An Ex Vivo Model of Ovarian Cancer Peritoneal Metastasis Using Human Omentum
Summary
This protocol describes the establishment of a three-dimensional (3D) ex vivo model of cancer cell-omentum interaction. The model provides a platform for elucidating pro-tumor mechanisms within the adipose niche and for testing novel therapies.
Abstract
Ovarian cancer is the deadliest gynecologic malignancy. The omentum plays a key role in providing a supportive microenvironment to metastatic ovarian cancer cells as well as immune modulatory signals that allow tumor tolerance. However, we have limited models that closely mimic the interaction between ovarian cancer cells and adipose-rich tissues. To further understand the cellular and molecular mechanisms by which the omentum provides a pro-tumoral microenvironment, we developed a unique 3D ex vivo model of cancer cell-omentum interaction. Using human omentum, we are able to grow ovarian cancer cells within this adipose-rich microenvironment and monitor the factors responsible for tumor growth and immune regulation. In addition to providing a platform for the study of this adipose-rich tumor microenvironment, the model provides an excellent platform for the development and evaluation of novel therapeutic approaches to target metastatic cancer cells in this niche. The proposed model is easy to generate, inexpensive, and applicable to translational investigations.
Introduction
Ovarian cancer is the deadliest gynecologic malignancy worldwide1. The lifetime risk of developing this cancer is approximately 1 in 70, with the median age of diagnosis at 63 years old2. Primary ovarian malignancies are classified histologically as either epithelial or non-epithelial. Epithelial ovarian cancers (EOC) represent over 90% of tumors, and the most common subtype is high-grade serous carcinoma (HGSC), which accounts for approximately 70%-80% of EOCs. Currently, there are no effective screening methods to detect disease early. So most patients are diagnosed at an advanced stage (i.e., Fédération Internationale de Gynécologie et d'Obstétrique [FIGO] stage III or IV) after the cancer has spread throughout the peritoneal cavity2.
Standard frontline treatment is cytoreductive surgery to remove all visible macroscopic disease, followed by adjuvant platinum-based chemotherapy to destroy any residual microscopic disease. While there have been many advances in ovarian cancer treatment over the last two decades, approximately 70% of patients with advanced disease will relapse within 3 years of treatment3. Given the overall poor prognosis of these patients, ongoing and future translational research efforts in EOC aim to identify biomarkers for early detection, prevent metastasis, improve current therapies to evade resistance and develop new personalized cancer treatments.
Generalized metastasis within the peritoneal cavity and its associated chemoresistance are two of the major limitations for the improvement of the treatment of patients with ovarian cancer4,5. The omentum, a fatty apron-like structure that hangs down from the stomach over the intestines, is a main site of ovarian cancer metastasis6,7. In addition to its function as a physical barrier, the omentum has been shown to have regenerative and angiogenic capacities and possess immune activities, which together promote vascularization, accelerate wound healing, and limit infection8. It contains a high concentration of stem cells that can differentiate into various cell types and can help repair damaged tissues. The omentum can become inflamed in response to injury or infection, which triggers the migration of immune cells to the site of injury9. These immune cells release growth factors and other molecules that help to promote the repair and regeneration of damaged tissue. Immune cells, such as macrophages, lymphocytes, and plasma cells, localized in the omentum are structures known as "milky spots", which are responsible for detecting and attacking pathogens and regulating peritoneal immunity. The omentum has also been shown to play a role in inducing immune tolerance10, which is the ability of the immune system to tolerate self-antigens and not attack healthy tissues. However, the same immune-related activities are also involved in pathological responses, such as the growth of omental tumors, metastasis, and escape of immune surveillance9,11. Previous studies from our lab and others have demonstrated a unique and active role of the adipose microenvironment in the inhibition of anti-tumoral immune responses and in the acquisition of chemoresistance12,13,14. Unfortunately, we have limited information on the cellular and molecular mechanisms by which the omentum provides a pro-tumoral microenvironment.
To better understand the interactions between cancer cells and the omentum, a 3D culture system consisting of human ovarian cancer cells and patient-derived omentum explants was developed. The protocol described here represents a novel ex vivo model of peritoneal carcinomatosis. This model mimics the natural progression of ovarian cancer tumorigenesis in this adipose-rich tissue. The proposed model is easy to generate, inexpensive, and potentially applicable to translational investigations in ovarian cancer research.
Protocol
The following research protocol was reviewed and approved by the Wayne State University Institutional Review Board (IRB). Informed consent was obtained from all patients prior to surgery. Figure 1 illustrates the three general steps in this protocol.
1. Preparation of human omentum tissue
- Prepare omentum culture media (DMEM/F12 + 10% fetal bovine serum + 1% penicillin-streptomycin) and store at 4 °C. Aliquot 30-40 mL of this media into a sterile 50 mL conical tube or surgical specimen container.
- Obtain surgical specimens from omental biopsy or omentectomy surgery. Immerse the sterile specimen in omentum culture media immediately after removal in the operating room. If the workflow does not allow this, place the specimen in omentum culture media as soon as possible. Transfer the sample by placing it on ice and store at 4 °C until processing.
NOTE: The size of the omentum specimen removed will determine the amount of workable tissue. - Process the omentum specimen within 1-2 h of collection using a laminar flow hood. Ensure that all materials and tools are sterile or sterilized.
- Remove the omentum from the collection container and transfer it into a 100 mm culture dish. Immerse the specimen in 1x phosphate-buffered saline (1x PBS) and gently wash the specimen to remove any blood clots or debris.
- Cut the tissue into pieces (0.5 cm x 0.5 cm or 100-200 mg; Figure 2A) using either small surgical scissors or a 10-15 mm scalpel. Use small surgical forceps to help manipulate the tissue and avoid crushing the omentum. If an energy device was used to surgically remove the omentum specimen, then avoid using the distorted tissue at the sealed edge.
- Place each piece of cut omentum into individual wells of a 24-well culture plate and fill the wells with 500 μL of omentum culture media or to a volume that is enough to cover the omentum without allowing the omentum piece to float above the well floor (Figure 2B).
- Store omentum pieces in fresh culture media at 4 °C until ready for injection.
2. Preparation of ovarian cancer cells
- Culture human ovarian cancer cells in a 75 cm2 culture flask at 37 °C and 5% CO2 to at least 75% confluency by the day of omentum collection.
NOTE: This protocol utilizes mCherry-positive OCSC1-F2 human ovarian cancer cells previously described15,16,17,18. It can be modified to any cancer cell line tagged with a fluorescence signal. - Prepare cells inside a laminar flow hood immediately after collection of the omentum specimen. Ensure that all materials and tools are sterile or sterilized.
- Add 10 mL of sterile 1x PBS to the culture flask and wash the cells by gently rocking the flask. Remove the 1x PBS and then add 3 mL of 0.05% Trypsin-EDTA.
- Gently rock the culture flask to coat all cells, and then place the flask in an incubator (37 °C and 5% CO2) for no more than 5 min. Tap the culture flask to completely detach the cells, and then neutralize trypsin by adding 3 mL of omentum culture media.
- Mix the cell suspension by pipetting, and then transfer the suspension into a 15 mL conical tube. Centrifuge the suspension for 5 min at 1,200 x g at 24 °C. Remove the supernatant and resuspend the cell pellet in 6 mL of fresh omentum culture media.
- Count the cells using a hemacytometer. Dilute the cell suspension to at least 100,000 cells per 100-200 μL of suspension. This is the volume of injection into each cut piece of omentum.
- Transfer an appropriate number of cells into a new culture flask to continue cell passage.
3. Injection of ovarian cancer cells
- Use a 1 mL syringe to draw up the cell suspension, then attach a 26-G needle. Do not draw up the cell suspension using the needle, as this can fragment the cells.
- Use small surgical forceps to pick up a piece of cut omentum. Transfer the omentum to a separate working sterile dish to facilitate injection. Gently pierce the omentum with the needle tip and inject a small volume of cell suspension into the tissue (Figure 2C).
- Repeat injection over several areas of omentum to a total volume of at least 100 μL or 100,000 cells. Note that much of the cell suspension may appear to pool around the specimen. If there is concern regarding the quality of the injection, then repeat the injection or inject a larger volume of cell suspension into the specimen.
- Return the injected omentum samples into each well of a 24-well culture plate. Take note that the volume of omentum culture media is to a level that covers the omentum without allowing it to float. Carefully handle the plate and place it inside an incubator (37 °C and 5% CO2).
- OPTIONAL: Use Matrigel (basement membrane matrix) to suspend omentum tissue in a solid matrix to allow easier injection and more concentrated cell suspension delivery.
- Thaw the basement membrane matrix at 4 °C and mix in 1:1 ratio with omentum culture media immediately prior to use. Store the basement membrane matrix mixture on ice or at 4 °C until injection. Fill empty wells with enough basement membrane matrix mixture to immerse a cut piece of omentum.
- Place specimens into the basement membrane matrix mixture and then place the 24 well culture plate in an incubator (37 °C and 5% CO2) for 20 min. Once the mixture has solidified, continue with injection as described above.
- Confirm successful injection using fluorescent imaging. Ensure a streak of fluorescent signal is visualized at the injection sites (Figure 2D). Note that the actual number of cells attached to the omentum after injection is unpredictable.
4. Co-culture of human omentum and ovarian cancer cells
- Change media every 48-72 h by adding 500-2000 μL of fresh omentum culture media. Do not pipet media directly on top of omentum tissue, as this may displace cancer cells. Note that if the media color turns to yellow, then change the media.
NOTE: The frequency of media change will depend on the volume of media used and the trajectory of cancer cell growth. Once the cancer cells have seeded the omentum, whether or not the omentum piece is floating is no longer important. - OPTIONAL: If a basement membrane matrix was used, the matrix would typically be dissolved by the time of the first media change.
- Monitor the growth of ovarian cancer tumors using fluorescent imaging. Frequency of imaging is at the discretion of the investigator. Anticipate evidence of small tumors by about 14 days (Figure 3A-C). Results may vary depending on the quality of the injection.
- Terminate the experiment based on the experiment endpoint.
NOTE: Tumor growth and integrity of omentum tissue have been observed past 50 days.
Representative Results
Successful establishment of ovarian cancer cells into omentum specimens was evident by about day 14 (Figure 3A–C). At least 24 replicates were prepared and injected per collected specimen to allow for further experimentation. Tumor growth was monitored by taking fluorescent images (Figure 3D,E). Images had to be carefully interpreted as a monolayer of cancer cells also grew at the bottom of each well that was not attached to the omentum. We preferred taking images of the omentum when it was suspended in media to avoid overlapping fluorescent signals with the cancer cell monolayer.
The absence of a fluorescent signal by day 14 can be considered as failed injections. It was observed that the cancer cells initially spread out across the surface of the omentum during the first 7 days, but over time, they congregated to form tumors (Figure 3A–D). A surrogate measure for tumor burden between samples was the rate at which omentum culture media changed color from red to yellow (Figure 3F). We utilized fluorescent imaging, histologic review, and gross inspection to confirm tumor growth and omental tissue viability past 50 days of co-culture (Figure 4).
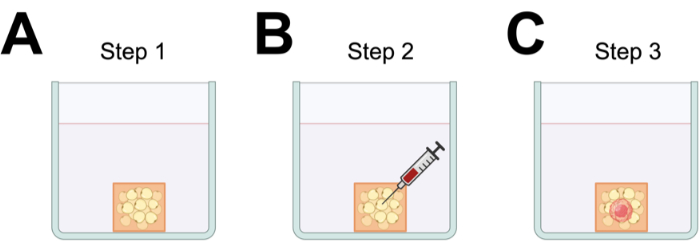
Figure 1: Illustration of general steps in the protocol. (A) Step 1: Preparation of omentum; (B) Step 2: injection of cancer cells; (C) Step 3: establishment of cancer cell-omentum microenvironment. (Figure prepared in BioRender.com). Please click here to view a larger version of this figure.
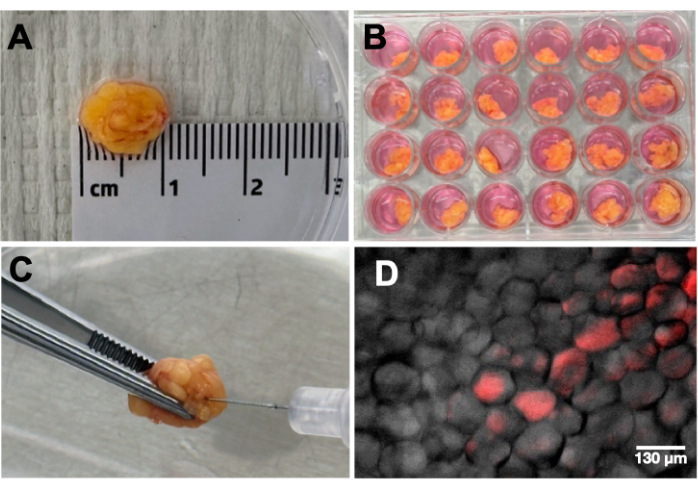
Figure 2: Preparation and injection of cancer cells into the omentum. (A) Omentum is cut into 1×1 cm pieces. (B) Each piece is placed in a well of a 24-well plate and covered with 500 μL of media. (C) Injection of cancer cells into omentum piece. (D) A streak of fluorescent cancer cells is observed after injection. Please click here to view a larger version of this figure.
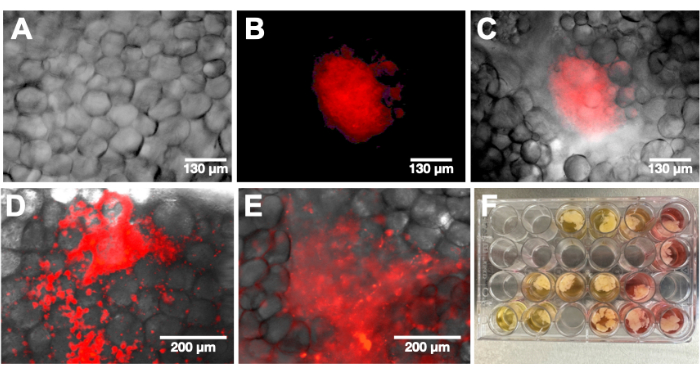
Figure 3: Representative images after 14 and 25 days of co-culture. (A–C) Representative images after 14 days of co-culture: (A) phase, (B) mCherry channel, (C) merged. (D–E) Representative images after 25 days of co-culture. (F) Change in media color from pink to yellow is an indication of successful cancer cell injection and establishment of co-culture. Please click here to view a larger version of this figure.
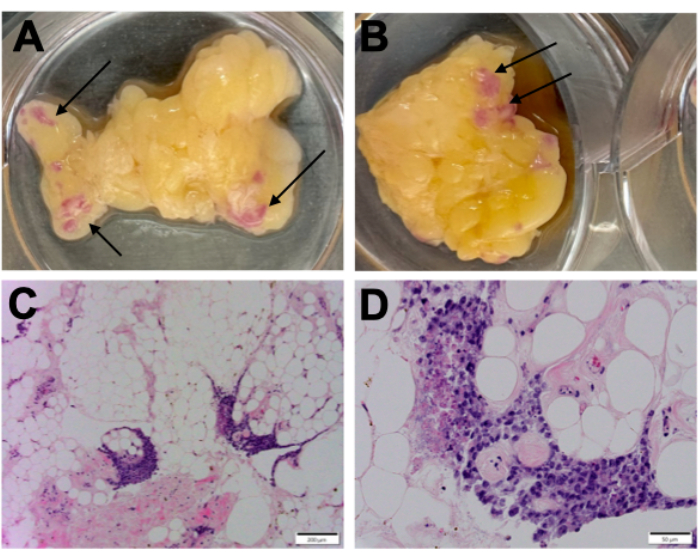
Figure 4: Gross morphology and Hematoxylin and Eosin (H&E) staining. (A,B) Representative gross morphology of co-cultures at day 50; arrows point to sites of growth of mCherry+ ovarian cancer cells. (C,D) Representative H&E staining of co-cultures at day 50. Please click here to view a larger version of this figure.
Discussion
Using this protocol, a preclinical model of peritoneal carcinomatosis for ovarian cancer was developed using a combination of basic in vitro and ex vivo techniques. A progressive tumor growth was observed across 50 days of co-culture after seeding omentum specimens with mCherry+ OCSC1-F2 human ovarian cancer cells. This method was developed and optimized across several experimental trials using different omentum specimens. Successful tumor growth depended on the quality of omentum, viability of cancer cells, and effectiveness of injection. In this report, we only used mCherry+ OCSC1-F2 cells and mCherry+ R182 human ovarian cancer lines previously reported in several publications12,15,16,17,18,19,20,21,22. Using these two cell lines with different doubling times (16 h for OCSC1-F2 and 36 h for R182), a difference in the time to achieve logarithmic growth within the omental tissue was noted. Nevertheless, we were successful in establishing both cell lines in the co-culture system.
Efficient communication between investigators, research coordinators, and surgical teams was critical for the collection and processing of omentum specimens. The investigator identified protocol candidates, the research coordinators obtained consent from patients before surgery, and the investigator collected the specimens from the operating room. Given this workflow, the investigator's schedule had to be flexible as many patient-sided factors affecting collection were unpredictable (e.g., surgery canceled, time of surgery changed, inadequate or no omentum removed). Direct visualization and selection of tissues from the operating room ensured specimen integrity, surgical sterility, and timely processing. Initially, specimen collection was delegated to research coordinators; however, after a few specimens were collected, we noted that time to processing was delayed (i.e., >4 h) and the quality of omentum was grossly inferior (e.g., tissue was in pieces). In one experimental trial, omental tissue was stored at 4 °C for 48 h prior to injection because cancer cells were not ready in time. Similar tumor growth was still observed, but this sequence was not repeated as temperature changes are known to affect the tumor microenvironment (TME).
Before specimen collection, it was important to have sufficiently confluent cancer cells according to the surgery schedule. Since the number of specimens collected each month varied, active cultures of ovarian cancer cells were not always maintained. The frozen cells were thawed at least 1 week in advance, plated using a standard protocol, and then passed the cells at least once to ensure viability. The cell lines used in this protocol were relatively resilient; however, we still encountered instances when cells had not recovered by the day of surgery and could not be injected. In this study, there was no attempt to inject cancer cells that were less than 50% confluent. Subsequent delays related to cell preparation were mitigated by using good sterile technique and splitting cells in ratios to maintain confluence depending on the anticipated specimen collection schedule. We limited the protocol to only two fluorescently tagged cancer cell lines, but it is important to note that other established cancer cell lines or primary cancer cells without fluorescent proteins could also be utilized.
Lastly, the rate of tumor growth was correlated to the confluence of cancer cells adjacent to and within adipocytes immediately following injection. This was determined by taking fluorescent images of all omentum specimens post-injection. Compared to tumor cell inoculation of solid organs or subcutaneous tissues, injecting cancer cells into omental tissue was more challenging. The loose structure and fatty consistency of omentum prevent the tissue from effectively holding volumes of cell suspension without leaking. When a smaller needle (i.e., 30 G or narrower) was used to inject, there was concern for cell fragmentation as cell proliferation was decreased. We tested various injection techniques, cell numbers, and cell suspension volumes and found consistent results with the protocol described above. At the same time, we acknowledge that such variations to the protocol are likely to still produce similar results given the malignant nature of the cells. The addition of Matrigel made the injection step easier as the extracellular matrix held the cell suspension better; however, this method is more expensive and did not consistently produce a higher tumor burden in the samples. Overall, it was rare for any of the omentum specimens to not grow tumors, but the number of tumors and speed of growth varied.
This model simulated a hallmark of ovarian cancer tumorigenesis by replicating early metastasis to adipose-rich peritoneal tissues. This protocol allows variation with no required skill, is easy to replicate, and generates a system with potential translational value. Compared to existing in vitro and ex vivo models in ovarian cancer, the method described here combines several techniques to produce a model that retains tumor architecture and TME over a long lifespan. Additionally, we observed that when an omentum specimen with multiple tumors was transferred into a new well and cultured with cancer-free omentum (i.e., not injected), the naïve omentum was seeded with cancer cells within 7 days. This finding suggests that the replicated tumors retain metastatic potential via epithelial-mesenchymal transition. We did not identify any similar ovarian cancer models in the literature that cultured tissue biopsies for extended periods of time. This approach is supported by a previous finding that mesothelial cells isolated from mouse omentum could be cultured for more than 30 passages after collection23.
The model described in this study can be employed to further understand the effect of direct interaction between ovarian cancer cells and the cells within the adipose-rich omentum. Cancer cells can be dissociated from the omentum tissues and obtained for transcriptomic or immunohistochemistry (IHC) analysis. Additionally, cells can be used for drug response studies.
The primary limitations of this model are that the number of tumors, rate of tumor growth, and location of tumors were unpredictable. Lack of standardization and variation across samples could limit the application of this model. We also made several observations that will require further examination during the development of this protocol. For example, the "control" replicates in one experiment were not actually cancer-free as the patient was subsequently diagnosed with omental micrometastasis; however, the non-injected tumors remained viable throughout the experimental period. Future applications of this model will include molecular studies of the TME during early tumorigenesis, manipulation of the TME by injecting immune cells, and drug response investigations. In summary, we believe that the preclinical model described here will add to the repertoire of existing research tools and help elucidate molecular mechanisms of TME in ovarian cancer.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This study is funded in part by The Janet Burros Memorial Foundation. We acknowledge the patients and the Karmanos Cancer Institute Gynecologic Oncology Department for the collection of omentum samples. We also acknowledge the Biobank and Correlative Sciences Core at Karmanos Cancer Institute for coordination of patient recruitment and preparation of pathology slides. The Biobank and Correlative Sciences Core is supported in part by NIH Center grant P30 CA22453 to the Karmanos Cancer Institute at Wayne State University.
Materials
| 0.05% Trypsin-EDTA (1x) | Gibco | 25300054 | |
| 1 mL Insulin Syringe with 26 G detachable needle | BD | 329652 | |
| 10 mL Serological Pipets | CELLTREAT | 229010B | |
| 100 mm Tissue Culture Dish | Fisherbrand | FB012924 | |
| 15 mL Centrifuge Tube | CELLTREAT | 229411 | |
| 24 Well Cell Culture Plate | Costar | 3524 | |
| 50 mL Centrifuge Tube | CELLTREAT | 229421 | |
| 75 cm2 Tissue Culture Flask | CELLTREAT | 229341 | |
| Corning Cell Counter | Corning | 9819000 | |
| Cytation 5 imager | Biotek | ||
| DMEM/F12 (1:1) (1x), +L-Glutamine, +2.438 g/L Sodium Bicarbonate | Gibco | 11320033 | |
| Fetal Bovine Serum, Qualified | Gibco | 1043028 | |
| Matrigel | Corning | 356230 | Basement membrane matrix |
| No. 10 Stainless Steel Disposable Scalpel | Integra-Miltex | 4410 | |
| Penicillin Streptomycin | Gibco | 15140122 | |
| Phosphate Buffered Saline, pH 7.4 (1x) | Gibco | 10010023 | |
| Revolve microscope | Echo |
References
- Siegel, R. L., Miller, K. D., Wagle, N. S., Jemal, A. Cancer statistics. CA Cancer J Clin. 73 (1), 17-48 (2023).
- Berek, J. S., Renz, M., Kehoe, S., Kumar, L., Friedlander, M. Cancer of the ovary, fallopian tube, and peritoneum: 2021 update. Int J Gynaecol Obstet. 155 (Suppl 1), 61-85 (2021).
- Ledermann, J. A., et al. Newly diagnosed and relapsed epithelial ovarian carcinoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 24 (Suppl 6), vi24-32 (2013).
- Jelovac, D., Armstrong, D. K. Recent progress in the diagnosis and treatment of ovarian cancer. CA Cancer J Clin. 61 (3), 183-203 (2011).
- Morgan, R. J., et al. Ovarian cancer. Clinical practice guidelines in oncology. J Natl Compr Canc Netw. 6 (8), 766-794 (2008).
- Nieman, K. M., et al. Adipocytes promote ovarian cancer metastasis and provide energy for rapid tumor growth. Nat Med. 17 (11), 1498-1503 (2011).
- Motohara, T., et al. An evolving story of the metastatic voyage of ovarian cancer cells: cellular and molecular orchestration of the adipose-rich metastatic microenvironment. Oncogene. 38 (16), 2885-2898 (2019).
- Di Nicola, V. Omentum a powerful biological source in regenerative surgery. Regen Ther. 11, 182-191 (2019).
- Meza-Perez, S., Randall, T. D. Immunological functions of the omentum. Trends Immunol. 38 (7), 526-536 (2017).
- Liu, M., Silva-Sanchez, A., Randall, T. D., Meza-Perez, S. Specialized immune responses in the peritoneal cavity and omentum. J Leukoc Biol. 109 (4), 717-729 (2021).
- Lee, W., et al. Neutrophils facilitate ovarian cancer premetastatic niche formation in the omentum. J Exp Med. 216 (1), 176-194 (2019).
- Cardenas, C., et al. Adipocyte microenvironment promotes Bclxl expression and confers chemoresistance in ovarian cancer cells. Apoptosis. 22 (4), 558-569 (2017).
- Wu, Q., et al. Cancer-associated adipocytes: key players in breast cancer progression. J Hematol Oncol. 12 (1), 95 (2019).
- Zhang, Z., Scherer, P. E. Adipose tissue: The dysfunctional adipocyte – a cancer cell’s best friend. Nat Rev Endocrinol. 14 (3), 132-134 (2018).
- Alvero, A. B., et al. TRX-E-002-1 Induces c-Jun-dependent apoptosis in ovarian cancer stem cells and prevents recurrence in vivo. Mol Cancer Ther. 15 (6), 1279-1290 (2016).
- Alvero, A. B., et al. Novel approach for the detection of intraperitoneal micrometastasis using an ovarian cancer mouse model. Sci Rep. 7, 40989 (2017).
- Craveiro, V., et al. Phenotypic modifications in ovarian cancer stem cells following Paclitaxel treatment. Cancer Med. 2 (6), 751-762 (2013).
- Sumi, N. J., et al. Murine model for non-invasive imaging to detect and monitor ovarian cancer recurrence. J Vis Exp. (93), e51815 (2014).
- Agarwal, R., et al. Macrophage migration inhibitory factor expression in ovarian cancer. Am J Obstet Gynecol. 196 (4), 348.e1-348.e5 (2007).
- Kelly, M. G., et al. TLR-4 signaling promotes tumor growth and paclitaxel chemoresistance in ovarian cancer. Cancer Res. 66 (7), 3859-3868 (2006).
- Li, J., et al. CBX7 binds the E-box to inhibit TWIST-1 function and inhibit tumorigenicity and metastatic potential. Oncogene. 39 (20), 3965-3979 (2020).
- Tedja, R., et al. Generation of stable epithelial-mesenchymal hybrid cancer cells with tumorigenic potential. Cancers (Basel). 15 (3), 15030684 (2023).
- Dauleh, S., et al. Characterisation of cultured mesothelial cells derived from the murine adult omentum. PLoS One. 11 (7), e0158997 (2016).

