Walk with Me Hybrid Virtual/In-Person Walking for Older Adults with Neurodegenerative Disease
Summary
The present protocol aims to inform rehabilitation specialists and fitness instructors in safe, feasible, and evidence-based methods of delivering virtual and in-person walking classes to older adults with neurodegenerative diseases.
Abstract
This study presents a protocol for virtual and in-person walking groups for older adults with neurodegenerative diseases and addresses the decline in physical activity and social connectivity during the pandemic. Physical activity, specifically moderate-intensity walking, has been shown to have multiple health benefits for older adults. This methodology was created during the COVID-19 pandemic, contributing to lower physical activity levels and social isolation in older adults. Both the in-person and virtual classes utilize technology such as fitness tracking apps and video platforms. Data are presented from two groups of older adults with neurodegenerative disease: people with prodromal Alzheimer’s disease and people with Parkinson’s disease. Participants in the virtual classes were screened for balance impairments before the walk, and any person deemed at risk for falls was not eligible to participate virtually. As COVID vaccines became available and restrictions were lifted, in-person walking groups became feasible. Staff and caregivers were trained in balance management, roles/responsibilities, and delivering walking cues. Both walks, virtual and in-person, consisted of a warm up, a walk, and a cool down, and posture, gait, and safety cues were given throughout. Measures of the rate of perceived exertion (RPE) and heart rate (HR) were taken pre-warm up, post-warm up, and at 15 min, 30 min, and 45 min time points. Participants also used a walking application (app) on their phones to record the distance walked and the number of steps taken. The study showed a positive correlation between HR and RPE in both groups. The participants in the virtual group rated the walking group favorably in terms of improving their quality of life during a period of social isolation and contributing to physical, mental, and emotional well-being. The methodology shows a safe and feasible way to implement virtual and in-person walking groups for older adults with neurological diseases.
Introduction
Older adults with neurodegenerative diseases, specifically Parkinson's disease (PD), have poor mobility, a high risk of falls, decreased quality of life (QOL), and generally decreased activity levels. More specifically, walking difficulties among older adults and people with PD are common, leading to decreased independence and increased morbidity and mortality1. Age-related changes in gait include altered gait biomechanics, slower gait speeds, and decreased coordination. In PD, bradykinesia and hypokinesia, along with timing and coordination problems, contribute to gait changes2.
In addition, older adults have been affected by the onset of the global COVID-19 pandemic in March 20203. Many countries implemented "isolation and quarantine" and "social distancing" to limit the spread of the virus. Given the high mortality and morbidity rate of older people due to COVID-19, strict social distancing and isolation rules remained in effect for older people for approximately one year until the vaccine became available. Unintended consequences of social distancing and social isolation for older adults include a marked decline in physical activity and a decreased daily step count. For example, many older adults were unable to participate in either daily functional physical activities, such as running errands and social engagements, or formal daily exercise programs for one year or longer. This trend is disconcerting given that many older adults were not achieving the recommended daily amount of physical activity pre-pandemic4.
Physical activity participation among older adults and people with PD has been widely researched and has been shown to have physical, psychological, and cognitive benefits for older adults5. Improving strength, balance, and endurance can reduce the risk of falls, enhance independence, and improve quality of life. A simple, salient, and low-cost form of exercise is walking. The guidelines for physical activity in older adults suggest 150 min of moderate-intensity exercise, such as brisk walking, per week to obtain health benefits. A heart rate of 64%-76% of the maximum heart rate or a rate of perceived exertion (RPE) between 4 and 6 on the 10-point Borg Rate of Perceived Exertion scale can be used to define moderate walking intensity6.
The method presented in this work is a hybrid in-person/virtual walking group format for older adults with and without balance impairment due to neurodegenerative disease. The increased use of online technology-based platforms and the increased technological familiarity among older adults have facilitated the use of this method. The technique was developed during the pandemic, from Summer to Fall of 2020, over several months, and the development process included holding weekly working group meetings of experts to build consensus regarding the methods. These working group meetings preceded the piloting of the method. An advantage of the hybrid method is the ability to involve older adults from distant geographical locations who are at low risk of falls (requiring less supervision) while also supervising those at higher risk of falls or other adverse events. Safety concerns are also addressed extensively in this work.
The purpose of this method is to provide guidelines, recommendations, and procedures to rehabilitation specialists and fitness instructors for the safe and feasible delivery of virtual and in-person walking classes to older adults with neurodegenerative diseases in order to improve older adult physical function and social connectivity and, thus, quality of life.
Protocol
This protocol was approved by the Emory Institutional Review Board and the Atlanta Veterans Administration Research & Development Committee. All participants signed an informed consent document prior to participation.
1. Participant recruitment
- Recruit older adults and individuals with PD and prodromal Alzheimer's disease (pAD) through flyers, registries, referrals, PD newsletters, educational meetings, webinars, support groups, older adult living communities, and websites (see Table 1 for participant information).
- Ensure the participants with PD have been diagnosed with "idiopathic" Parkinson's and positively respond to dopaminergic therapy7. Ensure that those with pAD have mild cognitive impairment with subjective memory loss.
- Confirm that participants with either PD or pAD have no other neurological insult and can ambulate 3 meters or more with and without assistance.
2. Safety training
- Train staff, instructors, care partners, and volunteers through an in-person experiential balance management class, a systematic approach to understanding balance, by presenting information about the three systems underlying balance: vestibular, visual, and somatosensory.
- Introduce principles such as the base of support, the center of gravity, and limits of stability. Perform exercises such as (1) standing while shifting to the edges of one's feet and maintaining balance, (2) closing the eyes while standing and shifting weight from foot to foot, (3) observing a partner shift their weight until the partner has to take a step and learning to use body weight to support the weight of a partner.
- Use the balance management exercises from the previously mentioned balance management class (step 2.1.1) to increase the team's ability to detect and prevent potential falls in a rehabilitative movement class.
- Provide ongoing education to staff given by the principal investigator (PI) and staff physical therapists regarding protecting participants with specific gait and balance impairments.
3. Technological considerations
- Identify and use any commercially available fitness app (see the Table of Materials) that can track time, distance, steps, pace, elevation, and other parameters needed for goal setting and to show progress.
- Identify a team meeting platform with video and sound capabilities (see the Table of Materials) for the virtual warm up.
- Use a one-tap mobile or conference call line for the virtual walk and cool down.
- Utilize heart rate monitors (see the Table of Materials) to track the heart rate throughout the walk.
- Create detailed written and picture instructions for using the fitness app, video team meeting platform, and conference call line. Email the instructions to all new participants 2 days prior to the walk day. Give technical support to all participants prior to and throughout the walks.
4. Overground walk environment
- Plan and inspect a safe outdoor walking route in terms of the convenience, safety, and appropriateness for older adults with sensory and motor impairments prior to the in-person walk in the local neighborhood, town, or near the older adult center.
- Make a note of rest spots, benches, and shade, which can be useful during the walk, any uneven surfaces and curbs, which may present safety issues, and other important environmental assets or hazards. Consider the amount of traffic in the area and the overall quality of the sidewalks and/or walking paths.
- Ensure that there is an appropriate, older adult-safe walking environment, including limited traffic, clear and even sidewalks, benches or other rest spots, shade, and mostly level ground. Some small inclines and declines may be tolerable, but check for ramps for those participants using rolling walkers.
5. Participant screening for virtual versus in-person walking groups
- Request that the participants complete a questionnaire regarding their age, education, medical history, fall history, use of assistive devices such as canes/walkers, and current medications during their initial testing session or prior to the first walk. Review the form with all the participants to ensure completeness/accuracy.
NOTE: Participants are not deemed appropriate for virtual walking classes due to safety considerations if they have a score of 4 or higher or if they answer "yes" to any of the first three key questions on the Stay Independent Screener8, if the participant scores a 2 or higher on item 3 of the New Freezing of Gait Questionnaire9, if an assistive device is used regularly, or if the participant reports falling more than once per month. - Use other fitness metrics to assess the fitness to maintain safety and to evaluate progress (e.g., heart rate monitoring, VO2 submaximal assessment, 6 min walk test, Mini Best test, and vascular function measurement using a commercially available device)10,11,12 (see the Table of Materials).
6. Schedule the participants for a walk
- Host virtual and in-person walks simultaneously with the number of staff necessary to fill the lead, co-lead, and back-marker positions, as well as any other staff needed for safety/assistance.
- Schedule the walks at a time of day that is appropriate for the group.
- Schedule the walks twice per week for 12 weeks, ensuring a minimum of 20 walks in total. After 12 weeks, invite the participants to walk once per week. The walk presented in this study was 90 min, including the warm up, walk, and cool down.
- Email the virtual walk group instructions to participants 2 days prior to the day of the walk. The instructions are below:
- Use an invitation with a link to a one-tap mobile or other video or conference call line.
- Provide new participants with instructions on how to use the technology and fitness tracking app, as well as regarding safety and appropriate attire.
7. Staff roles and responsibilities
- Group lead responsibilities
- Identify participants who have similar walking abilities before the walk. Assign back-markers/staff to participants who are deemed a high fall risk to protect them during the warm up, walk, and cool down.
- Introduce the self and the co-leader at the beginning of the session, along with other staff members. Educate the participants on the Borg Rate of Perceived Exertion (RPE) 10-point scale13, which is used to determine the participant's perceptions of their physical effort. Briefly discuss the session's agenda.
- Lead a total body warm up using cues for safety, effort, and time/repetitions.
- Monitor the remote participants during the warm up to ensure proper form, alignment, and safety.
- Motivate the participants. Tell them they are doing well if they participate. Congratulate all the participants on their efforts.
- Pay attention to the time for the warm ups, breaks, walks, and cool downs.
- Assess the participants continuously during one-tap mobile/conference call during the walk for safety, intensity, and form.
- Provide verbal cues for posture and gait mechanics (Table 2) after each RPE update and if a participant has not been heard speaking for a long period of time (to ensure we do not lose contact with a participant).
- Encourage rest and hydration breaks.
- Ask the participants about their walking environment (e.g., sidewalks, hills, etc.) and their walking form (posture). Check in with the participants frequently about safety concerns and how they can monitor and maintain good biomechanics of gait.
- Lead the cool-down after the walk on the one-tap mobile or conference call line.
- Answer any questions regarding the technology, walking form, intensity, goals, etc.
- Take over responsibilities if the co-leader becomes disconnected for any reason.
- Co-lead responsibilities
- Email the participant information and instructions for the fitness tracking app and team meeting links to all the participants 2 days prior to the walk.
- Take attendance at the start of the meeting. If a participant is not in attendance, call the participant to check on them.
- Assist the participants with the use of technology during the practice team meeting video calls.
- Assist the participants during the transition between the video call and the one-tap mobile call during the 5 min break.
- Assist the participants with the setting up, usage, and starting/stopping of the fitness tracking app.
- Ask and record the participants' RPE and heart rates pre-warm up, post-warm up, and at the 15 min, 30 min, and 45 min time points of the walk.
- Manually record the RPE, heart rates, steps, distance walked, elevation, and average pace for the participants at the 45 min time point of the walk.
- Enter the data into any commercially available database survey software immediately or as soon as possible after collecting the data.
- Take over group leader responsibilities should the group leader become disconnected from the call for any reason.
- Back-marker/other staff responsibilities
- Ensure all the participants' safety, particularly for the participants who have slower walking speeds, use an assistive device, or have a heightened fall risk, postural instability, or freezing of gait. Staff may be paired one-on-one or even two-on-one with participants who have been deemed a high fall risk.
- Ensure participants are walking along the same route and no participants become lost on the route. Watch for traffic carefully, and alert the group to oncoming traffic.
- Assist with any additional responsibilities as requested by the group leader or co-leader.
- Socialize with the participants during the walk.
8. Virtual and in-person walk: Preparation steps
- Virtual walk procedure
- At 15-20 min prior to the class time, log into the video team meeting. Educate new participants on the RPE scale. Lead a warm up for 25 min. Take the RPE pre- and post-warm up (co-leader).
- The warm up is performed by the group leader with whole-body large-amplitude movements incorporating posture, weight shifting, rotation, and stepping. Lead the warm up in both seated and standing positions with cues for safety, effort, amplitude, and form. Verbally ensure the safety of the participants.
- Implement a break for 5 min to prepare the participants for the walk. Assist the participants in logging on to the approved fitness tracking app and one-tap mobile or other conference call line.
- Instruct the participants in proper posture and gait mechanics after every RPE check-in and through the walk. See Table 2 for a complete list of cues. Ask the participants to be mindful of their environments and to describe their surroundings.
- Limit the walking group to four to six participants. Strongly encourage the participants to bring a caregiver or a walking buddy to their walks. Discuss with the participants the location and terrain of the walks prior to the first walk to ensure safety and familiarity with the chosen area.
- Take and record the participant's RPE at 15 min, 30 min, and 45 min.
- Ask the participants to stop their fitness tracking app after 45 min and participate in a 5-10 min guided cool down from the instructor delivered through the audio function.
- In-person walk procedure
- Arrive at an established walking location wearing a mask. Screen the participants for COVID-19, and assist with wearable HR and fitness tracking technology. Educate new participants on the RPE scale and agenda.
- Lead a warm up with whole-body large-amplitude movements incorporating posture, weight shifting, rotation, and stepping. Lead both seated and standing exercises with cues for safety, effort, amplitude, and form. Have an assigned staff member protect the participants with balance impairments to ensure their safety.
- Record the RPE and HR pre- and post-warm up.
- Implement a break for 5 min to prepare the participants for the walk. Assist the participants in starting the walking app technology.
- Divide the walking group into smaller groups based on speed, ability, and fall risk. Assign each walking group a leader, a back-marker, and/or other study staff, with one person in each group remaining on the audio call. The leader of the group with the greatest walking mobility leads the virtual walking group.
- Record the RPE and HR at the 15 min, 30 min, and 45 min time points.
- Give posture and gait cues at the beginning of the walk at 15 min, 30 min, and 45 min. Safety is of the utmost importance. Participants who are considered a high fall risk will have at least one person walking with them for safety and guarding. These individuals should be closely monitored for fatigue. Give cues for environmental hazards and encourage rest breaks and the use of assistive devices.
- Ask the participants to stop their walking app at the 45 min time point and participate in a 5-10 min guided cool down.
- Administer a satisfaction questionnaire intermittently (approximately every 10 classes) to determine the level of enjoyment the participants are experiencing.
9. Participant post-evaluation
- Measure the chosen fitness metrics, as noted in step 5.2, to determine the change in the participants' fitness over the course of the walking program.
- Administer a participant satisfaction survey.
Representative Results
Pilot virtual walking group
During COVID-19, an expert working group of seven individuals created and implemented the virtual walking protocol with eight pilot participants. The working group consisted of a PI, a physical therapist, an exercise physiologist, a lab manager, two research study coordinators, and a graduate student. The working group met virtually every week to form a consensus on the methods preceding the pilot of the methods. To pilot the methods, participants from the PD and older adult community were asked to join. Four of the virtual walkers had a diagnosis of PD, and four of the walkers were older adults with no known neurodegenerative disease diagnosis. The virtual pilot walks took place twice per week over a 4 month time frame. Participants were invited to attend any walk during the week. The participant attendance per walk was not recorded at the time, but we had a zero attrition rate during the 4 months of piloting the virtual walk, with no known adverse events. The heart rate and RPE were not measured during this time. The goal of the pilot program was to see if the methodology was feasible and effective in increasing physical activity and social connectivity with the use of technology during the pandemic quarantine. Participant satisfaction surveys were taken at the end of the 4 months (Table 3).
Hybrid virtual/in-person group
As the quarantine measures ended and the COVID-19 vaccine became readily available, in-person walking groups were formed specifically for people at a higher risk for falls and/or who preferred in-person instruction. The pilot participants were invited to continue to join the virtual group weekly. Generally, the enrollment for the virtual and in-person groups was rolling and continuously open, with walking groups being offered five days per week, and each participant walking two times per week for a target goal of 20 walks over a three-month time frame. The in-person and virtual groups included older adults with PD and older adults with pAD. The in-person walking group included people of all mobility levels, from independent ambulators to those requiring assistance due to balance and gait impairments. The virtual group included only participants deemed eligible based on the fall risk screening process.
At the time of authoring this paper, the in-person walking group has six people with PD and four people with pAD, with the expectation for growth as more participants are randomized into the walk intervention of the study. Of the original eight virtual pilot participants, seven are no longer participating due to illness, job obligations, and other personal reasons. For the in-person group, three of the six participants with PD required one-on-one supervision from a trained staff member. Two participants with PD were interested in virtual groups; however, neither of these participants qualified for the virtual walking group due to the high risk for falls. The remaining three of the six participants with PD and all four of the participants with pAD qualified as a low fall risk and, therefore, could walk with less supervision from staff. These seven low-risk participants chose the in-person walking group over the virtual group for unknown reasons. One to two staff members, in addition to the group leader and co-leader, were assigned to the low-fall risk group to monitor for safety and assist the group leader if needed. Typically, the group leader leads virtual participants and the low-fall risk group. All staff assisting with the walk are connected to the group leader and co-leader via a one-tap mobile or conference call line for the duration of the walk. There are 11 total staff members available to support these walks and assigned to walks according to the number of participants who sign up each week. The staff members included research coordinators, physical therapists, personal trainers, exercise physiologists, and graduate students. Additional staff were added over time as the walking group increased in participant size. New staff members were oriented and trained on an informal one-on-one basis by the PI and the staff physical therapist and by the formal balance management training class, as described in the protocol section above. The data presented below were collected from 10 participants with PD or pAD participating in person in walking groups who attended between 4 and 15 classes, at the time of this paper. The demographics and clinical characteristics table (Table 1) shows participants were about 70 years old and relatively highly educated (16-17 years of education). The PD participants had fallen more often in the previous six months compared to the pAD participants. More PD participants used an assistive device and were more afraid of falling than the pAD participants. At the time of this paper, there were no adverse events to report.
Heart rate, RPE, and distance outcomes
As stated in the methods, the heart rate/RPE data from each participant were collected during the in-person walks at five different time points throughout the class: baseline, after the warm up, 15 min, 30 min, and 45 min. At the end of the walk, the distance traveled during the walk was also collected.
The heart rate and RPE of the participants increased over the course of the walk, and people with PD had more variable RPE than those with pAD (Figure 1 and Figure 2). Furthermore, there was a strong positive correlation between RPE and heart rate (Figure 3). A correlation was found between the low RPE scores and HR when the participants were walking at a low to moderate intensity of 50%-75% of their max HR. During these walks, people with PD walked 1,800 m on average, and people with pAD walked 3,000 m on average (Figure 4).
A satisfaction survey was distributed among the pilot virtual participants. These participants were people with PD and with no other known neurological disorder. Five participants responded from a total out of eight consistent walkers who had been with the program over a 4 month time frame. Overall, the program was well-received (Table 3). All members of the group strongly agreed that walking improved their quality of life, motivated them to exercise, contributed to physical well-being, contributed to mental well-being, and that they would recommend the program to a friend or family member. Most participants found the group to be physically challenging. However, a few were neutral or disagreed, possibly due to the nature of the virtual walk. Although participants were verbally cued for intensity ranges based on RPE, ultimately, the pace and route were self-selected by the participant.
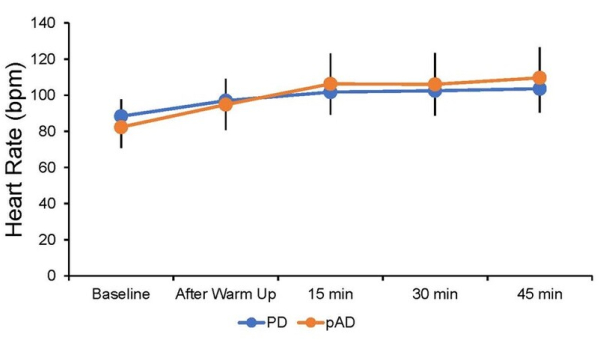
Figure 1: Average heart rates of the PD and pAD participants over the in-person walk. Data collected from multiple in-person sessions for individual participants who attended between 2 and 20 classes. Heart rates were collected at five different time points throughout the class: baseline, after warm up, 15 min, 30 min, and 45 min. Depicted are the average heart rates (± SD) separated by group into individuals with PD (blue; n = 6) and individuals with pAD (orange; n = 4) at each of these time points, with n = 45-57 HR per time point per group. Please click here to view a larger version of this figure.
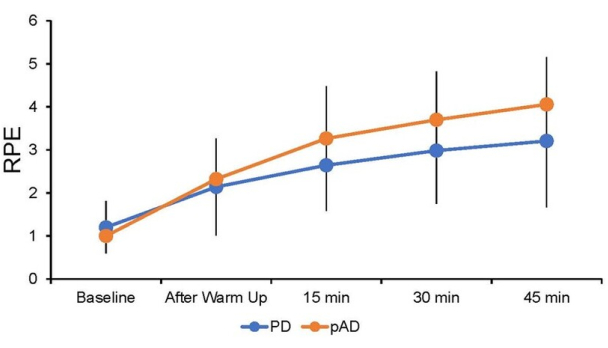
Figure 2: Average rates of perceived exertion (RPE) of the participants during the in-person walk. Data collected from multiple in-person sessions for individual participants who attended between 2 and 20 classes. The RPE was collected at five different time points throughout the class: baseline, after warm up, 15 min, 30 min, and 45 min. Depicted are the average RPEs (± SD) separated by group into individuals with PD (blue; n = 6) and individuals with pAD (orange; n = 4) at each of these time points, with n = 50-59 per time point per group. Please click here to view a larger version of this figure.
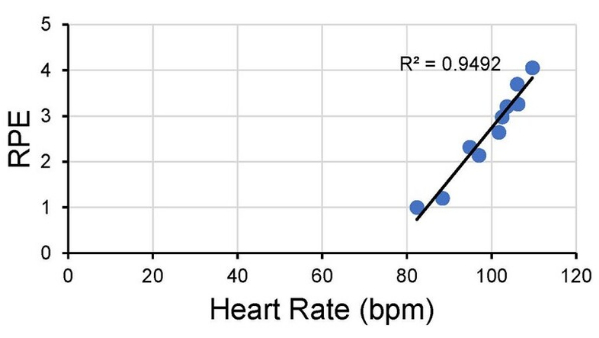
Figure 3: Correlation between the average RPE and heart rate for the different time points over the in-person walk. The average heart rate and average RPE were calculated for the five different time points throughout the in-person walking class and for each group (PD and pAD). These values were then correlated, and an R-squared value was calculated. Please click here to view a larger version of this figure.
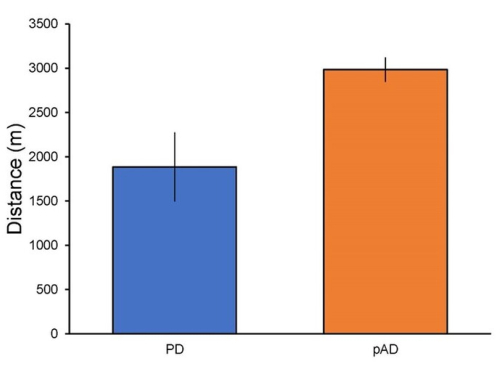
Figure 4: Average distance walked by people with PD and people with pAD in the in-person walk. Depicted is the average distance that the participants walked during the 45 min walking part of the class separated by clinical group (PD: n = 58; pAD: n = 53). This average includes multiple sessions for individual participants who attended between 2 and 20 classes. Please click here to view a larger version of this figure.
Table 1: Demographics table for participants with PD and pAD for the virtual versus in-person walking groups. Please click here to download this Table.
Table 2: Examples of posture and gait cues. Several possible posture and gait cues given at baseline, 15 min, and 30 min of the virtual and in-person walk are presented. Please click here to download this Table.
Table 3: Satisfaction survey. Representative satisfaction survey responses from the original eight virtual walk participants. For example, five out of five of the responding participants strongly agreed that the virtual walk group improved their quality of life. Five out of eight participants responded to the survey. Please click here to download this Table.
Discussion
The methods detailed above describe a safe and feasible way to implement a low-cost, salient, over-ground walking program for older adults with neurodegenerative diseases1,2. The virtual classes were shown to be effective in contributing to physical and mental well-being and quality of life during a period of social isolation due to COVID-193. Once the quarantine measures were lifted and COVID-19 vaccines became readily available, the participants in this study favored in-person walking over virtual walking. The few participants requesting the virtual walk group were ineligible due to a high risk for falls and/or a history of falls. Of the original eight pilot participants, only one continued to walk virtually at the time of this paper. The other seven participants were unable to continue walking virtually due to various reasons, such as returning to work, family obligations, surgery, and the time of day of the walks.
Overall, the protocol and methods for the hybrid virtual/in-person walking group for older adults with neurodegenerative diseases were feasible, safe, and effective. In utilizing simple technology for communication and physical activity tracking, the older adults in this study increased their physical activity and social connectivity during a time of social distancing and isolation. Critical steps in the protocol include identifying which participants are appropriate for in-person versus virtual walking based on fall risk scores and fall history. Healthy older adults with no known fall risk or history are more suitable for the virtual walking group, whereas people with neurodegenerative diseases may be more appropriate for an in-person supervised walking group. Onboarding and educating the virtual and in-person walk participants in the use of technology was feasible in this study with additional help from caregivers and staff, as well as with the step-by-step instructions in the emailed information packet that was sent prior to the walk. Most participants needed one or two demonstrations of the technology before learning it. A few of the participants needed ongoing assistance with the fitness tracking app, which takes about two min to set up. A few participants began using the fitness app to track activity outside of the walking group. Planning a safe walking route and walking with a buddy is also important to ensure the success of the virtual walking program. Lastly, training staff and caregivers/walk buddies on the principles of balance management and fall prevention is of utmost importance in this protocol to ensure the safety of the in-person walk participants.
The fast growth of a group with varying ability levels presented a few challenges that led to considerations that need to be addressed before starting a walking group. The first consideration is having enough staff available to lead a faster-paced in-person walking group in addition to the virtual group and several small groups or one-to-one pairings. The staff for this program are on a research team at a large university. This team has research coordinators, a physical therapist, a personal trainer, an exercise physiologist, graduate students, and undergraduate student volunteers that work together. For smaller programs, community volunteers, students, and caregivers can be trained in balance management and the walking protocol in order to satisfy safety needs. Perhaps a more feasible method for smaller programs to implement this protocol would be to divide the participants by ability level. The low-fall risk participants and virtual groups will require fewer staff and volunteers. The high-fall risk group may need to be generally smaller to ensure a one-to-one ratio of staff to participants for safety. Another consideration that presented itself relates to the chosen method for monitoring the heart rate via a chest strap and an app on an iPad. The participant must be within a certain range of the iPad for accurate monitoring. Using smartwatches with heart rate monitoring capabilities for participants instead of chest straps is a workable solution to ensure that all the participants' heart rates are monitored correctly.
Strengths and limitations
There are several strengths to this study. After several months of piloting and working with participants with various walking abilities, the methods for delivering hybrid virtual and in-person walking groups for older adults with neurodegenerative disease now have robust quality. In fact, the program was developed in codesign with several older adults and with people with Parkinson's disease. The piloting went on for several months. First, we worked things out with study staff and graduate students and then invited participants from previous studies who had connections with the lab to join us for walks so that we could test out these new methods. Some older adults from other cities and states also participated. These methods would translate well for the general older adult population, as well as other conditions beyond PD and pAD, and to encourage physical activity, increase social connectivity, and, therefore, enhance quality of life in a community exercise setting. For some older individuals, a program like this could have a very positive impact on loneliness and mood.
Several factors possibly affected the results of the study, and these are, therefore, limitations of the study. First, the RPE data showed that the participants reported low RPEs. Whereas the goal for participants is to work in the 4-6 range of RPE, the participants reported 3 and lower sometimes, on average. These low numbers could be due to the participants' lack of understanding of the RPE scale, inability to recall the scale accurately over a 45 min period, or social suggestions based on the first number given by another participant. Additionally, participants with PD may have a sensorimotor perceptual mismatch; in this case, the perception of effort does not match the speed or work output. To address this, the RPE scale is reviewed prior to each walk, individual cues are given to participants to increase their speed and effort, and the walking route may be changed to incorporate more difficult terrain, such as hills. The participant's self-selected gait speed over ground may contribute to low RPE and HR. People with PD and significant gait impairments may be unable to increase their heart rate to moderate intensity, thus affecting their RPE14. Although this methodology provides little control over participants' walking speed and intensity, the benefits of an organized walking program on physical activity levels and quality of life are positive. In addition, the benefits of overground walking with environmental demands are greater than those of using a treadmill or other such stationary equipment, as overground walking may be better for speed and intensity control, saliency, and real-life applicability.
In summary, the hybrid remote and in-person walking program described here may be useful nationwide for older adults both with and without movement impairments. In addition, decreased social networks and loneliness could be addressed using this program.
Divulgaciones
The authors have nothing to disclose.
Acknowledgements
We acknowledge our participants and the experts with whom we consulted on the methodology developed in this walking program.
Materials
| Chest strap heart rate monitor | Polar | NA | |
| Computer with video/sound | NA | ||
| Fitness tracking app | Any commercially available app | NA | |
| iPAD | Apple IPAD | NA | |
| Pressure management device | Atcor Medical, Australia | SphygmoCor | |
| Smartphone | Apple or Android | NA | |
| Standard chair | NA | ||
| Team meeting platform | Zoom | NA |
Referencias
- Brach, J. S., Vanswearingen, J. M. Interventions to improve walking in older adults. Current Translational Geriatrics and Experimental Gerontology Reports. 2 (4), (2013).
- Mirelman, A., et al. Gait impairments in Parkinson’s disease. Lancet Neurology. 18 (7), 697-708 (2019).
- Lopez, J., Perez-Rojo, G., Noriega, C., Martinez-Huertas, J. A., Velasco, C. Longitudinal impact of the COVID-19 pandemic on older adults’ wellbeing. Frontiers in Psychiatry. 13, 837533 (2022).
- Cunningham, C. Why physical activity matters for older adults in a time of pandemic. European Review of Aging and Physical Activity. 17, 16 (2020).
- Chodzko-Zajko, W. J., et al. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Medicine and Science in Sports and Exercise. 41 (7), 1510-1530 (2009).
- Target Heart Rate and Estimated Maximum Heart Rate. Centers for Disease Control and Prevention Available from: https://www.cdc.gov/pysicalactivity/basics/measuring/heartrate.htm#:~:text=For%20moderate%2Dintersity%20physical%20activity (2022)
- Frank, C., Chiu, R., Lee, J. Parkinson disease primer, part 2: Management of motor and nonmotor symptoms. Canadian Family Physician. 69 (2), 91-96 (2023).
- Stay Independent: Learn More about Fall Prevention. Centers for Disease Control and Prevention Available from: https://stacks.cdc.gov/view/cdc/53418 (2017)
- Giladi, N., et al. Validation of the freezing of gait questionnaire in patients with Parkinson’s disease. Movement Disorders. 24 (5), 655-661 (2009).
- Gill, T. M., DiPietro, L., Krumholz, H. M. Role of exercise stress testing and safety monitoring for older persons starting an exercise program. Journal of the American Medical Association. 284 (3), 342-349 (2000).
- Steffen, T. M., Hacker, T. A., Mollinger, L. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Physical Therapy. 82 (2), 128-137 (2002).
- Magnani, P. E., et al. Use of the BESTest and the Mini-BESTest for fall risk prediction in community-dwelling older adults between 60 and 102 years of age. Journal of Geriatric Physical Therapy. 43 (4), 179-184 (2020).
- Borg, G. . Borg’s Perceived Exertion and Pain Scales. , (1998).
- Sabino-Carvalho, J. L., Teixeira, A. L., Samora, M., Daher, M., Vianna, L. C. Blunted cardiovascular responses to exercise in Parkinson’s disease patients: Role of the muscle metaboreflex. Journal of Neurophysiology. 120 (4), 1516-1524 (2018).

