大鼠舌的机械和粘弹性的体内评估
Summary
我们描述了麻醉大鼠模型中用于确定舌头的肌肉紧张度和粘弹性质的外科手术。该程序涉及舌下神经的特异性刺激,并将被动的李萨如力/变形曲线应用于肌肉。
Abstract
舌头是大多数脊椎动物口腔地板上高度支配和血管化的肌肉液压稳定器。其主要功能包括支持咀嚼和吞咽,以及味觉和语音学。因此,舌头的强度和体积可以影响脊椎动物完成基本活动,如喂养,沟通和呼吸的能力。具有睡眠呼吸暂停的人类患者具有扩大的舌头,其特征在于肌肉紧张度降低和肌肉内脂肪增加,可通过磁共振成像(MRI)进行可视化和定量。测量舌的力产生和粘弹性的能力构成了获取与成像数据相关的功能信息的重要工具。在这里,我们提出了通过电刺激舌下神经测量麻醉Zucker大鼠舌力产生的技术,并确定粘弹性性质通过施加被动的李萨如力/变形曲线来解释舌头。
Introduction
舌头为咀嚼,吞咽,味觉和口语提供了重要的支持。外在和内在的肌肉组织的存在,具有明显的神经支配和解剖/功能,解释了这种肌肉液压稳定器的独特性。成像技术的最新进展提供了其复杂解剖学1的更详细的观点。舌头功能减退,舌萎缩,吞咽困难和言语障碍也是肌病情况的常见表现,如帕金森病2 ,肌萎缩性侧索硬化(ALS) 3 ,肌强直性营养不良(MD) 4等肌病。
与常见疾病相关的肌肉组成的变化影响舌头的机械和粘弹性质。例如,舌力的功能分析揭示了与衰老相关的收缩性质的变化ss =“xref”> 5,6 ,缺氧7,8和肥胖9,10 。在肌营养不良的情况下,增加的纤维化导致更高的肌肉僵硬度,这意味着当应用李萨如变形方案时,对变形的依从性降低11 。相反,肌肉脂肪含量的变化,如在肥胖患者中记录的那样,改变了骨骼肌13,14的代谢12和机械性质,并预测会增加肌肉对变形的依从性。增加的舌头脂肪也与人类17阻塞性睡眠呼吸暂停(OSA)的发展相关,通过增加舌体积到部分上呼吸道闭塞点(呼吸暂停) 15,16 。辛肥胖的Zucker大鼠10中已经记录了舌头脂肪浸润,这表明这种模型是研究脂肪浸润对舌头生理的影响的有价值的工具。
测量舌力需要精细的手术技术来分离和双向刺激舌下神经17,18 。之前已经在大鼠5,17,19,20 ,兔21和人22,23中描述了这样的技术,但对研究者有有限的视觉辅助。由于其高度的技术性质,详细协议的可用性将显着提高该技术的可访问性和可重复性。我们的实验范例的目标是生病ustrate一种有效和可靠的技术测量大鼠模型中舌头的强度和粘弹性。为了达到这个目的,大鼠被麻醉,舌下神经被暴露,气管插管,以确保自由进入动物的舌头。缝合环然后将舌头的尖端连接到能够控制力和长度的力传感器,而两个双极钩电极刺激舌下神经以引起舌头的收缩。在力测量完成后,力传感器的长度控制能力用于根据具有固定振幅(Lissajous曲线)的正弦波协议,持续时间和频率快速改变舌头的长度,从而允许推导其粘弹性11,24。协议将指导调查员通过解剖步骤,动物在实验平台上的定位rm,放置电极,最后到力和粘弹性数据的获取和分析。
Protocol
Representative Results
Discussion
舌质代谢和/或组成的变化, 例如由肥胖引起的舌头脂肪浸润,预计会导致我们的方案评估参数的量化变化。舌力的量化是非常有意义的,因为突出和侵袭性活动之间的不平衡或整体舌头衰弱可能导致上呼吸道15的闭塞。旨在增加舌强度的运动技术已经成功应用于大鼠25,26 ,也在人体27,28,29中 ,其中它们有效地降低了睡眠呼吸暂?…
Declarações
The authors have nothing to disclose.
Acknowledgements
这项调查得到了两个国家卫生研究院的支持:HL089447(“肥胖与OSA:了解舌头脂肪和代谢功能的重要性”)和HL094307(“了解肥胖与舌头脂肪之间的关系”)
Materials
| SurgiSuite (heated Surgical tray) | Kent Scientific | SurgiSuite-LG | Includes heated platform |
| LED Lighting and Magnification Kit | Kent Scientific | SURGI- 5003 | |
| RC2 Rodent Circuit Controller | VetEquip | 922100 | |
| Isoflurane | Butler Schein Animal Health Supply | 29405 | |
| Alcohol Prep | Webcol | 6818 | |
| Cotton-tipped applicators | MediChoice | WOD1002 | |
| Hair clipper | Conair | ||
| Hair remover lotion | Nair | ||
| Medical tape | Transpore | 3M | |
| D-PBS | Corning | 21-030-CM | |
| Operating Scissors | World Precision Instruments | 503717-12 | |
| Hemostatic Forceps | Merit | 97-458 | Any tissue forceps can be used instead |
| Microdissecting Forceps, Angled, Serrated, 10.2cm, SS | World Precision Instruments | 504479 | |
| Suture Tying Forceps | Fine Science Tools | 18025-10 | |
| Blunt Micro Hook | Fine Science Tools | 10062-12 | |
| Microhemostat | Fine Science Tools | 12075-14 | |
| Thermal cautery | WPI | 501292 | Disposable cauteries are available at lower cost |
| IV 14g x 3.25" cannula | BD | B-D382268H | For tracheal cannulation |
| Braided silk non-absorbable suture size 4-0 | Harvard Apparatus | SP104 | For stabilization of the tracheal cannula |
| Braided non-absorbable silk 5/0 suture | Surgik LC, USA | ESILRC15387550 | For suturing the tongue |
| Plastic-coated metal twist-tie (or electrical wire) | For securing the rat's nose to the platform | ||
| Camera stick | |||
| 3 way-swivel and Trilene 9Kg test monofilament line | Berkley | For securing the jaw and maintaining the mouth open | |
| Camera stick with adjustable angle | For supporting the 3 way-swivel and maintaining the mouth open. | ||
| in situ Muscle Test System | Aurora Scientific | 809C | This system is designed for mice and was modified by extending the platform. Alternatively the rat-specific 806D system can be used. |
| Dual-Mode Muscle lever (force transducer) | Aurora Scientific | 305C-LR | 309C offers higher excursion capabilities than 305C-LR. Link for more information and specifications: http://aurorascientific.com/products/muscle-physiology/dual-mode-muscle-levers/ |
| Needle Electrodes (surgical steel, 29 gauge) | AD Instruments | MLA1204 | 300C is recommended for use in mice. |
| Magnetic Stands | World Precision Instruments | M10 | Used for making the bipolar stimulating hook electrodes |
| Kite Manual Micromanipulator | World Precision Instruments | KITE-R and KITE-L | Require a steel plate |
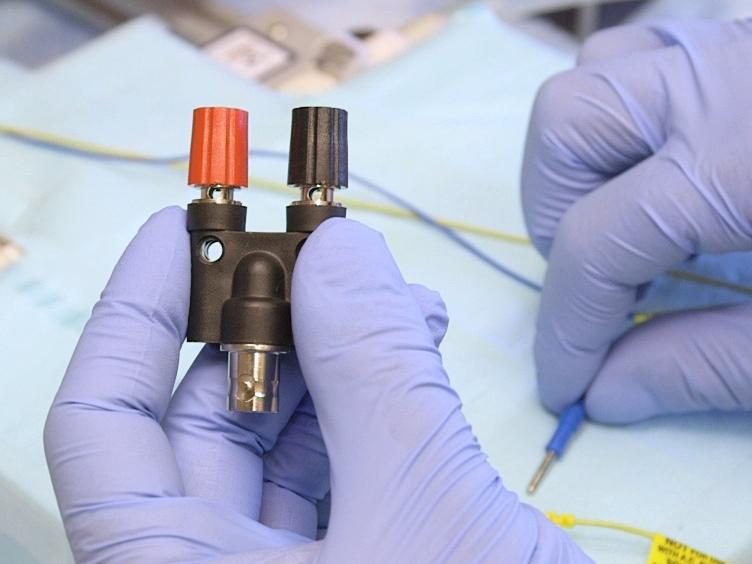
| Stackable Double Binding Post with Banana Jack x BNC Jack | McMaster Carr | 6704K13 | |
| Carbon fiber composites digital caliper | VWR | 36934-152 |
Referências
- Sanders, I., Mu, L. A three-dimensional atlas of human tongue muscles. Anat Rec (Hoboken). 296 (7), 1102-1114 (2013).
- Ciucci, M. R., et al. Tongue force and timing deficits in a rat model of Parkinson disease. Behav Brain Res. 222 (2), 315-320 (2011).
- Easterling, C., Antinoja, J., Cashin, S., Barkhaus, P. E. Changes in tongue pressure, pulmonary function, and salivary flow in patients with amyotrophic lateral sclerosis. Dysphagia. 28 (2), 217-225 (2013).
- Wang, Z. J., Huang, X. S. Images in clinical medicine. Myotonia of the tongue. N Engl J Med. 365 (15), e32 (2011).
- Ota, F., Connor, N. P., Konopacki, R. Alterations in contractile properties of tongue muscles in old rats. Ann Otol Rhinol Laryngol. 114 (10), 799-803 (2005).
- Schwarz, E. C., Thompson, J. M., Connor, N. P., Behan, M. The Effects of Aging on Hypoglossal Motoneurons in Rats. Dysphagia. 24 (1), 40 (2008).
- Pae, E. -. K., Wu, J., Nguyen, D., Monti, R., Harper, R. M. Geniohyoid muscle properties and myosin heavy chain composition are altered after short-term intermittent hypoxic exposure. J Appl Physiol. 98 (3), 889-894 (2005).
- Fuller, D. D., Fregosi, R. F. Fatiguing contractions of tongue protrudor and retractor muscles: influence of systemic hypoxia. J Appl Physiol. 88 (6), 2123-2130 (2000).
- Ray, A. D., Farkas, G. A., Pendergast, D. R. In-situ mechanical characteristics of the tongue are not altered in the obese Zucker rat. Sleep. 32 (7), 957 (2009).
- Brennick, M. J., et al. Tongue fat infiltration in obese versus lean Zucker rats. Sleep. 37 (6), 1095-1102 (2014).
- Stedman, H. H., Sweeney, H. L., Shrager, J. B., Maguire, H. C., Panettieri, R. A., Petrof, B., Narusawa, M., Leferovich, J. M., Sladky, J. T., Kelly, A. M. The mdx mouse diaphragm reproduces the degenerative changes of Duchenne muscular dystrophy. Nature. 352 (6335), 536-539 (1991).
- Goodpaster, B. H., Wolf, D. Skeletal muscle lipid accumulation in obesity, insulin resistance, and type 2 diabetes. Pediatr Diabetes. 5 (4), 219-226 (2004).
- Loro, E., et al. IL-15Rα is a determinant of muscle fuel utilization, and its loss protects against obesity. Am J Physiol Regul Integr Comp Physiol. 309 (8), R835-R844 (2015).
- Rahemi, H., Nigam, N., Wakeling, J. M. The effect of intramuscular fat on skeletal muscle mechanics: implications for the elderly and obese. J R Soc Interface. 12 (109), 20150365 (2015).
- Kim, A. M., et al. Tongue fat and its relationship to obstructive sleep apnea. Sleep. 37 (10), 1639-1648 (2014).
- Kim, A. M., et al. Metabolic activity of the tongue in obstructive sleep apnea. A novel application of FDG positron emission tomography imaging. Am J Respir Crit Care Med. 189 (11), 1416-1425 (2014).
- Gilliam, E. E., Goldberg, S. J. Contractile properties of the tongue muscles: effects of hypoglossal nerve and extracellular motoneuron stimulation in rat. J Neurophysiol. 74 (2), 547-555 (1995).
- Sokoloff, A. J. Localization and contractile properties of intrinsic longitudinal motor units of the rat tongue. J Neurophysiol. 84 (2), 827-835 (2000).
- Becker, B. J., Russell, J. A., Connor, N. P. Effects of aging on evoked retrusive tongue actions. Arch Oral Biol. 60 (6), 966-971 (2015).
- Connor, N. P., et al. Tongue muscle plasticity following hypoglossal nerve stimulation in aged rats. Muscle Nerve. 47 (2), 230-240 (2013).
- Seo, J., et al. Nerve cuff electrode using embedded magnets and its application to hypoglossal nerve stimulation. J Neural Eng. 13 (6), 066014 (2016).
- Friedman, M., et al. Targeted hypoglossal nerve stimulation for the treatment of obstructive sleep apnea: Six-month results. Laryngoscope. 126 (11), 2618-2623 (2016).
- Heiser, C., Maurer, J. T., Steffen, A. Functional outcome of tongue motions with selective hypoglossal nerve stimulation in patients with obstructive sleep apnea. Sleep Breath. 20 (2), 553-560 (2016).
- Syme, D. A. Passive viscoelastic work of isolated rat, Rattus norvegicus, diaphragm muscle. J Physiol. 424, 301-315 (1990).
- Connor, N. P., et al. Effect of tongue exercise on protrusive force and muscle fiber area in aging rats. J Speech Lang Hear Res. 52 (3), 732-744 (2009).
- Schaser, A. J., Stang, K., Connor, N. P., Behan, M. The effect of age and tongue exercise on BDNF and TrkB in the hypoglossal nucleus of rats. Behav Brain Res. 226 (1), 235-241 (2012).
- Puhan, M. A., et al. Didgeridoo playing as alternative treatment for obstructive sleep apnea syndrome: randomised controlled trial. BMJ. 332 (7536), 266-270 (2006).
- Guimarães, K. C., Drager, L. F., Genta, P. R., Marcondes, B. F., Lorenzi-Filho, G. Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 179 (10), 962-966 (2009).
- Ueda, H., Almeida, F. R., Chen, H., Lowe, A. A. Effect of 2 jaw exercises on occlusal function in patients with obstructive sleep apnea during oral appliance therapy: a randomized controlled trial. Am J Orthod Dentofacial Orthop. 135 (4), 430 (2009).
- Strollo, P. J., et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 370 (2), 139-149 (2014).
- Perrier, P., Payan, Y., Zandipour, M., Perkell, J. Influences of tongue biomechanics on speech movements during the production of velar stop consonants: A modeling study. J Acoust Soc Am. 114 (3), 1582-1599 (2003).
- Connor, N. P., et al. Tongue muscle plasticity following hypoglossal nerve stimulation in aged rats. Muscle & nerve. 47 (2), 230-240 (2013).
- Brady, J. P., et al. AlphaB-crystallin in lens development and muscle integrity: a gene knockout approach. Invest Ophthalmol Vis Sci. 42 (12), 2924-2934 (2001).
- Spassov, A., et al. Differential expression of myosin heavy chain isoforms in the masticatory muscles of dystrophin-deficient mice. Eur J Orthod. , ciq113 (2010).
- Lever, T. E., et al. Videofluoroscopic Validation of a Translational Murine Model of Presbyphagia. Dysphagia. 30 (3), 328-342 (2015).
- Gantois, I., et al. Ablation of D1 dopamine receptor-expressing cells generates mice with seizures, dystonia, hyperactivity, and impaired oral behavior. Proc Natl Acad Sci. 104 (10), 4182-4187 (2007).