Using an Automated Hirschberg Test App to Evaluate Ocular Alignment
Summary
We present a protocol of using a smartphone app to perform Hirschberg test for measuring manifest and intermittent ocular misalignment (strabismus) under near and far fixation conditions.
Abstract
A smartphone app has been developed to perform the automated photographic Hirschberg test for objective measurement of ocular misalignment. By computing the difference in corneal reflection generated by the phone camera flash relative to the iris center based on high resolution images, the app can measure misalignment with a much higher precision than the naked eye performing the Hirschberg test. It has been validated in a previous clinical evaluation study by comparing to the clinical gold standard-prism and alternate cover test. The goal of this article is to describe the testing techniques regarding how to use the app to measure ocular alignment for different fixation distances, without or with cover to break fusion, as well as angle kappa, so that users can use the app to perform equivalent tests typically done in clinic using prisms.
Introduction
Measurement of eye alignment is frequently performed in vision care clinics. Cover test with prism neutralization is the commonly used clinical method for quantifying the degree of eye misalignment (strabismus). This method requires a high degree of training and experience. Accurate measurement becomes more challenging when patients cannot fully engage in the exam such as young children1, individuals with brain injuries or stroke2, or developmental disabilities3. Furthermore, there is a need for ocular alignment testing in school screening, because strabismus develops during childhood in an estimated 5−8% of the US population4, and is a substantial risk factor for amblyopia with about 30−40% of cases of amblyopia attributed to strabismus5,6,7. However, school nurses are normally not trained to conduct the standard cover test with prism neutralization for such screening. For non-eye care professionals, an additional challenge in strabismus screening is that intermittent strabismus (misalignment is not always manifested) and smaller magnitudes of misalignment are not visually obvious (<15 prism diopters [Δ])8.
In an attempt to address the challenges in the detection and measurement of strabismus, we have developed a smartphone app (EyeTurn) that implements and automates the photographic Hirschberg method9 by comparing the displacement of corneal reflections between the eyes. While conventional photographic Hirschberg method has been shown to have good reproducibility in clinics10,11, the cost for dedicated, standalone devices is a barrier for wide adoption. By providing an easy-to-use tool to measure eye alignment with standard smartphones, we hypothesize it will be widely adopted in school vision screening and used by non-eye care professionals. Our previous evaluation studies have shown that the app measurement is consistent with the current clinical standard of prism and alternate cover test12, for strabismus magnitudes of esotropia and exotropia up to 60Δ. In a pilot school screening study, we also showed that the app can help the school nurse detect children with intermittent exotropia who were missed by standard school vision screening protocols13.
The iOS version of the app is currently available to researchers and clinicians upon request for research purposes. The requesters have thus far included school nurses, pediatric ophthalmologists, optometrists, neuro-ophthalmologists, and strabismus specialists. The purpose of this article is to share the detailed app protocols for using the app to evaluate ocular alignment under different viewing conditions, namely, near and far fixation distance; with and without eye covering to break binocular fusion.
Protocol
This study was conducted in accordance with the tenets of the Declaration of Helsinki, at Schepens Eye Research Institute (Boston, MA) and Spaulding Rehabilitation Hospital (Boston, MA). Informed consent was obtained from all the participants. The study was approved by the local institutional review boards of Mass Eye and Ear (Boston, MA).
NOTE: Patient inclusion criteria were prior diagnosis of horizontal strabismus (constant or intermittent exotropia or esotropia) and no other visual impairments. This study was a part of a larger one reported previously12. Data for 14 patients recruited in the US in the larger study12 are reported here with permission. An optometrist specialized in vision rehabilitation who routinely evaluate strabismus in clinic performed prism and alternate cover test, following by measurement with the app to prevent bias of the cover test results by the objective app measurement.
1. Prepare the test
NOTE: Testing can be performed in any environment; however, the following controls are likely to aid in successful testing.
- Conduct the test in a well-lit environment. Let the patients face in a direction such that corneal reflections from windows and ceiling lights are not located in the center of the eyes. Try to avoid strong background light, such as windows.
NOTE: Usually it helps to have a ceiling light right above the head, or a window on one side of the patient. Sometimes, asking the patient to hold their hand above their brow or using a visor can help shield the eyes from strong light sources which create additional reflections on the cornea, as needed. Turning off point light sources such as canister lights or gooseneck lamps will decrease the intensity of extra corneal reflections, making it easier for the software to detect the reflection from the camera flash as intended. If point light source is needed it may be diffused by pointing it at the wall or using a diffuser (i.e., lamp shade).
2. Measure tropia (manifest strabismus) with single snapshot−near fixation
- Launch the app and set the mode to No Cover (button at upper right corner).
- Select near fixation (button at lower right corner).
- Hold the phone in landscape orientation about 40 cm from the patient at eye level with the rear-camera facing the patient to be measured.
NOTE: The distance does not have to be accurately controlled. The app can automatically compensate for different distances. - Instruct the patient to fixate on the flash light, which is off at this point. For tests requiring precise accommodation such as when screening for accommodative esotropia, paste a fixation target (such as a letter) on the back of the phone, directly below or above the flashlight.
- While the patient confirms he/she is fixating, press the round button to take a snapshot, which will be analyzed by the app.
- When the analysis is completed, the app will show detected eye features: limbus (iris outer) boundary indicated by a large circle (green), the center of the eye indicated by a cross (green), and the location of the corneal reflection indicated by a small circle (red). Verify these features are detected without obvious errors (such as incorrect limbus fitting, or incorrect location or missing corneal reflection).
- On the same screen, under the captured picture, the app will show the measurements related to the eye alignment. If satisfied with the results, press the save button to save the current test in the phone. Otherwise, press the back-arrow button to retest.
3. Measure tropia (manifest strabismus) with snapshot−far fixation
NOTE: To measure tropia for far fixation, the angle kappa for each eye needs to be measured at least once. The app will automatically choose the latest measurement of angle kappa in the history. If it is not available for either eye, the app will give a reminder to first obtain this measurement (see section 6 for details of angle kappa measurement).
- Launch the app and set the mode to No Cover (button at upper right corner).
- Select far fixation mode (button at lower right corner).
- Hold the phone in landscape orientation about 40 cm from the patient at eye level with the rear face of the phone facing the patient.
NOTE: The distance does not have to be accurately controlled. The app can automatically compensate for different distances. - Place the phone slightly below two eyes so that the patient can look above the phone and fixate a target in the distance (typically 5 m away). Make sure the camera is in approximately between the two eyes, not too far to the side of either eye.
- While making sure the patient is fixating properly, press the round button to take a snapshot.
- When the analysis is completed, the app will show detected eye features: limbus boundary indicated by a large circle (green), the center of the eye indicated by a cross (green), and the location of the corneal reflection indicated by a small circle (red). Verify these features are detected without obvious errors (such as incorrect limbus fitting, or incorrect location or missing corneal reflection).
- Under the picture there are measurement outcomes for eye alignment including prism diopters. If satisfied with the results, press the save button to save the test in the phone. Otherwise, press the back-arrow button to retest.
4. Measure intermittent strabismus or phoria with cover test−near fixation
- Launch the app and toggle on the cover test mode (button at upper right corner), and select near fixation (button at lower right corner).
- Hold the phone in landscape orientation about 40 cm from the patient.
NOTE: The distance does not have to be accurately controlled. The app can automatically compensate for different distances. - Instruct the patient to fixate the flash light, which is turned off at this point. For tests requiring precise accommodation, paste a fixation target on the back of the phone, directly below or above the flashlight.
- Use an occluder to cover one of the eyes.
- Press the round button. The app will start to monitor the status of the two eyes (whether one eye is covered).
- While making sure the patient is fixating properly, remove the occluder quickly (i.e., cover-uncover test), or first move the occluder between the two eyes to perform alternate covering a few times and then take the occluder away quickly. The app will automatically take a picture as soon as the occlude is taken away from eyes.
- When the analysis is completed, the app will show detected eye features: iris indicated by a large green circle, the center of the eye indicated by a green cross, and corneal reflection from flash indicated by a small red circle. Verify these features are detected without obvious errors.
- Under the picture there are measurement outcomes for eye alignment in prism diopters. If satisfied with the results, press the save button to save the test in the phone. Otherwise, press the back-arrow button to retest.
5. Measure intermittent strabismus or phoria with cover test−far fixation
NOTE: To measure intermittent ocular misalignment for far fixation, the angle kappa for each eye needs to be measured at least once. The app will automatically choose the latest angle kappa measure. If it is not available for either eye, the app will give a reminder to first obtain this measurement (see section 6 for details of angle kappa measurement).
- Launch the app and set the mode to cover test (button at upper right corner).
- Select far fixation (button at lower right corner).
- Hold the phone in landscape orientation about 40 cm from the patient at eye level.
NOTE: The distance does not have to be accurately controlled. The app can automatically compensate for different distances. It is best if the flash light/camera is between the eyes. Since the camera and flash are off to one corner in most phone models, this means the phone display itself will be slightly off-center. - Instruct the patient to look just above the phone and to fixate the target in distance (typically 6 m away).
- Use an occluder to cover an eye.
- Press the round button. The app will start to detect the uncovering of the eye.
- While making sure the patient is fixating properly, remove the occluder quickly (i.e., cover-uncover test), or first move the occluder between the two eyes to perform alternate covering a few times and then take the occluder away quickly. The app will automatically take a picture as soon as the occluder is taken away from eyes.
- When the analysis is completed, the app will show detected eye features: limbus boundary indicated by a large circle (green), the center of the eye indicated by a cross (green), and the location of the corneal reflection indicated by a small circle (red). Verify these features are detected without obvious errors (such as incorrect limbus fitting, or incorrect location or missing corneal reflection).
- Under the picture there are measurement outcomes for eye alignment in prism diopters. If satisfied with the results, press the save button to save the test in the phone. Otherwise, press the back-arrow button to retest.
6. Measure angle kappa
- Launch the app.
- Select Measure angle kappa.
- Hold the phone in landscape orientation about 40 cm from the patient at eye level.
NOTE: The distance does not have to be accurately controlled. The app can automatically compensate for different distances. - Instruct the patient to use the eye to be tested (either eye) to fixate on the flash light, which is off at this point. Have the other covered by hand or an occluder.
- While making sure the patient is fixating properly, tap the round button to take a snapshot, which will be analyzed by the app.
- When the analysis is completed, the app will show the detected eye features: limbus boundary indicated by a large circle (green), the center of the eye indicated by a cross (green), and the location of the corneal reflection indicated by a small circle (red). Verify these features are detected without obvious errors (such as incorrect limbus fitting, or incorrect location or missing corneal reflection). Under the picture there are measurement outcomes for angle kappa (in degrees).
Representative Results
In this work, we describe the protocols to evaluate ocular alignment using a smartphone app that performs the photographic Hirschberg test. The interface of the app is shown in Figure 1. The users can choose to perform cover test or measure a patient with both eyes fixating at a target simultaneously, either at near or far fixation distances. Once the viewing conditions are determined depending on the test purposes, the users can follow the protocols and take a photo of the patient. After image processing, the app will show the analysis results to the users. As an example shown in Figure 2, the limbus boundaries (green circles) of the two eyes as well as the corneal reflection of the flash light (red dots) were detected correctly. This suggests that the ocular alignment measure (18.5Δ) shown below the image is not subject to image analysis error. In this particular case, the patient had left exotropia, which is obvious from the image as the corneal reflection offset was much larger in the left eye. However, the app does not report which eye is deviated, because in cases of small strabismus angle and unknown angle kappa, it would be unreliable for the app to determine the deviated eye. For comparison, an example without strabismus is shown in Figure 3. Figure 4 shows an example of erroneous limbus detection. While the detection of corneal reflection (small red circle) is correct, the green circle apparently does not match the limbus boundary. The test should be redone.
According to cover test on those patients, the range of strabismus angle was between 25Δ esotropia to 50Δ exotropia, with the smallest magnitude of strabismus angle being 6Δ. There were 10 patients with exotropia and 4 patients with esotropia. As the linear regression analysis showed (slope = 1.02, R2 = 0.94, p < 0.001), the app measurements of strabismus angles were consistent with clinical cover test measurements (Figure 5).
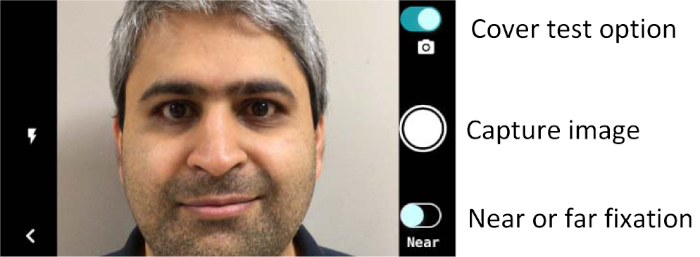
Figure 1: User interface of the strabismus testing app. Users can toggle on cover test and fixation distance. Under different conditions, the instructions given to the patient may be different, as described in the protocol. Please click here to view a larger version of this figure.
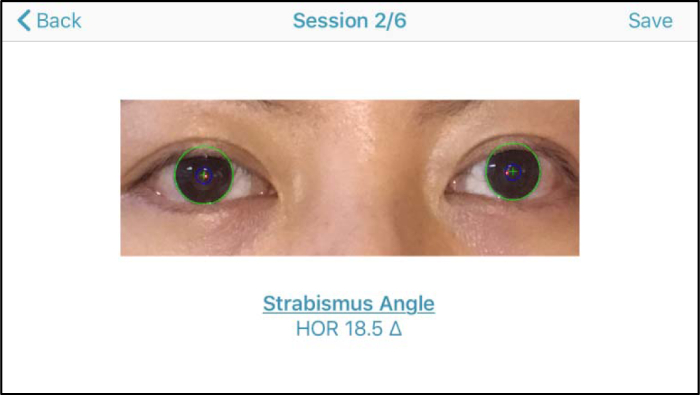
Figure 2: A case of left exptropia. This is the results shown to the users, who should verify the detection of limbus boundary and corneal reflection before reading the strabismus angle. If those image features are not detected correctly, the users should redo the test. Please click here to view a larger version of this figure.
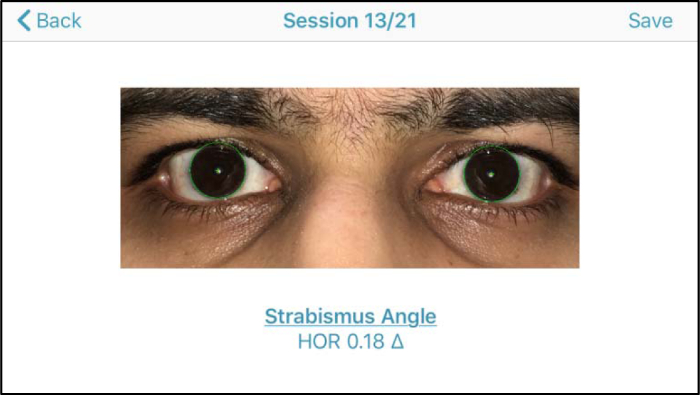
Figure 3: An example under near fixation without cover test. The corneal reflection and eye center were aligned well in both eyes. Therefore the horizontal (HOR) ocular misalignment was almost zero, as the app reported. Please click here to view a larger version of this figure.
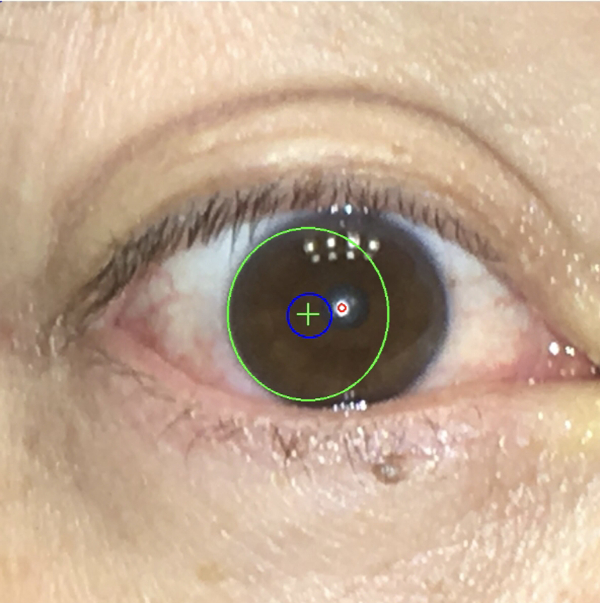
Figure 4: An example of erroneous limbus detection. Please click here to view a larger version of this figure.
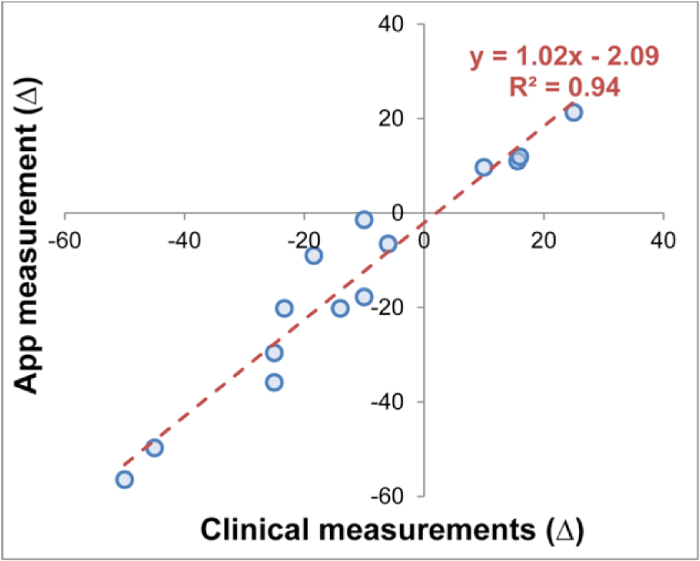
Figure 5: Comparison of strabismus angle measurement using the app with clinical measurements done with covert testing (n = 14). Negative values indicate exotropic deviations, positive values indicate esotropic deviations. Overall, measurements with the app were consistent with the clinical measurements of strabismus. This figure has been modified from our previous publication12. Please click here to view a larger version of this figure.
Discussion
A person without professional training can use the EyeTurn app to capture pictures of the eyes and obtain ocular alignment measurements, which might be interpreted by an eye care specialist onsite or remotely. The app only provides magnitude of the misalignment, rather than any interpretation or diagnosis. Eye care professionals such as optometrists or ophthalmologists should determine if the misalignment is significant or not, and make a diagnosis after considering other factors including the conditions under which the measurement was taken.
Taking good quality pictures is essential for the measurement. The camera should be placed at a position between two eyes. Being too far away from the midline can cause a difference in the image size between two eyes, and consequently result in measurement inaccuracy.
The limbus boundary is one of the key features that the app uses for locating eye position. Verifying the limbus boundary fitting (the green circle in results) is a crucial step. If the fitting appears to be inaccurate, the measurement will be subject to errors and the eye care professional will not be able to correctly interpret the test. Usually for patients with larger eye fissures, i.e., iris area being more revealed, the fitting will be robust and accurate. On the other hand, for patients with smaller eye fissures, which have only a small portion of the left and right boundaries revealed, the fitting may be prone to inaccuracies. In this situation, operators can ask the patients to open their eyes widely, or gently lift the eyelid wide open. The current version does not provide measurement of vertical misalignment, which will be implemented in future versions.
In addition to the promise for use in strabismus clinics, another potential application of the app is in vision screening. For prevention of amblyopia, the American Academy of Pediatrics strongly endorsed the development of cost-effective image-based screening as a means to extend screening to all children14. Red reflex method, which compares the brightness of the "red eye" flash artifact with the strabismus eye being a lighter or brighter red color, can detect both refractive error and strabismus, but cannot quantify the magnitude of the strabismus. Devices implementing the red flex method include Photoscreener and Vision Screener15,16. These photoscreeners have not been widely adopted by school districts, likely due to cost. Compared to standalone systems, modern smartphone cameras provide better value, improved accessibility, and rapidly improved and higher resolution cameras. Recently, there is an app that implements the red reflex method, GCK app17. The GCK app has some limitations in that it does not give a quantitative measurement of strabismus and requires more control of ambient lighting than the Hirschberg methods. The app presented in this article can be potentially an alternative or complementary solution for vision screening, because of its ease of use and equivalent accuracy with standard clinical measurement using prisms.
Divulgazioni
The authors have nothing to disclose.
Acknowledgements
This work was supported in part by NIH grant R44EY025902 and by the Mass Eye & Ear Curing Kids Grant.
Riferimenti
- Kemper, A. R., Clark, S. J. Preschool vision screening in pediatric practices. Clinical Pediatrics. 45 (3), 263-266 (2006).
- Rowe, F. The profile of strabismus in stroke survivors. Eye. 24 (4), 682-685 (2010).
- Black, K., McCarus, C., Collins, M. L. Z., Jensen, A. Ocular Manifestations of Autism in Ophthalmology. Strabismus. 21 (2), 98-102 (2013).
- Taylor, K., Elliott, S. Interventions for strabismic amblyopia. Cochrane Database of Systematic Reviews. 10 (8), (2011).
- Cotter, S. A., et al. Fixation preference and visual acuity testing in a population-based cohort of preschool children with amblyopia risk factors. Ophthalmology. 116 (1), 145-153 (2009).
- Robaei, D., et al. Factors Associated with Childhood Strabismus: Findings from a Population-Based Study. Ophthalmology. 113 (7), 1146-1153 (2006).
- Tarczy-Hornoch, K., et al. Risk factors for decreased visual acuity in preschool children: the multi-ethnic pediatric eye disease and Baltimore pediatric eye disease studies. Ophthalmology. 118 (11), 2262-2273 (2011).
- Chan, K. W., Deng, L., Weissberg, E. M. Detection of Strabismus by Non-Health Care Professionals in an Ethnically Diverse Set of Images. JAMA Ophthalmology. 134 (1), 30-36 (2016).
- Hunter, D. G., Guyton, D. L. Vertical location of the corneal light reflex in strabismus photography. Archives of Ophthalmology. 116 (6), 767-771 (1998).
- Eskridge, J. B., Wick, B., Perrigin, D. The Hirschberg test: a double-masked clinical evaluation. American Journal of Optometry and Physiological Optics. 65 (9), 745-750 (1988).
- Hasebe, S., Ohtsuki, H., Tadokoro, Y., Okano, M., Furuse, T. The reliability of a video-enhanced Hirschberg test under clinical conditions. Investigative Ophthalmology & Visual Science. 36 (13), 2678-2685 (1995).
- Pundlik, S., Tomasi, M., Liu, R., Houston, K., Luo, G. Development and Preliminary Evaluation of a Smartphone App for Measuring Eye Alignment. Translational Vision Science & Technology. 8 (1), 19 (2019).
- Cheng, W., et al. The EyeTurn App for School Vision Screening. American Academy of Optometry Annual Meeting. , (2018).
- Committee on Practice and Ambulatory Medicine and Section on Ophthalmology. Use of Photoscreening for Children’s Vision Screening. Pediatrics. 109 (3), 524-525 (2002).
- Simons, B. D., Siatkowski, R. M., Schiffman, J. C., Berry, B. E., Flynn, J. T. Pediatric photoscreening for strabismus and refractive errors in a high-risk population. Ophthalmology. 106 (6), 1073-1080 (1999).
- Kerr, N. C., Somes, G., Enzenauer, R. W. The effect of developmentally-at-risk status on the reliability of the iScreen(R) photorefractive device in young children. The American Journal of Orthopedics. 61, 117-123 (2011).
- Arnold, R. W., O’Neil, J. W., Cooper, K. L., Silbert, D. I., Donahue, S. P. Evaluation of a smartphone photoscreening app to detect refractive amblyopia risk factors in children aged 1-6 years. Clinical Ophthalmology. 12, 1533-1537 (2018).

