Generation of Mesenchymal Stem Cells from Human Umbilical Cord Tissue and their Differentiation into the Skeletal Muscle Lineage
Summary
We describe a protocol for the isolation of mesenchymal stem cells from human umbilical cord tissue and their differentiation into the skeletal muscle lineage.
Abstract
Exploring the therapeutic potential of mesenchymal stem cells is contingent upon the ease of isolation, potency toward differentiation, and the reliability and robustness of the source. We describe here a stepwise protocol for the isolation of mesenchymal stem cells from human umbilical cord tissue (uMSCs), their immunophenotyping, and the propagation of such cultures over several passages. In this procedure, the viability of the uMSCs is high because there is no enzymatic digestion. Further, the removal of blood vessels, including the umbilical cord arteries and the vein, ensures that there is no contamination of cells of endothelial origin. Using flow cytometry, uMSCs upon isolation are CD45−CD34−, indicating an absence of cells from the hematopoietic lineage. Importantly, they express key surface markers, CD105, CD90, and CD73. Upon establishment of cultures, this paper describes an efficient method to induce differentiation in these uMSCs into the skeletal muscle lineage. A detailed analysis of myogenic progression in differentiated uMSCs reveals that uMSCs express Pax7, a marker for myogenic progenitors in the initial stages of differentiation, followed by the expression of MyoD and Myf5, and, finally, a terminal differentiation marker, myosin heavy chain (MyHC).
Introduction
The human umbilical cord has been credited to possess a robust reservoir of mesenchymal stem cells, which are currently being explored for regenerative therapies due to their robust proliferation and differentiation rates, immunomodulatory properties, and ability to generate cells from all the three germ layers1. The umbilical cord tissue consists of multiple compartments such as the umbilical cord blood, the umbilical vein subendothelium, and the Wharton’s jelly (WJ), which in itself encompasses three indistinct regions-the perivascular zone, the intervascular zone, and the sub-amnion or the cord lining (CL)2. While uMSCs can be isolated from all these different regions and broadly express key MSC markers, there is no clarity on whether these compartments contain the same population of uMSCs or display differences in their differentiation potencies3. Hence, protocols for the isolation of uMSCs require a greater precision in their mode and region of isolation, the robust characterization of differentiation potentials, and finally, a comparative analysis from different compartments of the cord.
In this context, few studies have demonstrated differences in uMSC proliferative and differentiative potentials between different parts of the cord. Of these, comparative analyses between uMSCs isolated from the CL and WJ regions revealed a greater proliferative potential in CL-derived uMSCs3,4. In a separate study, WJ-derived uMSCs performed better in proliferation assays compared to perivascular cells (HUCPV)5. In examining differences between cord blood-derived uMSCs and cord tissue-derived uMSCs devoid of vascular contamination, differential expression of key MSC markers was reported between the two compartments, as well as increased proliferation rates in cord tissue-derived uMSCs6.
Of the several studies examining the differentiation potentials of uMSCs primarily into tissues of the mesoderm lineage such as osteogenic, adipogenic, and chondrogenic lineages, very few have provided detailed protocols for myogenic differentiation and subsequent characterization, as well as comparative analyses between various cord compartments. In this context, we have developed a robust muscle differentiation protocol and observed that cord tissue-derived uMSCs display superior myogenic differentiation capabilities compared to cord blood6. Here, a stepwise protocol is detailed for the isolation of uMSCs from the whole cord tissue devoid of cells associated with the vasculature, their characterization, and their differentiation into the myogenic lineage.
Protocol
The use of umbilical cord tissue in this study was approved by the Institutional Committee for Stem Cell Research (IC-SCR), the Institutional Ethics Committee, Translational Health Science and Technology Institute (IEC-THSTI), the Institutional Ethics Committee of Civil Hospital, Gurugram, Haryana, and the Institutional Biosafety Committee, THSTI. Human cord tissue samples were harvested from term deliveries at the time of birth. Informed written consent was obtained from subjects . All methods were carried out in accordance with relevant guidelines and regulations.
1. Isolation of MSCs from cord tissue
- At the time of delivery, cut at least 5 cm of cord, preferably closer to the placenta, and sterilize the cord by swabbing the outer surface with 70% ethanol. Transfer the piece of cord tissue sequentially from one 50 mL collection tube containing phosphate-buffered saline (PBS) to another containing the same. Transport the collection tube bearing the name of the subject on ice to the laboratory within 1 h.
NOTE: For a larger study, it might be useful to barcode the samples to enable their tracking throughout the study. Importantly, all personnel handling human tissues should be offered the full regimen of the hepatitis B vaccine. - In the lab, switch on the UV for 25 min in the BSL-2 hood to sterilize autoclaved instruments and pipettes prior to use.
- Transfer the cord tissue piece from the collection tube to a 10 cm2 tissue culture-treated dish containing PBS enriched with 5 g/L glucose, 50 µg/mL gentamicin, 2.5 µg/mL amphotericin B, 100 U/mL penicillin, and 100 µg/mL streptomycin (schematic in Figure 1).
- Using a scalpel, slice the cord tissue vertically along its longitudinal axis to obtain two half cylindrical pieces. Owing to cord torsion and the mucoid surface, pin down the tissue with a pair of forceps held in the other hand.
- At this point, observe the umbilical arteries and vein and remove the blood vessels by using a scalpel to scrape them off in one direction from the surface. Rinse the cord tissue once again in PBS to remove all residual blood associated with the tissue. Ensure that the scraping is gentle to preserve the integrity of cells in the WJ surrounding the vessels.
- Mince each half of the cord tissue into 0.5 cm3 sized fragments and place the fragments with the luminal surface facing down on the dish. Incubate the dish briefly for 10 min in a 37 °C humidified chamber containing 5% CO2.
- After incubation, flood the dish containing the cord tissue pieces with 20 mL of medium containing MEM Alpha Modification without L-glutamine, ribo- and deoxyribonucleosides, 15% fetal bovine serum (not heat-inactivated), and 50 µg/mL gentamycin. Add the growth medium gently along the sides to prevent the tissue explants from being dislodged from their orientation. Add excess medium to account for a fraction that will be soaked up by the tissue explants during incubation.
- After 3 days of incubation, add fresh medium to the cultures. Ensure that the cultures are protected from shocks and movement of the explants while handling the dishes.
- After 1 week, remove the tissue fragments individually using sterile forceps and discard using appropriate biohazard bags for disposal. Retain the existing medium and add 10 mL of fresh growth medium. Replace the growth medium every 4 days until individual colonies reach a confluence of 70%.
NOTE: It is likely that the cells will not be uniformly distributed throughout the dish, as there will be individual proliferative colonies that need to be monitored for confluence with time. Generally, within a month, a 10 cm2 dish generates enough cells to be split into a separate dish. - Harvest the adherent cells using trypsin/EDTA solution (1x 0.25% trypsin and 0.02% EDTA in Hanks Balanced Salt Solution [HBSS]). Centrifuge the cell suspension at 470 × g for 5 min at 25 °C and resuspend the cell pellet in growth medium.
2. Immunophenotyping and propagation of uMSCS
- Proceed to immunophenotyping once the adherent cells have reached 50%-60% confluence and are well spread. Do not perform MSC marker analysis on fully confluent cultures, as this tends to cause downregulation of key MSC markers.
- After trypsinization, distribute a cell suspension of 1 × 106 cells/mL in FACS tubes (1 × 105 cells/tube) and stain with appropriate fluorophore-linked antibodies (all 1:50 dilution) in combination: unstained; CD105 + CD90; CD105 + CD73; CD105; CD90; CD73; CD34 + CD45 (common fluorophore); isotype controls for each fluorophore. Record a total number of events of at least 10,000 on the flow cytometer for further analysis.
NOTE: Since the cells are analyzed for each surface marker separately, gating on cell subsets is not required. - In addition to the above markers, confirm the presence of positive and negative surface markers in uMSC lines created from individual cord tissue samples (Table 1).
- Analyze the labeled cells by flow cytometry and determine the percentage of CD105+CD90+ and CD105+CD73+ cells. Analyze CD105+ and CD34−CD45− cells separately.
3. Differentiation of uMSCs into skeletal muscle
- Coat tissue culture plates with 0.01% collagen and 20 µg/mL laminin in PBS. Coat these plates for a minimum of 4 h at room temperature.
- Plate uMSCs at a density of 10,000 cells/cm2 in growth medium.
- When the cells are 70% confluent, aspirate the growth medium and rinse the cultures 2x with PBS. Add myogenic differentiation medium (M1) comprising of DMEM + 5% horse serum + 0.1 µM dexamethasone + 50 µM hydrocortisone to the uMSCs. For determination of the kinetics of myogenic progression, add M1 medium every other day to the cultures.
- To determine the kinetics of myogenic progression, analyze uMSCs for Pax7, MyoD, Myogenin, and MyHC expression at 2 days, 4-5 days, 6-7 days, and 10-14 days, respectively.
Representative Results
The success of isolation of uMSCs from cord tissue is >95%, unlike the poor rates of success from whole cord blood. Upon successful isolation of uMSCs, FACS analysis reveals that all the cells are CD34−CD45−CD105+CD90+. However, in comparative analysis, uMSCs isolated from cord blood display heterogeneous populations, wherein a proportion of cells show CD34+CD45+CD105+ (~15%). Additionally, double-positive CD105+CD90+ are fewer in number (~5%) (Supplemental Figure S1). This results in reduced levels of myogenic differentiation amongst uMSCs from cord blood, as both CD105 and CD90 expression are required for the induction of myogenesis. uMSCs also display the expression of the markers listed in Table 1. If there is contamination of the cord blood-derived uMSCs, there will also be a presence of CD34+CD45+ cells. This results in false cell counts for plating for myogenic differentiation. An indication that >90% of the cells are double positive for CD105 and CD90 expression is that the uMSCs have not committed to any mesodermal lineage and continue to remain multipotent, as both CD105 and CD90 expression are downregulated upon differentiation. It is imperative to use multiple markers for the confirmation of uMSC phenotypes, as there is no single definitive uMSC marker. In this analysis, we evaluated the presence of all the markers listed in Table 1 for each of the uMSC lines established in the laboratory. Additionally, we determined the double-positive status of CD105 and CD90 (Figure 2A), as well as of CD105 and CD73 (Figure 2B), ensuring that the uMSCs express multiple key markers. This is necessary to avoid contaminating single-positive cells that are present in numbers of less than 0.05%.
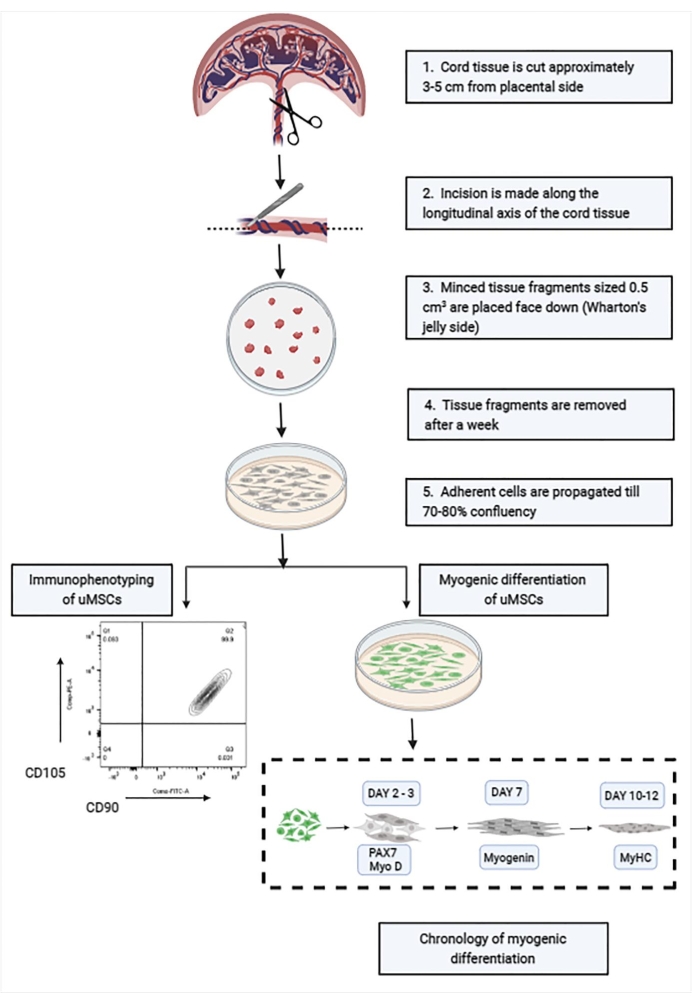
Figure 1: Schematic showing the stepwise isolation and characterization of uMSCs from cord tissue. Abbreviation: uMSCs = mesenchymal stem cells from human umbilical cord tissue. Please click here to view a larger version of this figure.
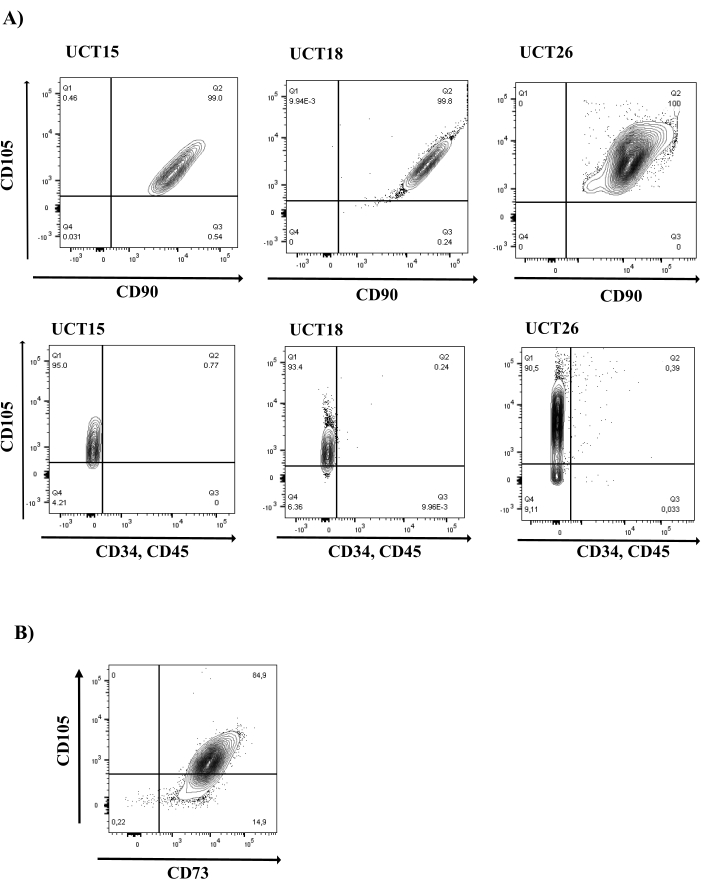
Figure 2: MSC marker analysis in cord tissue-derived uMSCs. (A) uMSCs display the expression of CD105 and CD90 and do not express hematopoietic markers, CD34 and CD45. Representative FACS plots of three uMSC lines (UCT15, UCT18, and UCT26) are shown (N = 16). Top row of panels shows cells in all three uMSC lines in the Q2 quadrant positive for CD105 and CD90 expression. Bottom row of panels shows cells in the Q1 quadrant positive for CD105 expression and negative for CD34 and CD45 expression. (B) uMSCs display the expression of MSC marker, CD73 (N = 16). Abbreviation: uMSCs = mesenchymal stem cells from human umbilical cord tissue. Please click here to view a larger version of this figure.
| uMSC positive markers | uMSC negative markers |
| CD105 | CD34 |
| CD90 | CD45 |
| CD73 | CD106 |
| CD29 | HLA DR |
| CD44 | CD31 |
| HLA ABC | CD14 |
| CD49e | CD49e |
| CD54 | |
| CD13 |
Table 1: List of positive and negative markers for uMSCs. Abbreviation: uMSCs = mesenchymal stem cells from human umbilical cord tissue.
For the differentiation of uMSCs into the myogenic lineage, uMSCs typically express Pax7, a marker for precursor cells within the first 2 days of the addition of M1, followed by MyoD within the first 4 days of M1 addition (Figure 3). At 6 days of differentiation, cells express Myogenin protein, followed by the expression of Myosin heavy chain (MyHC) between 10 days and 14 days of the induction of differentiation. We characterized in more detail the kinetics of myogenic expression using RNA sequencing, flow cytometry, immunocytochemistry, RT-PCR, and western blot analysis to document the stagewise expression of myogenic markers, confirming the robustness of this protocol. Whole-genome transcriptomic sequencing between undifferentiated uMSCs and uMSCs that were differentiated into skeletal muscle revealed the upregulation of 907 genes in response to the induction of myogenic differentiation (Figure 4).
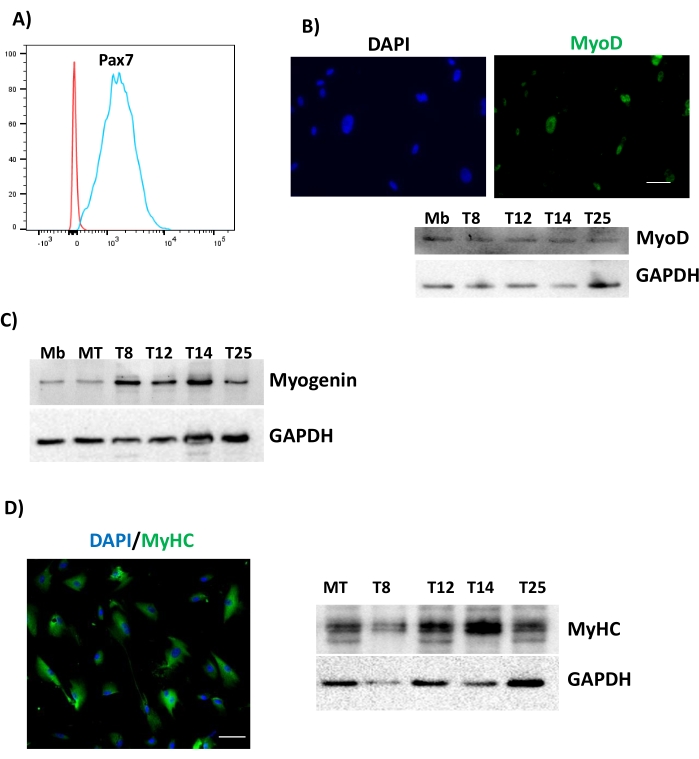
Figure 3: Differentiation of uMSCs into skeletal muscle. uMSCs were cultured in M1 medium for 2 days, 4 days, 7 days, and 10 days and assessed for (A) Pax7 after 2 days, (B) MyoD after 4 days, (C) Myogenin expression from different uMSC lines, denoted by T8, T12, T14, and T25 after 7 days, and (D) MyHC after 10 days. Scale bars = (B, D) 50 µm. Abbreviations: uMSCs = mesenchymal stem cells from human umbilical cord tissue; GAPDH = glyceraldehyde 3-phosphate dehydrogenase; MyoD = myoblast determination protein 1; MyHC = myosin heavy chain; DAPI = 4',6-diamidino-2-phenylindole; Mb = myoblast; MT = myotube. Please click here to view a larger version of this figure.
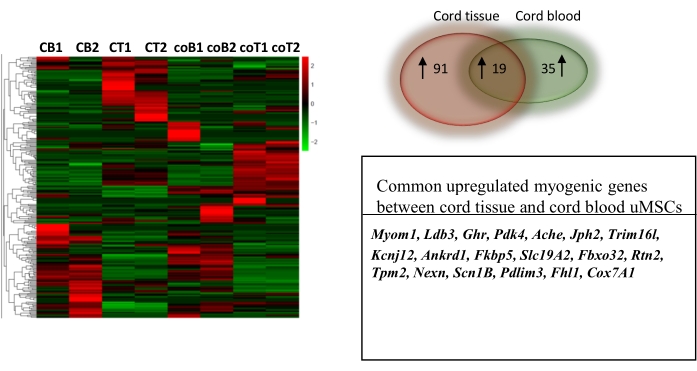
Figure 4: Comparative transcriptomic profiling of uMSCs derived from cord blood and cord tissue differentiated into skeletal muscle. Heat map of normalized counts of 907 genes between control uMSCs and uMSCs differentiated into skeletal muscle for 7 days from cord blood and cord tissue. Venn diagram (left) shows a greater number of myogenic genes upregulated in cord tissue-derived uMSCs compared to cord blood-derived uMSCs. Table below shows the common myogenic genes upregulated in both cord tissue and cord blood. This figure is from Mishra et al.6. Abbreviations: 1, 2 = biological replicates; CB1,2 = myogenic cells derived from uMSCs of cord blood; CT1, 2 = myogenic cells derived from uMSCs of cord tissue; coB1,2 = control undifferentiated uMSCs from cord blood; coT1, 2 = control undifferentiated uMSCs from cord tissue. Please click here to view a larger version of this figure.
For the purposes of conducting a comparative analysis, we compared uMSCs isolated from cord blood and cord tissue. RNA sequencing data revealed that there were more myogenic genes upregulated in uMSCs from cord tissue-derived myogenic cells than from those derived from cord blood (Figure 4). The RNA sequencing data used to support this study is uploaded to NCBI (SRA accession is GSE147114). Briefly, tissue-specific transcriptomic analysis using the PANTHER GO-slim database identified cytoskeletal proteins associated with actin binding and sarcomere assembly (TPM2, LDB3, PDLIM3, FHL1, NEXN, MYOM1) transporters associated with contractile function (RTN2, SLC19A2, ACHE, SCN1B, SLC19A2, JPH2, KCNJ12, ANKRD1), muscle mass maintenance (FBXO32, TRIM16L, GHR), calcium signaling (FKBP5), and enzymatic function (COX7A1, PDK4) (Figure 4). Altogether, these data demonstrate that cord tissue-derived uMSCs represent a compartment displaying robust myogenic potential.
Due to individual variation between uMSC lines that might arise from efficiencies in isolation, heterogeneity within the uMSC compartment, the age of the mother, and the mother's health status, including her nutrient levels, there might be differences in proliferation rates and myogenic potentials between established uMSC lines. However, despite differences in the kinetics of expression, the overall trend of increasing myogenicity with the stagewise expression of myogenic markers is maintained.
Supplemental Figure S1: MSC marker analysis in cord blood-derived uMSCs. uMSCs display the expression of CD105 and hematopoietic markers, CD34 and CD45. Analysis of the CD105+ population shows that only a small proportion of these cells co-express CD90 (N = 5). Abbreviation: uMSCs = mesenchymal stem cells from human umbilical cord tissue. Please click here to download this File.
Discussion
Critical steps
A critical step in this protocol is the collection of tissue under aseptic conditions, from the time of delivery to the maintenance of sterile cultures, for the entire duration of propagation. During cord collection, it is essential that the cord does not touch any non-sterilized surface and is externally swabbed with 70% ethanol before collection in tubes containing PBS supplemented with antibiotics. It is important to limit the time between cord collection and processing of the tissue for uMSC isolation. In case there is a need to transport tissue from the site of collection to the laboratory, care must be taken to maintain the tissue in antibiotic-containing buffers and store it on ice.
Modifications and troubleshooting of the method
The key modification in this protocol to induce myogenic differentiation of uMSCs is the coating of dishes with 0.01% type 1 collagen and 20 µg/mL laminin. We observed that myogenic progression in uMSCs in the presence of M1 medium is enhanced when adhesion conditions are also modulated. Whether the use of other superior, albeit expensive, matrices such as Matrigel might further improve upon this protocol needs to be tested. Variations in yield between individual samples might result in some tissues generating a lower cell count. In such instances, it might be preferable to collect a greater length of cord tissue that is >5 cm. In this context, few reports have used 10 cm of cord tissue to increase the yield of uMSCs. The majority of the reports describing the isolation of uMSCs from cord tissue have made use of extracellular matrix-degrading enzymes for the increased release of cells from the cord stroma3,5,7,8. The use of explant cultures by a few studies, including this report, has continually demonstrated increased cellular viability and yield6,9,10. Additionally, the absence of the need to perform cell sorting to purify cell populations, which is often included in purifying uMSCs from cord blood, increases cellular numbers and integrity.
Limitations of the method
A key limitation of the method is the time required for complete establishment of uMSC lines from individual cord tissue samples. Typically, 3 weeks are required to generate each uMSC line using this protocol. Following this, 2 weeks are required for complete myogenic differentiation. This extended duration of investigation can be cumbersome in large cohorts examining the differentiation potentials of uMSCs from different participants, with the intention of obtaining information on the intrauterine milieu or predicting offspring organ metabolic parameters such as body composition. A second limitation is the heterogeneity within the cord tissue matrix, which might possess intrinsic phenotypic differences between the various uMSC compartments and which could be responsible for differentiation potentials amongst the different sources. For instance, uMSCs from the WJ display lower osteogenic potential compared to CL-derived uMSCs11. Therefore, this method does not describe the differences inherent between different compartments within the cord tissue itself.
Significance of the method with respect to existing methods
Using this protocol, we are able to obtain a cell count of 1 × 104 to 1 × 106 uMSCs from individual cord tissue samples. These uMSC lines can be reliably used for assays for at least 6-8 passages. Despite the extent of variation in cellular phenotypes typical of human populations, the average doubling time of uMSCs observed in our cohort of 15 women from North India was less than 2 days6. An analysis of their proliferative rates using the incorporation of 5-ethynyl-2′-deoxyuridine (EdU) showed that at least 80% of the cells had gone through the S-phase in a span of 6 h6. Additionally, uMSCs from cord tissue also display low senescence rates, indicating the robustness of this method of isolation6. We previously compared the degree of myogenic induction in uMSCs using this protocol with the one used to induce myogenesis in human and murine pluripotential stem cells6,12. We found that this protocol is a more potent inducer of myogenic differentiation than existing protocols.
Importance of the method and applications
Successful cellular and regenerative therapies are dependent on cellular viability and yield, requiring large numbers of cells from early passages. Thus, this method offers a convenient alternative for clinical applications. The robust myogenic differentiation protocol provided in this report and the in-depth molecular characterization of myogenic progression using this protocol in our work complement the efforts to recapitulate fetal myogenesis and can be used as a model to mimic the intrauterine environment and reflect postnatal metabolism.
Declarações
The authors have nothing to disclose.
Acknowledgements
We thank Mr. Ojas Tikoo for their help with filming and video production. We also acknowledge the help received from the GARBH-Ini (Interdisciplinary Group on Advanced Research and Birth Outcome-DBT India) staff, nurses, and senior research officers at the Gurugram Civil Hospital and Dr. Pallavi Kshetrapal for help with logistics. This work was supported by grants awarded to Suchitra Gopinath from the Department of Biotechnology, India (BT/09/IYBA/2015; BT/PR29599/PFN/20/1393/2018).
Materials
| 4',6-diamidino-2-phenylindole (DAPI) | Thermo Fisher Scientific | D1306 | |
| Amphotericin B | Sigma Aldrich | A2411 | |
| Antibiotic solution 100x Liquid, endotoxin tested (10,000 U Penicillin and 10 mg Streptomycin/mL in 0.9% normal saline) | HiMedia | A001A-50mL | |
| Anti-GAPDH antibody | Sigma Aldrich | G8795 | |
| Anti-MyHC antibody (My32) | Novus Biologicals | NBP2-50401AF647 | |
| Anti-MyoD antibody (5.8A) | Novus Biologicals | NB100-56511 | |
| Anti-Myogenin antibody (Clone F5D) | Novus Biologicals | NBP2-34616AF594 | |
| Anti-Pax7 antibody | DSHB | DSHB-C1-576 | |
| APC Mouse anti-human CD90 clone 5E10 | BD Biosciences | 559869 | |
| Collagen Type 1 | Merck | C8919 | |
| D (+) Glucose | Sigma Aldrich | G7021 | |
| Dexamethasone | SIGMA | D4902 | |
| FACSCanto II or FACSAria III | BD Biosciences | ||
| Fetal Bovine Serum, qualified Brazil | GIBCO | 10270106 | not to be heat-inactivated |
| FITC Mouse anti-human CD106 clone 51-10C9 | BD Biosciences | 551146 | |
| FITC Mouse anti-human CD14 clone M5E2 | BD Biosciences | 557153 | |
| FITC Mouse anti-human CD31 clone WM59 | BD Biosciences | 557508 | |
| FITC Mouse anti-human CD34 clone 581 | BD Biosciences | 555821 | |
| FITC Mouse anti-human CD45 clone HI30 | BD Biosciences | 555482 | |
| FITC Mouse anti-human CD49D clone 9F10 | BD Biosciences | 560840 | |
| FITC Mouse anti-human CD90 clone 5E10 | BD Biosciences | 555595 | |
| FITC Mouse anti-human HLA-A,B,C clone G46-2.6 | BD Biosciences | 557348 | |
| FITC Mouse anti-human IgG clone G18-145 | BD Biosciences | 555786 | |
| FlowJo software | BD Biosciences | ||
| Gentamicin | Sigma Aldrich | G1264 | |
| Horse serum | HiMedia | RM1239 | |
| Hydrocortisone | Merck | H4001 | |
| Laminin | Merck | L2020 | |
| MEM Alpha Modification without L-glutamine, ribo- and deoxyribonucleosides | Hyclone | SH30568.FS | Basal medium for uMSCs |
| PE Mouse anti-human CD105 clone 266 | BD Biosciences | 560839 | |
| PE Mouse anti-human CD44 clone 515 | BD Biosciences | 550989 | |
| PE Mouse anti-human CD49E clone llA1 | BD Biosciences | 555617 | |
| PE Mouse anti-human IgG clone G18-145 | BD Biosciences | 555787 | |
| PE-Cy7 Mouse anti-human CD73 CLONE AD2 | BD Biosciences | 561258 | |
| Phosphate buffered saline (PBS), pH=7.4 | HiMedia | M1866 | |
| Trypsin/EDTA solution (1x 0.25% Trypsin and 0.02% EDTA in Hanks Balanced Salt Solution (HBSS) | HiMedia | TCL049-100mL |
Referências
- Kuroda, Y., et al. Unique multipotent cells in adult human mesenchymal cell populations. Proceedings of the National Academy of Sciences of the United States of America. 107 (19), 8639-8643 (2010).
- Troyer, D. L., Weiss, M. L. Wharton’s jelly-derived cells are a primitive stromal cell population. Stem Cells. 26 (3), 591-599 (2008).
- Karahuseyinoglu, S., et al. Biology of stem cells in human umbilical cord stroma: In situ and in vitro surveys. Stem Cells. 25 (2), 319-331 (2007).
- Kita, K., Gauglitz, G. G., Phan, T. T., Herndon, D. N., Jeschke, M. G. Isolation and characterization of mesenchymal stem cells from the sub-amniotic human umbilical cord lining membrane. Stem Cells and Development. 19 (4), 491-502 (2010).
- Sarugaser, R., Lickorish, D., Baksh, D., Hosseini, M. M., Davies, J. E. Human umbilical cord perivascular (HUCPV) cells: A source of mesenchymal progenitors. Stem Cells. 23 (2), 220-229 (2005).
- Mishra, S., et al. Umbilical cord tissue is a robust source for mesenchymal stem cells with enhanced myogenic differentiation potential compared to cord blood. Scientific Reports. 10 (1), 18978 (2020).
- Lu, L. L., et al. Isolation and characterization of human umbilical cord mesenchymal stem cells with hematopoiesis-supportive function and other potentials. Haematologica. 91 (8), 1017-1026 (2006).
- Seshareddy, K., Troyer, D., Weiss, M. L. Method to isolate mesenchymal-like cells from Wharton’s Jelly of umbilical cord. Methods in Cell Biology. 86, 101-119 (2008).
- Sotiropoulou, P. A., Perez, S. A., Salagianni, M., Baxevanis, C. N., Papamichail, M. Characterization of the optimal culture conditions for clinical scale production of human mesenchymal stem cells. Stem Cells. 24 (2), 462-471 (2006).
- Yoon, J. H., et al. Comparison of explant-derived and enzymatic digestion-derived MSCs and the growth factors from Wharton’s jelly. BioMed Research International. 2013, 428726 (2013).
- Ishige, I., et al. Comparison of mesenchymal stem cells derived from arterial, venous, and Wharton’s jelly explants of human umbilical cord. International Journal of Hematology. 90 (2), 261-269 (2009).
- Chal, J., et al. Differentiation of pluripotent stem cells to muscle fiber to model Duchenne muscular dystrophy. Nature Biotechnology. 33 (9), 962-969 (2015).

