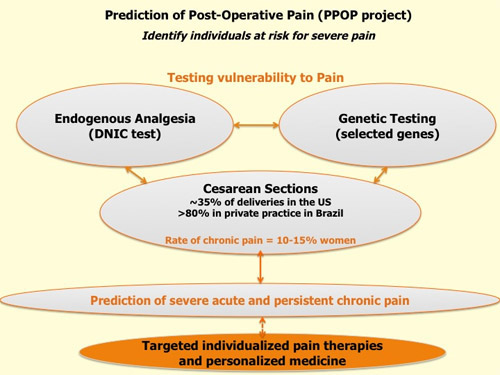
Figure 3. Prediction of post-operative pain (PPOP project).
Acknowledgements
UWMC Department of Anesthesiology and Pain Medicine
Materials
| Material Name | Type | Company | Catalogue Number | Comment |
|---|---|---|---|---|
| Pathway – Pain and Sensory Evaluation System | Medoc Advanced Medical Systems, Durham, North Carolina | |||
| Boekel 14L Hot Tub | Boekel Scientific, Feasterville, Pennsylvania | |||
| 180g Touch-Test Sensory Evaluator | North Coast Medical, Morgan Hill, California | |||
| Electronic von Frey | Bioseb, Cedex, France |
References
- Eisenach, J. C., Pan, P. H., Smiley, R., Lavand’homme, P., Landau, R., Houle, T. T. Severity of acute pain after childbirth, but not type of delivery, predicts persistent pain and postpartum. Pain. 140, 87-94 (2008).
- Kehlet, H., Jensen, T. S., Woolf, C. J. Persistent postsurgical pain: risk factors and prevention. Lancet. 367, 1618-1625 (2006).
- Ecker, J. L., Frigoletto, F. D. Cesarean delivery and the risk-benefit calculus. N Engl J Med. 356, 885-888 (2007).
- Carvalho, B., Cohen, S. E., Lipman, S. S., Fuller, A., Mathusamy, A. D., Macario, A. Patient preferences for anesthesia outcomes associated with cesarean delivery. Anesth Analg. 101, 1182-1187 (2005).
- Yarnitsky, D., Crispel, Y., Eisenberg, E., Granovsky, Y., Ben-Nun, A., Sprecher, E., Best, L. A., Granot, M. Prediction of chronic post-operative pain: pre-operative DNIC testing identifies patients at risk. Pain. 138, 22-28 (2008).

