Low-Cost Single-Port (LoCoSP) Device for a Transcervical Approach in Minimally Invasive Transhiatal Esophagectomy
Summary
Here, we describe a step-by-step description of transhiatal esophagectomy and the development of a low-cost single-port device for a transcervical approach in a minimally invasive transhiatal esophagectomy.
Abstract
Esophagectomy remains the preferred option to achieve curative treatment in advanced esophageal cancer, but the choice of surgical approach remains controversial. A transthoracic approach may improve lymph node dissection, but it has considerable morbidity and respiratory complications. Transhiatal access has been demonstrated as an efficient means of minimizing post-operative complications. Minimally invasive transhiatal esophagectomy may reduce operative trauma and morbidity as well as enhance postoperative recovery with no compromise in cancer recurrence or survival. Nevertheless, it has a technical limitation in terms of cervical esophagus dissection. Thus, a low-cost single-port device was developed to complete upper mediastinal dissection by a transcervical approach during minimally invasive transhiatal esophagectomy. This device uses a nasogastric tube, a number-eight sterile glove, a sterile sponge, and 3 permanent 5-mm trocars. The step-by-step process of transhiatal esophagectomy and the development of this device are described. This technique allows for the dissection of the upper mediastinum, as well as the esophagus over the aortic arch and behind the superior portion of the trachea. The harvesting of lymph nodes along the left recurrent laryngeal nerve and paratracheals was improved.
Introduction
There are multiple options for the treatment of esophageal cancer, which involve endoscopy, surgery1, neoadjuvant, and definitive treatment with chemoradiotherapy2. Esophagectomy is the most important element in the curative treatment of patients with advanced esophageal cancer3, and the two main approaches currently used for surgical treatment are transthoracic esophagectomy (TTE) and transhiatal esophagectomy (THE). However, the choice of approach remains controversial. Since TTE requires pulmonary collapse during surgery, more frequent pulmonary complications are to be expected than in a transhiatal approach. Minimally invasive techniques are used to reduce access trauma to the lungs and others structures of the thorax, but they do not decrease the morbidity in comparison to THE. Thus, minimally invasive THE has become a more attractive option; however, the upper esophagus and upper mediastinum are difficult areas to dissect due to blind areas, and cervical incision might be not enough to allow a safe dissection of the upper part.
Laparoscopic THE reduces morbidity4 and enhances postoperative recovery with no compromise in cancer recurrence or survival5. THE has been shown to decrease the hospital stay, hospital mortality, surgical time, and blood loss. Furthermore, TTE has a higher risk of pulmonary complications. The patient’s stay in the intensive care unit is significantly longer after transthoracic resection, and hospital stay is also significantly prolonged.
However, there is an issue with THE regarding the lymph node dissection, particularly in the upper mediastinum, which is a blind area. This results in a risk of tracheal and vascular lesions during the surgery. Tokairin6 et al. and Fujiwara et al. described a single-port mediastinoscopic method for upper mediastinal dissection in esophageal cancer surgery. This technique enabled clear visualization of the structures around the aortic arch and safe lymphadenectomy7. A low-cost single-port device was developed to improve upper mediastinal dissection using a left transcervical mediastinoscopic approach, which was used to improve the visibility and dissection in the upper mediastinum around the aortic arch. The aim of this project is to describe the step-by-step process of a laparoscopic THE completed using a mediastinoscopy cervical approach with a low-cost single-port device in a rendezvous technique.
Protocol
The surgical procedure and the protocol were explained to the patients, and they signed a consent form. This study was approved by the local ethics committees of the institutional review board and informed consent were collected from patients, register number 1688/20. Patients who underwent transhiatal esophagectomy were included in the protocol, while those patients who underwent a transthoracic approach were excluded.
1. Production of low-cost single-port device
- Use a nasogastric tube, a sterile number-eight glove, a sterile sponge, 3 permanent 5-mm trocars and surgical suture materials.
- Make one cylinder with the sterile sponge.
- Use three glove fingers to triangulation the trocars: little finger, middle finger and thumb
- Use the three trocars to pierce the sponge and perform a triangulation (Figure 1 and Figure 2).
- Make one ring with the nasogastric tube.
- Place the sponge, the trocars and the glove between the ring to seal the air leak during mediastinoscopy and to stabilize the structures.
- Use the glove to cover all the structures to prevent air leak again.
2. Laparoscopic and transhiatal procedure
- Put the patient under general anesthesia in a supine position.
- Insert an orotracheal, a central venous and an invasive arterial pressure catheter respectively in the trachea, jugular vein and radial artery.
- Create a pneumoperitoneum using a Veress needle. Insert the needle in the midline above the umbilical scar.
- Place laparoscopic trocars in the following positions: one 12-mm trocar in the supraumbilical area, two 10-mm trocars in the left and right hypochondrium, and two 5-mm trocars in the right hypochondrium and the epigastrium.
- Perform abdominal cavity inventory to search for peritoneal or liver metastasis.
- Examine the gastroepiploic arcade from the right gastroepiploic artery to the short gastric vessels.
- Open up the gastrocolic ligament to the pilorus to gastric fundus while preserving the gastroepiploic arcade.
- Perform the posterior gastric wall release. Lift up the posterior aspect of the stomach and dissect using an ultrasonic harmonic scalpel to free it from the retroperitoneum. Identify the pancreas, left gastric vessels, and celiac trunk.
- Make a gastric tube with a stapler. Start stapling in the antrum by the lesser curvature and move towards the greater curvature. Make a slim gastric tube to create an anastomosis in the cervical esophagus and empty it properly.
- Perform dissection and ligation of the left gastric vessels at the origin to harvest the appropriate lymph nodes. Perform the dissection cranially to the origin of the left gastric vein and the left gastric artery.
- Use one clip proximally and other distally in the left gastric vein before sealing it. Use two hemolocks proximally and one distally in the left gastric artery before sealing it.
- Sequentially dissect all the lymph nodes and connective tissue along the left gastric artery (7), common hepatic artery (8a), celiac trunk (9), proximal splenic artery (11p), lesser curvature (3), and the esophago gastric junction (1) and reflect toward the stomach.
- Perform dissection of the esophageal hiatus. Enlarge the hiatus anteriorly to facilitate dissection and mobilization of the thoracic esophagus and the other mediastinal structures.
- Identify the aorta and dissect the posterior wall of the esophagus from the descending aorta with a harmonic scalpel.
- Continue the dissection of the esophagus in a paraesophageal plane in the lower mediastinum under pneumomediastinum. In the middle to upper portion of the mediastinum, however, this dissection is normally performed blindly and may lead to tracheal lesions or hemorrhage from tearing of the larger vessels.
- Stop the dissection in the transition of the middle to upper mediastinum up to the carina and started with a single-port mediastinoscopic cervical approach using a rendezvous technique (this technique is described below).
3. Transcervical procedure
- Make an oblique incision along the anterior border of the left lower sternocleidomastoid parallel to the clavicle.
- Identify the sternocleidomastoid muscle and divide.
- Mobilize the cervical esophagus and initiate the dissection of the cervical lymph nodes along the left recurrent laryngeal nerve.
- Insert the single-port device into the cervical wound (Figure 3) and create a pneumomediastinum by carbon dioxide insufflation (8 mmHg). Use a 5-mm Otic and a Harmonic Scalpel for esophagus dissection along with a laparoscopic grasper.
- Dissect the esophagus over the aortic arch and behind the superior portion of the trachea. Perform the dissection of the lymph nodes along the left recurrent laryngeal nerve and trachea.
- After this stage, completely mobilize the esophagus, and reach the region that was dissected using a transhiatal approach. Divide the cervical esophagus, and remove the esophagus with the tumor by an abdominal incision.
- Perform cervical anastomosis with gastric tube and esophageal stump.
Representative Results
The LoCoSP device is a useful tool for safely dissecting the structures of the upper mediastinum. Direct visualization of the cervical and upper thoracic esophagus allows for safe dissection with less risk of tracheal injury and hemorrhage from tearing of the larger vessels, in addition to improving the lymphadenectomy of the left recurrent laryngeal and paratracheal nodes.
From 2018 to 2020, 12 patients with distal esophageal carcinoma (2 squamous cell carcinoma and 10 adenocarcinoma) were submitted to laparoscopic transhiatal esophagectomy with transcervical access to cervical esophagus dissection and lymphadenectomy. The median age was 62 (60 ± 85) years old, only one patient was female. There was no chordal palsy, bleeding, tracheal damage related to the transcervical access. One anastomotic fistula occurred with no clinical complications, spontaneous drainage through the cervical incision. The median operation time was 360 min (300 ± 420 min), and the operation time of the transcervical dissection of the cervical esophagus was 60 min (40 ± 110 min). The median hospital stay was 10 days (9 ± 12 days). All cases were performed with the LoCoSP device (Table 1).

Figure 1: Low-cost single-port device Please click here to view a larger version of this figure.
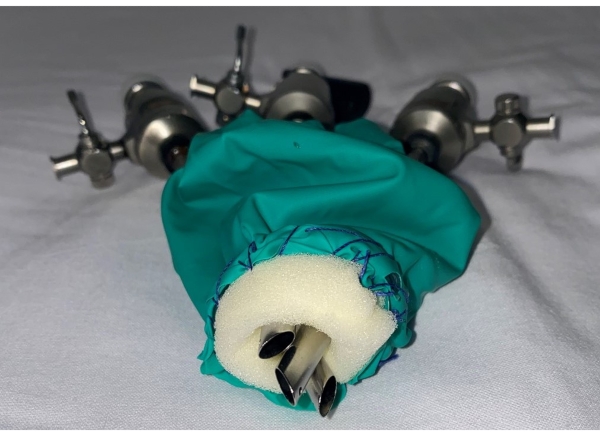
Figure 2: Low-cost single-port device (note the triangulation of the three trocars) Please click here to view a larger version of this figure.
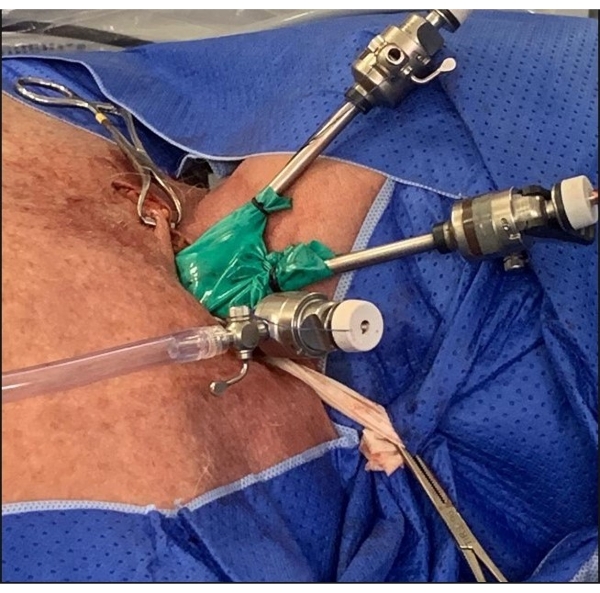
Figure 3: Low-cost single-port device into the cervical wound Please click here to view a larger version of this figure.
| Total Patients | 12 |
| Median Age (years) | 62 |
| Number Anastomotic fistula | 1 |
| Median operation time (minutes) | 360 |
| Median operation time transcervical dissection (minutes) | 60 |
| Median Hospital stay (days) | 10 |
Table 1: Surgery results using low cost single-port device
Discussion
The LoCoSP device allows for safer surgery using a transcervical approach in minimally invasive THE. This is accomplished by improving the recognition and dissection of the esophagus, trachea, and the aortic arch under magnified vision. The advantages of THE are amplified. In addition to allowing surgery with less morbidity and fewer pulmonary complications, this technique can improve the dissection of left paratracheal and recurrent lymph nodes. Another advantage of this technique is that it is possible to reduce the risk of tracheal and vascular injury during THE.
Damage of the posterior wall of the trachea or the main bronchi rarely occurs during esophagectomy, and the reported rates are 1.35%8 to 1.8%9. However, when it does happen, the prognosis is unfavorable10. Dissection with a single-port mediastinoscopic cervical approach allows for direct visualization of the upper esophagus and the trachea, which could possibly decrease the chances of injury to the airways. Finally, the production of the LoCoSP device is easy, and it can be reproduced in other centers. The device is produced using cheap and widely available instruments in any operating room. An important limitation of the technique is the leakage of air through the cervical wound, during the dissection of the upper mediastinum. Nevertheless, the method is still an experimental method, and the real benefit of using the LocOSP device must be studied and analyzed in a greater number of patients.
Disclosures
The authors have nothing to disclose.
Acknowledgements
None.
References
- Borggreve, A. S., et al. Surgical treatment of esophageal cancer in the era of multimodality management. Annals of the New York Academy of Sciences. 1434 (1), 192-209 (2018).
- Kato, H., Nakajima, M. Treatments for esophageal cancer: a review. General Thoracic and Cardiovascular Surgery. 61 (6), 330-335 (2013).
- Rice, T. W., Patil, D. T., Blackstone, E. H. 8th edition AJCC/UICC staging of cancers of the esophagus and esophagogastric junction application to clinical practice. Annalsof Cardiothoracic Surgery. 6 (2), 119-130 (2017).
- Hulscher, J. B., Tijssen, J. G., Obertop, H., van Lanschot, J. J. Transthoracic versus transhiatal resection for carcinoma of the esophagus: a meta-analysis. Annals of Thoracic Surgery. 72 (1), 306-313 (2001).
- Rentz, J., et al. Transthoracic versus transhiatal esophagectomy: a prospective study of 945 patients. Journal of Thoracic and Cardiovascular Surgery. 125 (5), 1114-1120 (2003).
- Tokairin, Y., et al. Mediastinoscopic subaortic and tracheobronchial lymph node dissection with a new cervico-hiatal crossover approach in thiel-embalmed cadavers. International Surgery. 100, 580-588 (2015).
- Fujiwara, H., et al. Single-port mediastinoscopic lymphadenectomy along the left recurrent laryngeal nerve. Annals of Thoracic Surgery. 100 (3), 1115-1117 (2015).
- Gupta, V., et al. Major airway injury during esophagectomy: experience at a tertiary care center. Journal of Gastrointestinal Surgery. 13 (3), 438-441 (2009).
- Hulscher, J. B., et al. Injury to the major airways during subtotal esophagectomy: incidence, management, and sequelae. Journal of Thoracic and Cardiovascular Surgery. 120 (6), 1093-1096 (2000).
- Fermin, L., Arnold, S., Nunez, L., Yakoub, D. Extracorporeal membrane oxygenation for repair of tracheal injury during transhiatal esophagectomy. Annals of Cardiac Anaesthesia. 20, 67-69 (2017).

