Use of Crystal Violet to Improve Visual Cytopathic Effect-based Reading for Viral Titration using TCID50 Assays
Summary
This protocol shows an accurate and objective approach to visualize viral titrations using crystal violet, by comparing it with optical microscopy and immunocytochemical staining.
Abstract
Viral titration is a key assay for virology research. The detection of cytopathic effect (CPE) via TCID50 assays and plaque-forming units (PFU) assays are the two main methods to calculate the titer of a virus stock and are often based on microscopy detection or cell staining for visualization. In the case of TCID50 assay, objective visualization is commonly based on immunocytochemical (ICC) staining of intracellular virus to calculate titers combined with visual CPE detection via microscopy. However, ICC staining is costly and time consuming. In this study, we compared visual CPE observation via microscopy, ICC staining and crystal violet staining to determine the titers of two CPE-forming viruses, Influenza A virus (IAV) of swine origin and Porcine Reproductive and Respiratory Syndrome virus (PRRSV). We show that both crystal violet and ICC staining are more accurate than visual CPE detection, presenting nearly identical levels of precision on both IAV and PRRSV. For this reason, here we present crystal violet staining as a faster and more affordable way to determine viral titrations on a TCID50 assay for CPE-forming viruses titrated in cell lines.
Introduction
Viral titration via TCID50 assay is a commonly used technique in infectious disease research1. Although variations on the math behind this method have been proposed over time1,2,3,4, the currently applied methods of infection detection rely on visual confirmation through the presence of cytopathic effect (CPE) using microscopy5. To confirm CPE visualization more objectively on TCID50 assays, immunocytochemical (ICC) intracellular staining targeting the proteins of the virus is one of the most-commonly used methods6 as different viruses can produce varying forms of CPE. In our case, the cell morphological changes are similar when infected with both Influenza A virus (IAV) and Porcine Reproductive and Respiratory Syndrome Virus (PRRSV), where infected cells round up and detach from the plate. In the case of PRRSV, it causes a CPE known as "total destruction", where all cells end up detaching from the well. IAV on the other hand, can present both total destruction and an additional CPE known as "subtotal destruction" where a small number of cells do not detach after infection7. However, this technique is time consuming to perform and requires the use of relatively costly reagents. It is important to note that ICC does not label CPE, but rather the number of cells successfully infected by the virus. This implies that the cells that were successfully infected by the end of the incubation will be seen as positive even if the infection has not caused CPE yet, and thus, a higher percentage of ICC positive cells compared to CPE is expected. For that reason, in this study we describe a complementary method of visual detection of CPE in a TCID50 assay based on crystal violet, a chemical with a positive charge that attaches to cell membranes and is used to stain adherent cells. Crystal violet is often utilized in virology research to measure plaque-forming units, among others8.
In this study, we compare the sensitivity of non-stained microscopy CPE detection with crystal violet staining and immunocytochemical staining based on viral protein recognition, which is known to be more objective due to its high sensitivity. This study shows that both crystal violet and immunocytochemical staining are more accurate than visual microscopy-based CPE detection and can be used to objectively identify infected wells in a TCID50 titration. Given their ability to reach nearly identical level of accuracy on the cytopathic viruses tested in cell lines, crystal violet is presented as a faster and more affordable way to determine viral titrations on a TCID50 assay. The proposed method using crystal violet staining takes a total time of 40 min to perform, with 15 min for paraformaldehyde (PFA) incubation, 5 min for crystal violet incubation and a maximum of 15 min for material preparation, buffer washes, and drying. The immunocytochemistry protocol applied for comparison takes an average time of 4 h 30 min and was performed as previously described9,10. The method proposed aims to help visualize a completed viral titration. Infection and incubation times can be performed with different layout depending on the virus. Here we tested two RNA viruses with cytopathic effect on cell lines.
Protocol
1. Titration protocol
NOTE: Use a cytopathic virus infecting adherent cells. For this demonstration, Influenza A Virus (IAV) of swine origin (A/California/07/2009/(H1N1)) and Porcine Reproductive and Respiratory Syndrome Virus (PRRSV) Type 2, strain NC 1-7-4 were used.
- Titrate these viruses in 96 well plates for 7 days in a biosafety cabinet located in a Biosafety Level 2 (BSL-2) laboratory.
- To perform these titrations, seed 96 well plates with the required cell line. For PRRSV, use MA-104 cell line and for IAV use MDCK cell line. For the cell culture, use DMEM medium supplemented with 10% FBS, L-Glutamine and Penicillin-Streptomycin and grow the cells to confluency.
- Before infection, wash the cells using 200 µL of PBS.
- Dilute the virus stocks using 10 fold dilutions series by mixing 900 µL of media and 100 µL of virus. Make sure to properly vortex the tube to ensure proper mixing of the medium and virus and to avoid dilution errors.
- Mark the layout of the plate on the lid. Wash the wells with 1x phosphate saline buffer (PBS). Add 50 µL of the inoculum in the corresponding wells following previously described titration methods2,3.
- Incubate at 37 °C in a 5% CO2 incubator for 7 days.
2. Cytopathic effect (CPE) assessment via microscopy
- After the 7-day incubation, wash all wells with 200 µL of 1x PBS twice.
- Assess all wells of the plate under a light microscope to visually detect CPE. In the case of both PRRSV and IAV, their CPE consists of cell death and subsequent detachment from the plate, leading to monolayer disruption. However, other viruses may present different types of CPE.
3. Staining protocol
NOTE: Cytopathic effect (CPE) was assessed via crystal violet staining.
- After the 7-day incubation, wash all the wells using 200 µL of 1x PBS twice.
- Fix the cells by adding 50 µL/well of 4% paraformaldehyde (PFA) in 1x PBS and incubate for 15 min at room temperature (RT).
- After incubation, wash the cells twice with 200 µL of 1x PBS. Then, add 50 µL/well of crystal violet diluted to 4% in water and incubate for 5 min at RT.
NOTE: Crystal violet chemical stains the cells that remain attached to the plate at the time of fixation, leaving the sections of the well where the cells detached as unstained. - Finally, aspirate crystal violet from the wells and optionally leave the plates to air dry for 2-5 min at RT or wash the plate with 200 µL of water to remove excess stain prior to visualization.
- Use previously described methods to mathematically calculate the titer. Here, Karber formula and Muench formula were applied for PRRSV and IAV, respectively2,3. Details of these equations are presented in the representative result section.
4. Immunocytochemical (ICC) labeling
NOTE: Immunocytochemistry labeling for both viruses was performed following previously described methods9,10,11.
- After the 7-day incubation of the titration, fix the cells using PFA as described in step 3.2.
- Wash the plates with a solution composed by 100 mL of 1 M Tris hydrochloride, 1 g of Saponin, and 8.5 g of NaCl in 900 mL of H2O. Then, complete two additional washes with a mixture of 1x PBS and 5% Fetal Bovine Serum (FBS) and incubate with that Tris-Saponin-NaCl solution at Room temperature (RT) for 20 min.
- Incubate all the wells with the primary antibody for 2 h at RT.
NOTE: The volume of primary antibodies for each virus was 100 µL and was prepared using a 1:300 dilution of 2% FBS in 1x PBS. - Wash the cells twice with the Tris, Saponin, and NaCl solution prepared in step 4.2.
- Incubate all the wells with the secondary antibody for 1 h at RT.
NOTE: The volume of secondary antibody was 100 µL and was prepared using a 1:250 dilution of 2% FBS in 1x PBS. - Wash the cells with the Tris, Saponin, and NaCl dilution as described in step 4.2.
- Aspirate the previous dilution and incubate the plates with 200 µL/well of aminoethyl carbazole (AEC) solution at a final dilution of 1:50 in water following the manufacturer's directions for 30 min at RT.
- After incubation, discard the AEC solution and add 100 µL/well of 1x PBS for imaging via microscopy.
- Mathematically derive the titer as described in step 3.5.
Representative Results
The equations used for mathematically calculating the titer were previously described2,3.
Briefly, for PRRSV, we apply the Karber method:
Titer (TCID50) = 10 T + 1.3 where:
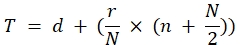
In this formula d = negative log of the last dilution with complete positive virus response: five positive replicates; r = log of dilution range; N = number of replicates by dilution; n = number of wells with positive virus response on the next dilutions.
In the case of IAV, we use the Muench formula:
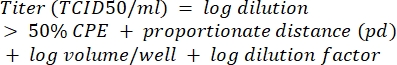
For details on each mathematical method, refer to Ramakrishnan et al., (2016) and Reed et al., (1938)2,3.
As a visual example, the titer obtained for PRRSV shown in Figure 1 would be calculated as follows:
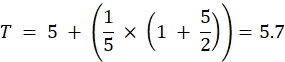
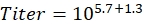
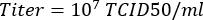
The number of positive wells obtained when ICC (left half of the plate) and Crystal Violet staining (right part of the plate) were compared was highly similar for both PRRSV (Figure 1) and IAV (Figure 2) and was in both cases able to detect between one and two positive wells more than the CPE observed prior to staining through microscopy, even though these differences were not statistically significant (Table 1). While the output obtained from crystal violet staining is usually a positive-negative well, using ICC there is a gradual decrease on the number of positive cells that get labeled as the virus gets more diluted. Furthermore, ICC requires the use of a microscope for visualization, while crystal violet can be easily performed by eye.
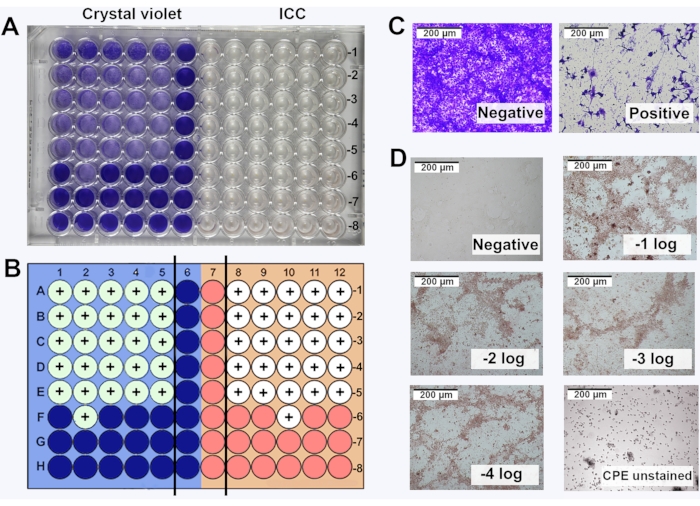
Figure 1: Comparison of crystal violet staining and immunocytochemical labeling (ICC) for PRRSV titration. (A) Visualization of the titration plate by eye, with the left-half corresponding to crystal violet staining and right-half corresponding to ICC; (B) Schematic representation of the plate with positive wells indicated with a '+' sign using crystal violet and ICC; (C) Microscopy image (10x objective) of crystal violet staining; (D) Microscopy image (10x objective) of positive wells detected by ICC. Ten-fold dilutions of the virus from -1 to -8 log. were performed. Images of positive wells from -1 log to -5 log. Uninfected cells were used as negative control (referred as negative). Please click here to view a larger version of this figure.
Figure 2: Comparison of crystal violet staining and immunocytochemical labeling (ICC) for IAV titration. (A) Visualization of the titration plate by eye, with the left-half corresponding to crystal violet staining and right-half corresponding to ICC; (B) Schematic representation of the plate with positive wells indicated with a '+' sign using crystal violet and ICC; (C) Microscopy image (10x objective) of crystal violet staining; (D) Microscopy image (10x objective) of positive wells detected by ICC. Ten-fold dilutions of the virus from 10-1 to 10-8. were performed. Images of positive wells from -1 log to -5 log. Uninfected cells were used as negative control (referred as negative). Please click here to view a larger version of this figure.
Table 1: Comparison of the titers obtained for both PRRSV and IAV using the three visualization approaches. Titers expressed as the average ± SEM of the log10 TCID50/mL in n = 5 replicates. No statistically significant differences were found between the groups (p > 0.05). Please click here to download this Table.
Discussion
Viral titrations are routinely used in virology research, with PFU detection and TCID50 assays most commonly used1,2,3,4. Both methods rely on the detection of CPE in infected cells, and even though they can be visually assessed via microscopy, a staining is usually applied to obtain a more objective result or to even reduce incubation times. In the case of TCID50, one of the most commonly used alternatives to visual CPE detection that offers an accurate and objective measure is ICC staining6, which is time consuming and often expensive due to the utilization of specific antibodies9,10. However, even though this type of assay also benefits from the application of crystal violet staining for visualization, there are no comparative studies assessing the differences in sensitivity between ICC and crystal violet staining. Thus, the protocol proposed here is a suitable option for TCID50-based viral stock titrations, as the application of crystal violet showed a comparable level of accuracy to the sensitive immunocytochemical intracellular staining targeting specific virus protein. This method is less time consuming, generally easier to execute and more accurate than CPE detection via microscopy, demonstrating that this approach is beneficial to use for virus titrations that are performed on a regular basis.
The critical steps for this crystal violet staining are a proper fixation of the cells after the 7-day incubation period for the titration and the application of enough crystal violet to cover the entire surface of the wells. To achieve successful staining, ensure that non-infected cells were properly covered with crystal violet, and that all wells are stained. This indicates that the cells were healthy, and the protocol worked as expected.
In conclusion, the utilization of crystal violet staining is proposed as a faster and less costly alternative for the objective detection of CPE on TCID50 assays, with similar accuracy to the specific ICC intracellular labeling commonly applied during this type of titration. However, there may be cases where the pathogen-specific antibodies are able to detect positive wells that would go undetected by our crystal violet method, since ICC positives will show successfully infected cells, even before the infection leads to CPE. Therefore, even though we did not find significant differences between the two, it is strongly recommended to test both methods to assess the level of sensitivity in each virus titration to determine potential differences and subsequent adjustments before using this staining routinely.
Divulgaciones
The authors have nothing to disclose.
Acknowledgements
Authors would like to acknowledge Dr. Frank Scholle for his helpful comments in the manuscript, Chloe Mariant for her help with the microscopy images and Teresa M. Tiedge for her helpful English revision.
Materials
| 96-well cell culture plates | Genesee | 25-221 | Clear, flat bottom |
| AEC solution | Thermo Fisher | 1122 | |
| Crystal violet | Thermo Fisher | C581-25; C581-100 | |
| DMEM | Corning | 10-017-CV | |
| Fetal bovine serum | BioWest | S1480 | |
| Paraformaldehide | Thermo Fisher | J19943 | |
| Primary Influenza Antibody | Bioss | BS-0344R | |
| Primary PRRSV Antibody | Bioss | BS-10043R | |
| Saponin | Thermo Scientific | AAA1882014 | |
| Secondaty antibody | Invitrogen | 31460 | |
| Tris Hydrochloride | Thermo Scientific | AM9856 |
Referencias
- Kärber, G. Contribution to the collective treatment of pharmacological series experiments. Naunyn-Schmiedeberg’s Archive for Experimental Pathology and Pharmacology. 162 (4), 480-483 (1931).
- Ramakrishnan, M. A. Determination of 50% endpoint titer using a simple formula. World Journal of Virology. 5 (2), 85-86 (2016).
- Reed, L. J., Muench, H. A simple method of estimating fifty per cent endpoints. American Journal of Epidemiology. 27 (3), 493-497 (1938).
- Spearman, C. The method of right and wrong cases (constant stimuli) without Gauss’s formulae. British Journal of Psychology. 2 (3), 227 (1908).
- Darling, A. J., Boose, J. A., Spaltro, J. Virus assay methods: accuracy and validation. Biologicals. 26 (2), 105-110 (1998).
- Kim, J., Chae, C. A comparison of virus isolation, polymerase chain reaction, immunohistochemistry, and in situ hybridization for the detection of porcine circovirus 2 and porcine parvovirus in experimentally and naturally coinfected pigs. Journal of Veterinary Diagnostic Investigation. 16 (1), 45-50 (2004).
- Suchman, E., Blair, C. Cytopathic effects of viruses protocols. American Society of Microbiology. , (2007).
- Karakus, U., Crameri, M., Lanz, C., Yángüez, E. . Influenza Virus. , 59-88 (2018).
- Tingstedt, J. -. E., Nielsen, J. Cellular immune responses in the lungs of pigs infected in utero with PRRSV: an immunohistochemical study. Viral Immunology. 17 (4), 558-564 (2004).
- Guarner, J., et al. Immunohistochemical and in situ hybridization studies of influenza A virus infection in human lungs. American Journal of Clinical Pathology. 114 (2), 227-233 (2000).
- Nicholls, J. M., et al. Detection of highly pathogenic influenza and pandemic influenza virus in formalin fixed tissues by immunohistochemical methods. Journal of Virological Methods. 179 (2), 409-413 (2012).

