Murine Model of Central Venous Stenosis using Aortocaval Fistula with an Outflow Stenosis
Summary
An aortocaval fistula was created by puncturing the murine infra-renal aorta through both walls into the inferior vena cava and was followed by creation of a stenosis in its outflow via partial ligation of the inferior vena cava. This reproducible model can be used to study central venous stenosis.
Abstract
Central venous stenosis is an important entity contributing to arteriovenous fistula (AVF) failure. A murine AVF model was modified to create a partial ligation of the inferior vena cava (IVC) in the outflow of the fistula, mimicking central venous stenosis. Technical aspects of this model are introduced. The aorta and IVC are exposed, following an abdominal incision. The infra-renal aorta and IVC are dissected for proximal clamping, and the distal aorta is exposed for puncture. The IVC at the midpoint between the left renal vein and the aortic bifurcation is carefully dissected to place an 8-0 suture beneath the IVC. After clamping the aorta and IVC, an AVF is created by puncturing the infra-renal aorta through both walls into the IVC with a 25 G needle, followed by ligating a 22 G intra-venous (IV) catheter and IVC together. The catheter is then removed, creating a reproducible venous stenosis without occlusion. The aorta and IVC are unclamped after confirming primary hemostasis. This novel model of central vein stenosis is easy to perform, reproducible, and will facilitate studies on AVF failure.
Introduction
Arteriovenous fistulae (AVF) are the most common accesses for hemodialysis, with superior patency and reduced infection compared to other accesses such as grafts or central venous catheters. However, up to 60% of AVF fail to mature1,2,3; a recent systematic review reported that primary patency rates at 1 year were only 60%4. Stenosis along the venous outflow predominantly causes failure of AVF maturation5,6. There are certain characteristic locations prone to stenosis proximal to the fistula: the juxtaanastomotic swing segment for the radiocephalic fistula, the cephalic arch region for the brachiocephalic fistula and the central vein for the fistula with previously placed ipsilateral subclavian or internal jugular vein catheters7,8.
Central venous stenosis is often asymptomatic in patients without an AVF, but can cause ipsilateral extremity edema by venous hypertension as well as failure of fistula maturation when challenged by fistula flow9. The pathophysiology of central venous stenosis is most likely related to inflammation and the activated coagulation cascade after device placement. Furthermore, constant movement of the catheter tip as well as increased flow from the fistula can alter shear stress, resulting in platelet deposition and venous wall thickening10. To understand the basic mechanisms underlying AVF failure caused by central venous stenosis, an animal model mimicking central venous stenosis with an AVF is required.
We have established a murine aortocaval fistula model that is easy to perform and master and recapitulates the clinical course of human AVF.11 We applied the concepts and technique of several previously established murine models to create a novel murine AVF model with venous stenosis. We introduce a murine aortocaval fistula model with an IVC stenosis in the outflow fistula that can be used for the study of central venous stenosis.
Protocol
All experiments were performed with approval from the Yale University Institutional Animal Care and Use Committee (IACUC).
1. Anesthesia and pre-operative procedures
- Sterilize all surgical instruments and materials by autoclaving. Turn on the thermal support device to be certain it is warm (40–42 °C).
- Place a 9–11-week old C57BL/6 mouse into an acrylic induction chamber and anesthetize it with vaporized 2.5% isoflurane and 0.8 L/min oxygen. Anesthesia induction takes about 3 min.
- Remove the mouse from the chamber. Confirm a deep plane of anesthesia by a toe pinch, an ear pinch and a tail pinch. Place the mouse in supine position on the surgical area and deliver 2.5% isoflurane using silicone mask. Provide buprenorphine at 0.1 mg/kg analgesic and apply ophthalmic ointment to the eyes.
- Remove fur from the ventral side of the neck to the lower abdomen using Nair, a hair remover.
- Cleanse and disinfect the surgical site by using a two-step scrub with 10% povidone-iodine and 70% isopropanol. Apply a surgical drape.
2. Operative procedures
- Exposure of the clamp and puncture sites
- Prepare sterile instruments and wear sterile gloves to maintain sterility throughout the surgery.
- Make a skin-deep midline abdominal incision with a scalpel from the level of the lower liver edge to just above the pubis. Cut through the musculature with scissors to open the abdominal cavity.
- Insert a retractor into the abdomen and pull out the bowels to the right side. Keep them moist by wrapping in a saline-soaked gauze. Retreive the bladder and the seminal vesicles (in male mice) and pull them out to the caudal side. Dissect the mesentery between the rectum and retroperitoneum with a micro-needle holder to obtain a full view of the aorta and IVC.
- Dissect the infra-renal aorta and IVC en bloc from the lateral and dorsal surrounding retroperitoneal tissues with a micro-needle holder to cross-clamp them together.
- Dissect the surrounding tissues to expose the aortic puncture site at approximately three-quarters of the distance from the left renal vein to the aortic bifurcation.
- IVC dissection
- Dissect between the infra-renal IVC and aorta immediately distal to the left renal vein. Extend the dissection distally to the halfway between the left renal vein and the aortic bifurcation, so that the infra-renal IVC, both upstream and downstream to the stenosis, can be observed postoperatively.
NOTE: Blunt dissection between the IVC and aorta should be performed from immediately distal to the left renal vein where the connective tissue between the IVC and the aorta is relatively loose. - Make a window to separate the IVC from the aorta at that level and dissect the IVC from the surrounding tissue. Place an 8-0 polyamide monofilament suture firstly beneath the IVC and aorta (Figure 1A), then position the suture beneath only the IVC (Figure 1B) by pulling the suture end through the window.
NOTE: Since the IVC is fragile, dissecting along the aortic adventitia is useful to make a window to prevent the IVC as well as small IVC or aortic branches from being damaged. If bleeding occurs, it is likely to be uncontrollable. If the IVC has distinct side branches, place an 8-0 suture distally to the branches.
- Dissect between the infra-renal IVC and aorta immediately distal to the left renal vein. Extend the dissection distally to the halfway between the left renal vein and the aortic bifurcation, so that the infra-renal IVC, both upstream and downstream to the stenosis, can be observed postoperatively.
- AVF creation
- Bend a 25 G needle to a 45–60° angle at a point ~4 mm from the needle tip.
- Clamp the infra-renal aorta and IVC by applying a microsurgical clip.
- Rotate the aorta medially and caudally by grasping the connective tissue surrounding the bifurcation to expose the puncture site of the aorta stretched it slightly to the ventral side.
- Holding the aorta in a suitable position, puncture through the aorta into the IVC using the prepared 25 G needle (Figure 1C).
- Release the aorta and cover the puncture site with the surrounding tissue pulling up from the left side of the aorta. Take out the needle and press the puncture site gently using a cotton-tipped swab for hemostasis.
- Creation of the IVC stenosis
- Place a tip of a 22 G IV catheter (see the Table of Materials) onto the IVC longitudinally. Ligate the IV catheter and IVC together with an 8-0 suture (Figure 1D), and then remove the IV catheter.
- Confirm primary hemostasis (Figure 1E) and then unclamp the aorta and IVC. Cover the puncture site 1 min more to ensure hemostasis.
NOTE: Do not clamp for too long so as to avoid IVC thrombosis distal to the stenosis. - Return organs to their original positions and close the abdomen with 6-0 sutures.
3. Post-operative procedures
- After closure of the abdominal wound, discontinue isoflurane inhalation. Put the mouse into an individual bedding-free cage and place the cage on a thermal support device to prevent hypothermia.
NOTE: The mouse is observed until they achieve and maintain sternal recumbency. Apply post-operative care including analgesia and wound care in accordance with recommendations of the local IACUC. For analgesia we use buprenorphine at 0.1 mg/kg intrasmuscularly every 12 h for 48 h following the surgical procedures and thereafter as needed. - Confirm the AVF patency postoperatively by using Doppler ultrasound (see the Table of Materials). In addition, measure other vessel and flow characteristics as required.
Representative Results
Male mice underwent the operation mentioned above to create both an AVF and an IVC stenosis. Control mice underwent only laparotomy and dissection of the tissues surrounding the IVC, e.g., a sham procedure, or only creation of an IVC stenosis without simultaneous creation of an AVF.
The IVC was observed with Doppler ultrasound on day 7 after the surgical procedure (Figure 2). The fistula and stenosis areas of the IVC were easily detected in the longitudinal view (Figure 2C,E). The IVC between the fistula and the stenosis was dilated in mice having an AVF with the stenosis. The ultrasound waveforms were examined in the IVC at the point of the stenosis (Figure 2D,F). In mice bearing a stenosis alone, without an AVF, the stenosis segment showed a venous waveform with more spectral broadening than sham-operated mice but without much pulsatility. However, in mice having an AVF as well as a stenosis, the stenosis segment showed a pulsatile waveform in addition to spectral broadening. The time-averaged maximum velocity of the flow at the stenosis in mice having an AVF with stenosis was significantly higher than mice having stenosis alone (Table 1).
The Doppler ultrasound B mode was used in transverse views to assess the IVC on day seven after surgery (Table 1). The mean IVC diameter at the stenosis in mice having stenosis alone was similar to the mice having an AVF as well as the stenosis (Table 1). The percent stenosis of the IVC was calculated according to the NASCET method12. Using either the upstream segment or the downstream segment as the reference, the percent stenosis was significantly greater in mice having an AVF in addition to the stenosis (Table 1).
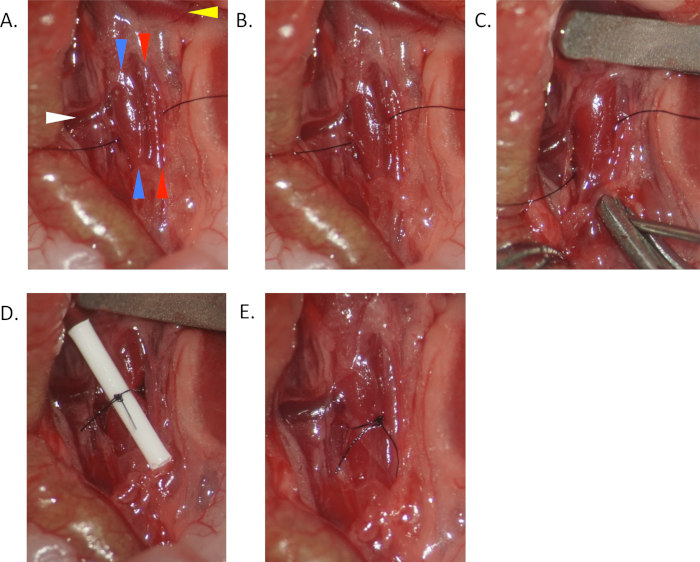
Figure 1. Operative photos of murine AVF model with venous stenosis. (A) Place an 8-0 suture beneath the IVC (blue arrowheads) and aorta (red arrowheads) halfway between the left renal vein (yellow arrowheads) and the aortic bifurcation, distally to any large IVC branches if present. (B) Place the suture beneath the IVC only. (C) After proximal clamping, puncture the aorta through both walls and into the IVC. (D) Tie a tip of a 22 G IV catheter and the IVC together with the placed suture. (E) Remove the catheter and unclamp. Arterial blood flow through IVC stenosis can be observed. Please click here to view a larger version of this figure.
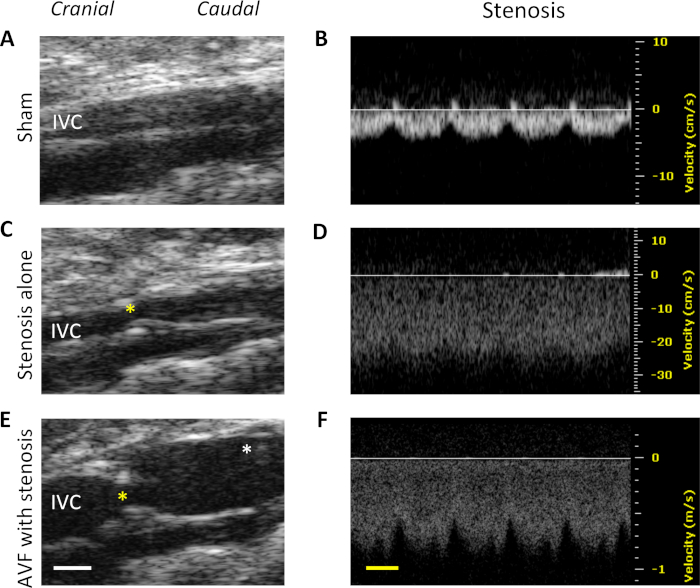
Figure 2. Ultrasound findings on day 7 after the surgical procedure. Top: representative images of mice with a sham procedure. (A) B-mode image shows IVC in the longitudinal view. The left side is the cranial side. (B) Waveform of the infrarenal IVC. Middle: representative images of mice with a stenosis alone. (C) B-mode image shows IVC including the stenosis (yellow asterisk) in the longitudinal view. The left side is the cranial side. (D) Waveform in the area of the stenosis. Bottom: Representative images of mice having AVF with stenosis. (E) B-mode image shows IVC including fistula (white asterisk) and stenosis. The left side is the cranial side. (F) Waveform in the area of the stenosis. White scale bar represents 1 mm. Yellow scale bar represents 100 ms. Please click here to view a larger version of this figure.
| Stenosis | Yes | Yes | P value |
| AVF | No | Yes | |
| Time-averaged maximum velocity (mm/s) | 180 | 878 | 0.0023 |
| Stenosis diameter (mm) | 0.62 ± 0.01 | 0.63 ± 0.01 | 0.3558 |
| % stenosis (upsteam) | 43% | 66% | 0.0159 |
| % stenosis (downsteam) | 42% | 56% | 0.0006 |
Table 1. Ultrasound measurement at the IVC stenosis area of each group. Ultrasound derived measurements at the IVC stenosis area of mice having stenosis alone and mice having AVF with stenosis on day 7 after surgery. %stenosis (upstream) = (1 – [diameter at stenosis / diameter at upstream reference segment]) x 100%. %stenosis (downstream) = (1 – [diameter at stenosis / diameter at downstream reference segment]) x 100%. %dilation = (diameter on postoperative day 7 / preoperative diameter at the same segment) x 100%. P values are based on Student’s t-tests, n = 4-6.
Discussion
The murine AVF model has been used to study the basic mechanisms and molecular events leading to AVF maturation13,14. In this study, we modified an established murine AVF model to create a novel murine aortocaval fistula model with an IVC stenosis in the outflow tract of the fistula. Our ligation model is similar to several previously described murine models that use vascular ligation. A murine model of deep vein thrombosis was created using partial IVC ligation with a 30 G needle spacer15; we used a larger 22 G IV catheter spacer to create a smaller stenosis and thereby avoid thrombotic occlusion. A murine model of partial carotid artery ligation was used to induce disturbed flow, leading to atherosclerosis16; our model similarly used a partial venous ligation and accordingly demonstrated disturbed flow in the IVC at the area of the partial ligation.
Mechanisms underlying AVF maturation failure caused by fistula venous stenosis have been studied. Hemodynamic changes including disturbed frequencies of shear stress were shown to be important factors17,18. A computational fluid dynamics simulation showed disturbed flow at the venous stenosis19, although animal models of AVF with venous stenosis have not been previously reported. This modified murine aortocaval fistula model can be used to study an AVF with central venous stenosis. The IVC diameter at the stenosis has less variation and more consistency in this model; partial IVC ligation using an IV catheter increases the reproducibility of this model. Clinical symptoms and signs of central vein stenosis often develop only after fistula creation in the ipsilateral extremity9. In this model, mice having a partial IVC stenosis (<50%) had normal flow and were asymptomatic, whereas addition of an AVF increased the degree of stenosis to a degree that could cause symptoms (>50%) (Figure 2, Table 1). These results mimic the phenotype of central vein stenosis; increased venous flow due to the presence of the fistula can unveil the existence of asymptomatic central vein stenosis, causing venous hypertension and failure of fistula maturation.
There are some critical steps and points to improve the success rate and consistency of the procedure. If the IVC has distinct side branches, an 8-0 suture is placed distally (caudally) to the branches (Figure 1). In the original murine AVF model, side branches of IVC are typically ignored because the higher vascular resistance of the branches keeps the fistula flow from entering the branches. However, if the IVC stenosis is created proximally to distinct side branches in this model, the fistula flow may escape into the branches due to vascular resistance by the newly placed suture. To avoid massive bleeding, the IVC dissection is started immediately inferiorly to the left renal vein and is extended further inferiorly to the point where the IVC is to be ligated. This step is the most critical part of this surgery; bleeding from damaged IVC or branches is likely to be uncontrollable. Furthermore, to avoid touching the IVC when placing the suture around it, and potentially tearing it, the 8-0 suture is initially placed around both the IVC and the aorta, and then repositioned beneath only the IVC. Lastly, the knot of the 8-0 suture is placed on the side of the IVC, not directly anteriorly, to prevent any artifact that could affect the postoperative ultrasound examination.
A potential limitation of this study is that the IVC stenosis in this model is created by external mechanical compression; adventitial inflammation caused by the suture and IVC dissection could potentially affect venous remodeling at the stenosis area. In addition, the fistula in this model is made between aorta and IVC so that all the fistula flow is directed into the IVC stenosis, whereas the fistula created in the human upper extremity often allows collateral veins to develop, keeping the stenosis asymptomatic. Physical signs of central venous stenosis such as distal edema and collateral formation are not shown in this model.
In summary, we introduce a protocol for a novel murine aortocaval fistula model with an IVC outflow stenosis that is easy to perform and reproducible. We expect that this model will be useful to study hemodynamic changes by a central venous stenosis that could affect AVF maturation.
Divulgations
The authors have nothing to disclose.
Acknowledgements
This work was supported by US National Institute of Health (NIH) Grant R01-HL128406; the United States Department of Veterans Affairs Biomedical Laboratory Research and Development Program Merit Review Award I01-BX002336; as well as with the resources and the use of facilities at the VA Connecticut Healthcare System, West Haven, CT.
Materials
| 20-60 Mhz scan head | VisualSonics Inc. | RMV-704 | |
| 8-0 Sterile Micro Suture, 6mm (140 µ), 3/8 Circle, TAP Point Needle | AROSuture | T06A08N14-13 | polyamide monofilament sutures |
| Induction Chamber, 2 Liter 3.75"W x 9.00"D x 3.75"H |
VetEquip | 941444 | |
| Isoflo, Isoflurane liquid | Zoetis | 26675-46-7 | |
| Mice, C57BL/6J | The Jackson Laboratory | 664 | |
| Pet Bed Microwave Heating Pad | Snuggle Safe | 6250 | |
| PrecisionGlide Needle 25G | BD | 305122 | |
| Surflo I.V. Catheter 22G | Terumo | SR-OX2225CA | 0.85mm outer diameter |
| Vascular clamp | Roboz Surgical Instrument | RS-5424 | |
| Vevo770 High Resolution Imaging System | VisualSonics Inc. | 770 |
References
- Dember, L. M., et al. Effect of clopidogrel on early failure of arteriovenous fistulas for hemodialysis: a randomized controlled trial. JAMA. 299 (18), 2164-2171 (2008).
- Dixon, B. S. Why don’t fistulas mature?. Kidney International. 70 (8), 1413-1422 (2006).
- Wilmink, T., Hollingworth, L., Powers, S., Allen, C., Dasgupta, I. Natural History of Common Autologous Arteriovenous Fistulae: Consequences for Planning of Dialysis. European Journal of Vascular and Endovascular Surgery. 51 (1), 134-140 (2016).
- Al-Jaishi, A. A., et al. Patency rates of the arteriovenous fistula for hemodialysis: a systematic review and meta-analysis. American Journal of Kidney Diseases. 63 (3), 464-478 (2014).
- Rocco, M. V., Bleyer, A. J., Burkart, J. M. Utilization of inpatient and outpatient resources for the management of hemodialysis access complications. American Journal of Kidney Diseases. 28 (2), 250-256 (1996).
- Roy-Chaudhury, P., Sukhatme, V. P., Cheung, A. K. Hemodialysis vascular access dysfunction: a cellular and molecular viewpoint. Journal of the American Society of Nephrology. 17 (4), 1112-1127 (2006).
- Quencer, K. B., Arici, M. Arteriovenous Fistulas and Their Characteristic Sites of Stenosis. AJR: American Journal of Roentgenology. 205 (4), 726-734 (2015).
- Kian, K., Asif, A. Cephalic arch stenosis. Semin Dial. 21 (1), 78-82 (2008).
- Agarwal, A. K. Central vein stenosis. American Journal of Kidney Diseases. 61 (6), 1001-1015 (2013).
- Glanz, S., et al. Axillary and subclavian vein stenosis: percutaneous angioplasty. Radiology. 168 (2), 371-373 (1988).
- Yamamoto, K., et al. The mouse aortocaval fistula recapitulates human arteriovenous fistula maturation. American Journal of Physiology: Heart and Circulatory Physiology. 305 (12), H1718-H1725 (2013).
- North American Symptomatic Carotid Endarterectomy Trial. Methods, patient characteristics, and progress. Stroke. 22 (6), 711-720 (1991).
- Kuwahara, G., et al. CD44 Promotes Inflammation and Extracellular Matrix Production During Arteriovenous Fistula Maturation. Arteriosclerosis, Thrombosis, and Vascular Biology. 37 (6), 1147-1156 (2017).
- Protack, C. D., et al. Eph-B4 regulates adaptive venous remodeling to improve arteriovenous fistula patency. Scientific Reports. 7 (1), 15386 (2017).
- Payne, H., Brill, A. Stenosis of the Inferior Vena Cava: A Murine Model of Deep Vein Thrombosis. J Vis Exp. (130), (2017).
- Nam, D., et al. Partial carotid ligation is a model of acutely induced disturbed flow, leading to rapid endothelial dysfunction and atherosclerosis. American Journal of Physiology: Heart and Circulatory Physiology. 297 (4), H1535-H1543 (2009).
- Ene-Iordache, B., Remuzzi, A. Disturbed flow in radial-cephalic arteriovenous fistulae for haemodialysis: low and oscillating shear stress locates the sites of stenosis. Nephrology, Dialysis, Transplantation. 27 (1), 358-368 (2012).
- Yamamoto, K., et al. Disturbed shear stress reduces Klf2 expression in arterial-venous fistulae in vivo. Physiological reports. 3, (2015).
- Remuzzi, A., Ene-Iordache, B. Novel paradigms for dialysis vascular access: upstream hemodynamics and vascular remodeling in dialysis access stenosis. Clinical Journal of the American Society of Nephrology. 8 (12), 2186-2193 (2013).

