Contact-Free Co-Culture Model for the Study of Innate Immune Cell Activation During Respiratory Virus Infection
Summary
This protocol details an investigation of the early interactions between virally infected nasal epithelial cells and innate cell activation. Individual subsets of immune cells can be distinguished based on their activation in response to viral infections. They can then be further investigated to determine their effects on early antiviral responses.
Abstract
The early interactions between the nasal epithelial layer and the innate immune cells during viral infections remains an under-explored area. The significance of innate immunity signaling in viral infections has increased substantially as patients with respiratory infections who exhibit high innate T cell activation show a better disease outcome. Hence, dissecting these early innate immune interactions allows the elucidation of the processes that govern them and may facilitate the development of potential therapeutic targets and strategies for dampening or even preventing early progression of viral infections. This protocol details a versatile model that can be used to study early crosstalk, interactions, and activation of innate immune cells from factors secreted by virally infected airway epithelial cells. Using an H3N2 influenza virus (A/Aichi/2/1968) as the representative virus model, innate cell activation of co-cultured peripheral blood mononuclear cells (PBMCs) has been analyzed using flow cytometry to investigate the subsets of cells that are activated by the soluble factors released from the epithelium in response to the viral infection. The results demonstrate the gating strategy for differentiating the subsets of cells and reveal the clear differences between the activated populations of PBMCs and their crosstalk with the control and infected epithelium. The activated subsets can then be further analyzed to determine their functions as well as molecular changes specific to the cells. Findings from such a crosstalk investigation may uncover factors that are important for the activation of vital innate cell populations, which are beneficial in controlling and suppressing the progression of viral infection. Furthermore, these factors can be universally applied to different viral diseases, especially to newly emerging viruses, to dampen the impact of such viruses when they first circulate in naïve human populations.
Introduction
Respiratory viruses are perhaps amongst the most widespread pathogens causing severe healthcare and economic burden. From the periodic global outbreaks of emerging epidemic strains (e.g., H1N1, H5N1, H3N2, MERS, COVID-19) to the seasonal strains of influenza every year, viruses are a constant threat to public health. Although vaccines form the main bulk of the response to these global public health challenges, it is sobering to note that these countermeasures are merely responsive1,2. Furthermore, a delay between the emergence of a new infectious strain and the successful development of its vaccine is inevitable3, leading to a period when measures available to curb the spread of the virus are highly limited.
These delays are further emphasized by the costs that are inflicted upon society-economically and socially. The seasonal flu alone is responsible for approximately $8 billion in indirect costs, $3.2 billion in medical costs, and 36.3 thousand deaths in the United States of America annually4. This is before consideration of the research costs that are necessary to fund vaccine development. Epidemic outbreaks have even more severe effects on society, compounded by the increasing rate of globalization every year, as evidenced by the global disruptions caused by the emergence and rapid spread of severe acute respiratory syndrome coronovirus 2 (SARS-CoV-2)5,6,7.
Recent studies have shown that infected patients having a greater population of activated innate T cells tend to have a better disease outcome8,9,10. Furthermore, the innate T cell population is categorized into multiple subgroups: the mucosal-associated invariant T (MAIT) cells, Vδ1 γδ T cells, Vδ2 γδ T cells, and the natural killer T (NKT) cells. These subgroups of innate T cells also exhibit heterogeneity within their populations, increasing the complexity of the interactions between the cell populations involved in the innate immune response11. Hence, the mechanism that activates these innate T cells and the knowledge of the specific subgroups of innate T cells may provide a different avenue of research to curtail the infectious effects of these viruses on the human host, especially during the period of vaccine development.
Epithelial cells infected by influenza produce factors that activate innate T cells rapidly12,13,14. Building upon that finding, this contact-free Air-Liquid Interface (ALI) co-culture model aims to mimic the early chemical interactions (mediated by soluble factors released by the infected epithelial layer) between the infected nasal epithelial layer and the PBMCs during early infection. The physical separation between the nasal epithelial layer (cultured on membrane inserts) and the PBMCs (in the chamber underneath) and the epithelial integrity prevent direct infection of the PBMCs by the virus, allowing a detailed study of the effects of epithelial-derived soluble factors on the PBMCs. The identified factors can therefore be further investigated for their therapeutic potential in inducing the appropriate innate T cell population that may protect against influenza infection. This paper therefore has detailed the methods of establishing a co-culture for the study of innate T-cell activation from epithelium-derived soluble factors.
Protocol
NOTE: Refer to Table 1 for recipes of media used in this protocol.
NOTE: hNECS grown on 12-well transwell have been found to grow into more optimal thickness for soluble factors to reach the basal chamber readily when infected with Influenza virus. Hence use of 12-well sized transwell for co-culture is recommended.
1. Establishment of the 3T3 feeder layer
- Establishment from frozen stocks
- Thaw a cryovial of NIH/3T3 fibroblasts from frozen stocks. Add the contents of the cryovial to 2 mL of complete Dulbecco's Minimal Essential Media (DMEM) and resuspend the cells.
- Centrifuge for 5 min at 300 × g and room temperature/pressure (rtp), and remove the supernatant. Resuspend the cells in complete DMEM.
- Count the cells using trypan blue staining. Add 10 µL of trypan blue to 10 µL of the resuspended cell suspension. Mix thoroughly, and add 10 µL of the suspension to a hemocytometer to count the cells.
- Seed cells at a density of 1 × 104 cells/cm2 in an appropriate culture dish (e.g., T75 flask). Incubate the resulting culture flask for 3 days at 37 °C in a 5% CO2 atmosphere.
- Mitomycin C treatment
- At 3 days, ensure confluency is 60%-80%, remove the medium, and wash the cells with 1x phosphate-buffered saline (PBS).
NOTE: It is important that the 3T3 feeder layer does not reach full confluency; otherwise, the mitomycin C treatment will not be effective. - Add mitomycin C-supplemented complete DMEM to the flask, and incubate for 3.5 h at 37 °C in a 5% CO2 atmosphere. Remove the mitomycin C-containing medium, and wash the cells 2x with 1x PBS.
- At 3 days, ensure confluency is 60%-80%, remove the medium, and wash the cells with 1x phosphate-buffered saline (PBS).
- Seeding 3T3 cells in 6-well plates
- Add 3 mL of 1x trypsin-EDTA to the flask for 3-5 min to disassociate the cells. Collect the disassociated cells in a fresh 15 mL tube. Centrifuge the 15 mL tube for 5 min at 300 × g, rtp; discard the supernatant. Resuspend the cells in complete DMEM.
- Count the cells using trypan blue staining. Seed the cells in a 6-well plate at 7.5 × 105-2.5 × 106 cells/well. Incubate the plate overnight at 37 °C in a 5% CO2 atmosphere.
NOTE: The 3T3 feeder layer is considered ready if the cells are healthy. At this point, seed the human nasal epithelial stem/progenitor cells (hNESPCs) onto the feeder layer for expansion. - Add Complete DMEM to the flask and incubate at 37°C, 5% CO2 overnight for 3T3 cells to recover from mitomycin C treatment.
2. Establishment of human nasal epithelial cell (hNEC) culture
NOTE: Clinical samples should be obtained from patients who are free of symptoms of upper respiratory tract infection.
- Processing nasal tissue into single-cell suspension
- Wash nasal tissue in 1x Dulbecco's PBS (dPBS) (PBS without Mg2+ and Ca2+) containing 100 µL/mL of an antibiotic-antimycotic mixture. Cut the tissue into small fragments, and treat the sample in 10 mg/mL of a neutral protease overnight at 4 °C with shaking.
- Centrifuge for 5 min at 200 × g, and remove the supernatant after centrifugation. Incubate the pellet in 1-2 mL of 1x trypsin-EDTA (37 °C, 15 min), and quench by adding a volume of fetal bovine serum equal to 10% of the volume in the tube.
- Mechanically dissociate the digested tissue into single-cell aggregates by pipetting, and then pass the resulting suspension through a 70 µm cell strainer. Resuspend the cells in complete DMEM.
NOTE: After this step, the cell suspension is a mixture of terminally differentiated cells and stem cells that are referred to as human nasal epithelial stem/progenitor cells (hNESPCs). The objective of the subsequent steps is to select for and enrich the hNESPC population from the mixture of different cell populations.
- Seeding a single-cell suspension onto the 3T3 feeder layer for selection of hNESPCs
- Centrifuge the cell suspension from step 2.1.3 (300 × g, 5 min, rtp), and remove the supernatant. Resuspend the cells in 3-5 mL of medium 3.
NOTE: Medium 3 is formulated to promote the selective growth of hNESPCs. - Count the cells via trypan blue staining. Seed 1 x 106 cells in 2mL of medium 3 per well onto 6-well plate containing prepared 3T3 feeder layer after removing the media in the 6 well plate. Incubate the resulting co-culture at 37 °C in a 5% CO2 atmosphere.
NOTE: After seeding, take care not to agitate the plate as it will affect the attachment of the hNESPCs. - Change medium 3 (2 mL) every 2-4 days by removing the old medium entirely and replacing it with fresh medium 3.
NOTE: Medium is changed to replenish nutrients and to prevent overly acidic conditions from negatively influencing the growth of the hNESPCs. The interval between each medium change depends on how acidic (yellow) the medium becomes. Intervals should be shortened if the medium turns acidic quickly. - After 7-10 days, observe that hNESPCs are at a confluency suitable for transferring them onto membrane inserts. See Figure 1 for representative morphology of hNESPCs at 3 different timepoints (2 days, 5 days, and 10 days).
- Centrifuge the cell suspension from step 2.1.3 (300 × g, 5 min, rtp), and remove the supernatant. Resuspend the cells in 3-5 mL of medium 3.
- Transferring hNESPCs onto membrane inserts
NOTE: Due to the mitomycin C treatment, the 3T3 feeder layer will slowly degrade over the hNESPC expansion period. This will result in a weakened adhesion to the surface of the well, allowing their dislodgement by flushing with a pipette, leaving behind only the healthy hNESPCs.- Remove the medium, and add 500 µL of 1x dPBS to each well. Flush the cells 3x with a micropipette to dislodge the 3T3 cells, and discard the 1x dPBS. Observe under the microscope that the round hNESPCs remain while the spindle-shaped 3T3 feeder layer is dislodged.
- Add 500 µL of a cell disassociation reagent per well, and incubate at 37 °C in a 5% CO2 atmosphere for 5-10 min, or until the hNESPCs have detached from the well surface.
- Collect the hNESPC suspension, centrifuge (300 × g, 5 min, rtp), and remove the supernatant.
- Resuspend the pellet in medium 3. Count the cells via trypan blue staining. Seed 3 × 104 cells in 150 µL of medium 3 per membrane insert (24-well plate) or 1 × 105 cells in 300 µL of medium 3 per membrane insert (12-well plate) (Figure 2). Incubate the cells at 37 °C in a 5% CO2 atmosphere.
- Change the medium (medium 3) of the apical and basal chambers every 2 days. Navigate a pipette tip between the supporting arms of the membrane insert to access the basal chamber, remove the old medium, and then reintroduce fresh medium by the same method. Although the apical chamber is readily accessible, take care not to disturb the growing hNESPC layer.
NOTE: Do not disturb the medium in the apical chamber for at least 2 days after seeding as the cells need time to attach to the membrane.
- Differentiation of hNESPCs into hNECs
- When hNESPCs reach 100% confluency (approximately 3-7 days from seeding on the membrane insert), start the ALI culture. Change the basal medium to differentiation medium, and remove the medium from the apical chamber. Only add medium to the basal chamber without adding it to the apical chamber when changing the medium every 2-3 days, as indicated in Figure 3 and step 2.3.5.
NOTE: Medium is changed to differentiation medium to promote the differentiation of the hNESPCs into hNECs in ALI. The hNESPCs take approximately 3-4 weeks to reach full maturity to become hNECs in ALI, at which point the cells would have grown into a multilayer with different populations of cells in each layer. Cilia should also be observed at a magnification of 400x (cilia can be identified by their beating movement, which cause the microscope field to appear like it is vibrating). At this point, the cells are ready to be used for the co-culture experiments. Refer to Figure 4 for the cross-section of a fully differentiated hNEC layer. - After obtaining mature hNECs, wash the cells in the apical chamber 3x with 1x dPBS at 2-3-day intervals for 1 week prior to the co-culture experiment. Synergize the wash step with the basal medium changes, and perform the washes as follows.
- Add 50 µL (24-well)/150 µL (12-well) of 1x dPBS into the apical chamber of the membrane insert, and incubate the cells at 37 °C for 10 min. Remove the dPBS after 10 min of incubation to remove accumulated mucus and dead cells over the course of differentiation.
NOTE: Depending on the nature of the experiment, sodium bicarbonate solution can be used to wash off the mucus layer entirely. However, for viral infection in co-culture experiments, the mucus layer is retained, and only excess mucus is removed with dPBS wash. This retention is to mimic the physiological mucus layer present on the nasal epithelia that will interact with the incoming viral infection.
- Add 50 µL (24-well)/150 µL (12-well) of 1x dPBS into the apical chamber of the membrane insert, and incubate the cells at 37 °C for 10 min. Remove the dPBS after 10 min of incubation to remove accumulated mucus and dead cells over the course of differentiation.
- When hNESPCs reach 100% confluency (approximately 3-7 days from seeding on the membrane insert), start the ALI culture. Change the basal medium to differentiation medium, and remove the medium from the apical chamber. Only add medium to the basal chamber without adding it to the apical chamber when changing the medium every 2-3 days, as indicated in Figure 3 and step 2.3.5.
3. Transepithelial electrical resistance (TEER) measurement
NOTE: Confirmation of epithelial integrity is important to ensure that an intact and healthy epithelial layer is obtained. An intact epithelial layer is determined through TEER measurement performed on 4 random wells using a voltohmmeter.
- Rinse the electrode with 70% ethanol, and sterilize it with ultraviolet light for 15 min before use to ensure sterility. Rinse with 1x dPBS after sterilization.
- Add 100 µL (for 24-well) or 300 µL (for 12-well) of 1x dPBS to the apical chamber of the membrane insert. Incubate the plate at 37 °C for 10 min; then, remove the dPBS.
- For each well to be measured, prepare an unused well with 1 mL (for 24-well) or 3 mL (for 12-well) of prewarmed (to 37 °C) differentiation medium. Place the membrane insert in the prepared well, and add 200 µL (for 24-well) or 600 µL (for 12-well) of prewarmed differentiation medium to the apical chamber. Equilibrate at 37 °C (subject to the incubation temperature of the type of virus added, e.g., 35 °C for Influenza) for 15 min.
NOTE: Prepare a blank (empty membrane insert) in the same way for the calculation of the TEER. - Equilibrate a 15 mL tube of prewarmed differentiation medium at the same temperature for 15 min as well. Place the electrodes in the 15 mL tube, and switch on the voltohmmeter.
NOTE: At this point, the reading should be 0 resistance, as the electrodes are in the same medium. If any other reading is obtained, equilibrate the electrode in the 15 mL tube until the reading is 0. - Starting from the blank, position the electrodes in each well such that one electrode is submerged in the apical chamber medium and the other in the basal chamber medium. Record the reading only when a constant reading is obtained for a period of at least 5 min.
- After each measurement, wash the electrode with PBS before the next measurement. For each well tested, take measurements for three samples at different positions of the membrane. To calculate the net TEER of each sample, subtract the background resistance, given by the blank membrane insert, from each measurement.
- Calculate the total TEER reading for a well using the following equation:
Epithelial Integrity (Ωcm2) = Net TEER(ohms) × Area of membrane (cm2)
NOTE: The TEER values of hNECs for viral infection experiments should be >1000 Ωcm2 13,15,16.
4. Isolation of peripheral blood monocytes and NK cells
NOTE: Blood samples should be obtained from healthy volunteers and used on the same day of isolation.
- Collect 30-40 mL of whole blood from each donor in 10 mL blood collection tubes.
- Isolate PBMCs using density gradient centrifugation, and obtain PBMCs from the buffy coat after the following steps (see also the Table of Materials).
- Thoroughly mix ~10 mL of blood from the blood collection tube in a vacutainer before diluting with an equal volume of balanced salt solution (PBS).
- Add 15 mL of density gradient medium to the base of a 50 mL tube.
NOTE: The ratio of density gradient medium to diluted blood should be 2:3-3.5. - Layer 35 mL of diluted blood on the density gradient medium with a pipette gun (with the dispense setting set to the lowest possible) by tilting the tube by 45° and allowing the diluted blood to fall dropwise onto the inner wall of the tube so that the layer of density gradient medium is not disturbed.
- Centrifuge lysate at 500 × g, 18-20 °C for 30 min (brake: off). Carefully remove and discard the upper plasma layer without disturbing the lower layer.
- Transfer the buffy coat to a new tube without mixing the red blood cell layer, gradient density medium layer, or the buffy coat. Once the buffy coat has been collected in a new 50 mL tube, top up the volume to 50 mL with 1x PBS.
- Centrifuge lysate at 800 × g, 18-20 °C, 8 min (brake: off), and remove the supernatant with a pipette gun. Resuspend the cell pellet with 50 mL of 1x PBS, and centrifuge at 120 × g, 18-20 °C, 10 min to remove platelets.
- Discard the supernatant by pipetting, without disturbing the cell pellet.
NOTE: As the cell pellet might be loose, it is inadvisable to discard the supernatant by pouring. - Resuspend the cell pellet with complete RPMI (Roswell Park Memorial Institute) medium. Perform a cell count by adding 10 µL of 3% acetic acid with methylene blue to 10 µL of the resuspended cell suspension. Mix thoroughly, and add 10 µL of the mixture to a hemocytometer to count the cells.
- Dilute PBMCs with complete RPMI medium to a density of 2 × 106/mL (for 24-well) or 4 × 106/mL (for 12-well).
5. hNEC Viral infection and transition to hNEC:PBMC co-culture
NOTE: H3N2 (A/Aichi/2/1968) is used as the representative strain of infection in this protocol. Multiplicity of infection (MOI) of 0.1 is used as the representative MOI in this protocol.
- Day 0 (Infection of hNECs)
NOTE: One well from the hNECs grown from the same donor is used to obtain a representative cell count for every well used in the experiment.- In the representative well, add 150 µL of 1x trypsin-EDTA to the apical chamber of the membrane insert and 350 µL of 1x trypsin-EDTA to the basal chamber, and incubate at 37 °C for 10 min, or until the cells detach from the membrane.
- Flush the cells on the membrane by pipetting up and down, and collect the suspension in a 1.5 mL centrifuge tube. Add 200 µL of complete DMEM to quench trypsin activity. Count cells via trypan blue staining to obtain the cell count per well.
- Calculate the required MOI of the virus based on the cell count per well, and dilute the virus stock accordingly with complete RPMI on ice.
NOTE: MOI 0.1 of 1.26 × 106 hNECs per well = 1.26 × 105 H3N2 viral particles per well in 30 µL (for 24-well)/100 µL (for 12-well) - For the remaining wells for the infection experiment, add 50 µL (for 24-well)/150 µL (for 12-well) of 1x dPBS into the apical chambers of the membrane inserts, incubate at 37 °C for 10 min, and remove the 1x dPBS.
- Change the basal medium in the membrane inserts to complete RPMI medium by transferring the inserts to a new plate with complete RPMI added to the wells (350 µL (for 24-well)/700 µL (for 12-well)).
NOTE: When hNESPCs have fully differentiated to hNECs, they are tolerant/permissive to different media for up to 72 h, with no changes to morphology or organization when the medium is switched to RPMI12. RPMI is used to support the growth and maintenance of the PBMC population. - Add the prepared 30 µL (for 24-well)/100 µL (for 12-well) of the virus inoculum into the apical chamber of the membrane insert, incubate at 35 °C in a 5% CO2 atmosphere for 1 h, and remove the viral inoculum from the apical chamber.
- Change the basal medium of membrane insert to fresh complete RPMI medium and incubate for at 35 °C in a 5% CO2 atmosphere for 24 h.
- Day 1 (establishment of hNECs + PBMCs co-culture)
- Seed the required number of PBMCs in 150 µL (for 24-well)/300 µL (for 12-well) of complete RPMI medium by directly adding the PBMC suspension into the basal chamber of each well of uninfected or infected hNECs from Day 0 (1.5 × 106 for 24-well plates and 3 × 106 for 12-well plates). Incubate at 37 °C for 24/48 h.
NOTE: The final volume in the basal chamber after the establishment of the co-culture is 500 µL (for 24-well)/1000 µL (for 12-well).
- Seed the required number of PBMCs in 150 µL (for 24-well)/300 µL (for 12-well) of complete RPMI medium by directly adding the PBMC suspension into the basal chamber of each well of uninfected or infected hNECs from Day 0 (1.5 × 106 for 24-well plates and 3 × 106 for 12-well plates). Incubate at 37 °C for 24/48 h.
- Days 2-3 (harvesting of PBMCs 48/72 h post-viral infection)
- Collection of apical supernatants (48/72 h post-viral infection)
- Add 50 µL (for 24-well)/150 µL (for 12-well) of 1x dPBS to each apical chamber, and incubate at 37 °C for 10 min. Collect the 1x dPBS in 1.5 mL tubes. Aliquot 25 µL (for 24-well)/50 µL (for 12-well) of the supernatant for plaque assay in a new 1.5 mL tube, and immediately freeze both the stock and the aliquots at -80 °C.
- Collection of cellular RNA from hNECs (48/72 h post-viral infection)
- Transfer the membrane insert to a clean well, add 300 µL (for 24-well)/600 µL (for 12-well) of RNA lysis buffer to the apical chamber, and incubate at rtp for 5 min. Collect the supernatant in a 1.5 mL centrifuge tube, and store it at -80 °C until RNA extraction for molecular analysis.
- Harvesting PBMCs (48/72 h post-viral infection)
- With the broad base of a sterile pipette tip, gently scrape the surface of the well to dislodge the activated PBMCs that may be adherent to the well surface. Collect the basal medium containing PBMCs in a 2 mL centrifuge tube.
- Flush the wells 2x with 300 µL of 1x dPBS, and collect the wash in the same 2 mL tube. Centrifuge the 2 mL tube (500 × g, 5 min, rtp), and collect the supernatant in a fresh 2 mL tube without disturbing cell pellet. Store the supernatant at -80 °C for cytokine and chemokine analysis; resuspend the cell pellet in 200 µL of 1x dPBS.
- Collection of apical supernatants (48/72 h post-viral infection)
6. Flow cytometry
NOTE: This section of the protocol is continued directly from the previous section using the PBMC cell suspension from step 5.3.3.2. Ensure minimal light exposure during the following steps in this section. A sample panel of surface staining markers can be found in Table 2.
- Surface staining
- Transfer the resuspended PBMC cell pellet into a 96-V bottom well plate. Centrifuge lysate at 800 × g for 3 min, and remove the supernatant.
- Incubate all the PBMCs (except for the "unstained") with 100 µL of a viability stain for 15 min at rtp. Top up to 200 µL with 150 µL of Magnetic-Activated Cell Sorting (MACS) buffer. Centrifuge lysate at 800 × g for 3 min, and discard the supernatant.
- Prepare a panel of surface staining antibodies of interest with appropriate dilution ratios and a final volume of 50 µL per reaction (top-up with MACS buffer to obtain the final volume). Perform surface staining by adding 50 µL of the prepared antibody mix to the cells using a multi-channel pipette. Incubate at 4 °C for 15 min in the dark.
- Wash by adding 150 µL of MACS buffer. Centrifuge lysate at 800 × g for 3 min, and discard the supernatant. If intracellular staining is not required, proceed directly to the 15 min incubation in step 6.3.
- Intracellular staining (If required)
- Add 100 µL of a fixation and permeabilization solution to each well. Incubate at 4 °C for 20 min in the dark. Top up the wells with 100 µL of 1x MACS buffer.
- Centrifuge (800 × g, 3 min, 25 °C), and remove the supernatant. Repeat the wash by adding 200 µL of 1x Permeabilization Wash buffer. Centrifuge (500 × g, 3 min, 25 °C), and remove the supernatant.
- Prepare the dilutions for the antibody panel of interest to achieve a final volume of 50 µL using 1x Permeabilization Wash buffer. Incubate on ice for 30 min in the dark. Add 200 µL of 1x Permeabilization Wash buffer.
- Centrifuge the cells (800 × g, 3 min, 4 °C), and remove the supernatant. Resuspend the cells in 100 µL of fluorescence-activated cell sorting buffer.
- Pipette 200 µL of a lysing solution into each well. Incubate for 15 min at rtp. Centrifuge lysate at 800 × g for 3 min and discard the supernatant.
- Resuspend the cell pellets in 200 µL of MACS buffer. Perform flow cytometry in accordance to the settings outlined previously13, or store at 4 °C in the dark.
7. Determination of cytokine and chemokine levels
- Process 25 µL of the basal chamber supernatant using an immunology multiplex assay according to the manufacturer's protocol18.
- Calculate the concentration of each analyte using multiplex manager software utilizing a curve-fitting algorithm (5 parameters) for the standard curve.
8. Assessment of viral contamination
- Extract viral RNA using an extraction kit on 4 sets of solutions: the stock H3N2 solution, the MOI 0.1 dilution for infection, the 10x serial dilutions of the MOI 0.1, and the basal medium from the samples (both 48 and 72 h post-viral infection)12.
- Select non-structural gene (NS1) and matrix (M1) as targets for polymerase chain reaction (PCR) (see the Table of Materials for primers used in the representative experiment).
- Perform reverse-transcription-PCR (RT-PCR) (42 °C, 60 min) to convert the viral RNA to cDNA before performing quantitative PCR (qPCR) to measure NS1 and M1 levels as a proxy for viral presence, and correlate the levels to the standard curve obtained from the RT-qPCR performed on the 10x serial dilution of the MOI 0.1 aliquot. Refer to Table 3 for the composition of the reaction mixes, and use the following conditions: preincubation at 95 °C for 10 min, followed by a 3-step amplification for 40 cycles: 95 °C for 10 s, 60 °C for 10 s, 72 °C for 30 s; melting curve: 95 °C for 10 s, 65°C for 60 s, and 97°C for 1 s.
9. Plaque assay
- Day 0: seeding MDCK (Madin Darby Canine Kidney) in 24-well plates
- Remove the medium from a T75 Flask of confluent MDCK cells. Wash 2x with 1x PBS to remove all traces of serum. Trypsinize the MDCK cells by adding 10 mL of trypsin and incubating at 37 °C in a 5% CO2 atmosphere for 20-30 min until the cells detach.
NOTE: Do not tap the flask as this might result in clumping. - Pipette the cell suspension into a 15 mL tube containing 2 mL of complete Eagle's Minimal Essential Medium (EMEM). Centrifuge (300 × g, 5 min, rtp), and remove the supernatant.
- Resuspend the cells in 6 mL of complete EMEM. Count the cells by trypan blue staining.
- Dilute the MDCK cell suspension to a concentration of 1 × 105 cells/mL, and seed 1 mL of the diluted suspension in each well of a sterile 24-well plate. Incubate at 37 °C in a 5% CO2 atmosphere for 24 h to obtain a confluent monolayer of MDCK cells in each well.
- Remove the medium from a T75 Flask of confluent MDCK cells. Wash 2x with 1x PBS to remove all traces of serum. Trypsinize the MDCK cells by adding 10 mL of trypsin and incubating at 37 °C in a 5% CO2 atmosphere for 20-30 min until the cells detach.
- Day 1: infection of MDCK cells
- Prepare the infection medium. Remove the medium from the MDCK monolayer in the 24-well plate, and wash 2x with 1x dPBS. For the second wash, leave the PBS in the wells while preparing serial dilutions of the virus.
- Thaw the virus samples on ice, and serially dilute them in a 24-well plate to achieve serial dilutions from 10-1 to 10-6.
NOTE: As an example, fill each well in a 24-well plate with 270 µL of infection medium. - Add 30 µL of the virus sample to the first well in the row. With a new pipette tip, mix well and transfer to the next well in the row to dilute the sample by 10x. Proceed until 10-6 dilution has been achieved; perform steps 9.2.1-9.2.3 for all virus samples.
- Remove PBS from the MDCK plate, and infect in duplicate with 100 µL of the prepared viral dilutions. For control wells, add 100 µL of the infection medium (without the viral sample). Incubate at 35 °C in a 5% CO2 atmosphere for 1 h, shaking the plate to eliminate dry spots every 15 min.
- Remove the viral inoculum, and add 1 mL of liquid overlay for each well. Incubate at 35 °C in a 5% CO2 atmosphere for 72 h.
- Day 4 (72 h post-infection): plaque visualization
- Remove the liquid overlay, and fix the cells with 4% formaldehyde in 1x PBS for 1 h. Remove the formaldehyde solution, and wash once with 1x PBS or distilled water.
- Stain the fixed cells by adding 1% crystal violet solution for 15 min. Remove the crystal violet dye, and wash the cells with running water. Dry the plate at rtp.
- Once dry, count plaques, and calculate the viral titer according to the following formula:
Number of Plaques × Dilution Factor = Number of Plaque – Forming Units in 100 μL
Representative Results
Although conventional T cells form the main repertoire of adaptive immune response against viral infection to facilitate viral clearance, the innate T cell population works across a broader spectrum to suppress the viral load for effective clearance at a later stage. Therefore, this protocol specifically creates a robust condition to study innate T cells, their activation, and their functional population following influenza infection, without needing epithelial and immune cell samples from the same donor. This protocol can also be applied to other viruses, although it may be limited to viruses with apical release, i.e., no virus should enter the basal layer to come into contact with the PBMC compartment.
Based on the representative results in Figure 1, this protocol can help to obtain hNESPC populations grown from a primary cell suspension in a 3T3 feeder layer. Figure 1 provides a sample of the expected progression of the hNESPCs as they grow on the 3T3 feeder layer. These cells will be used for differentiation in the ALI culture to obtain multilayered hNECs, complete with functional ciliated and goblet cells (Figure 4). Using the hNECs, innate T-cell activation can be investigated using flow cytometry. The results shown in Figure 5 show the detection of MAIT cell, γδ-T cell, and NK cell populations, which were significantly increased in co-culture involving hNECs infected with influenza virus. This setup can then be applied to other strains of the influenza virus to tease out the universal population across strains, as well as other viruses and their ability to activate innate T cell populations. In addition, the detection panel can also be customized according to the innate immune cell population of interest to observe their respective activation under co-culture conditions with infected epithelial cells.
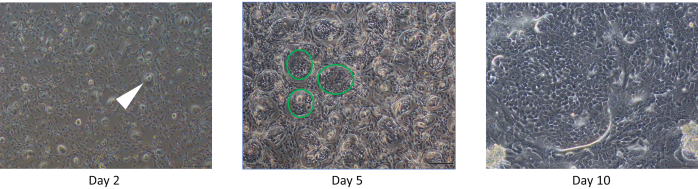
Figure 1: hNESPCs grown on a 3T3 feeder layer 2/5/10 days from seeding. Day 2: Note the islets of hNESPCs (an example is demarcated with a white arrow) that should be observed 2 days after seeding on the 3T3 feeder layer. Day 5: The islets observed on Day 2 should now be larger (examples of islands of hNESPCs are demarcated by green circles), and the 3T3 layer should be observed to be degenerating. Day 10: The hNECPSs should be dominating the entire plate with little or no 3T3 cells visible. Scale bars for Day 2 and Day 5 = 50 µm based on a magnification of 200x, scale bar for Day 10 = 100 µm based on a magnification of 100x. Abbreviation: hNESPCs = human nasal epithelium stem/progenitor cells. Please click here to view a larger version of this figure.
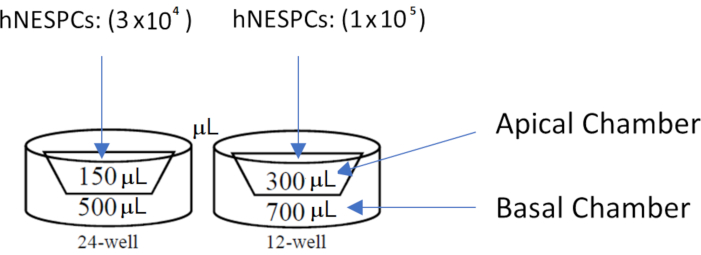
Figure 2: Well diagrams for membrane inserts in 24-well and 12-well plates. Note the medium volume to be used for each compartment. hNESPCs are seeded in the apical chambers of the membrane inserts. Abbreviation: hNESPCs = human nasal epithelium stem/progenitor cells. Please click here to view a larger version of this figure.
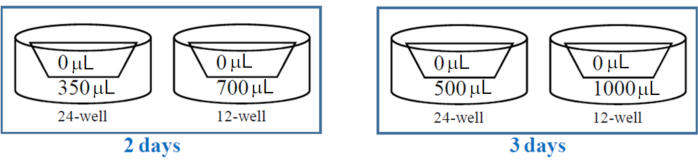
Figure 3: Well diagrams for membrane inserts in 24-well and 12-well plates for ALI co-culture establishment. Note the medium volume to be used for each compartment. Note the differences in medium volume to be used for the different intervals (2 days/3 days) between medium changes. Abbreviation: ALI = air-liquid interface. Please click here to view a larger version of this figure.
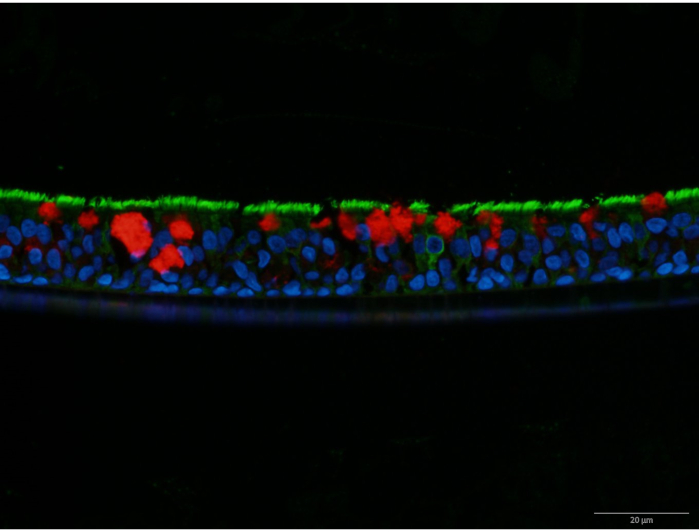
Figure 4: β4-Tubulin and MUC5AC co-stain of an hNEC layer. β4-Tubulin is stained in green, while MUC5AC is stained in red. The nuclei are stained in blue with DAPI. MUC5AC indicates the presence of mucus-producing goblet cells, while β4-tubulin indicates the presence of cilia on ciliated cells. Scale bar = 20 µm based on 600x magnification. Abbreviations: hNEC = human nasal epithelial cell; MUC5AC = mucin 5AC; DAPI = 4′,6-diamidino-2-phenylindole. Please click here to view a larger version of this figure.
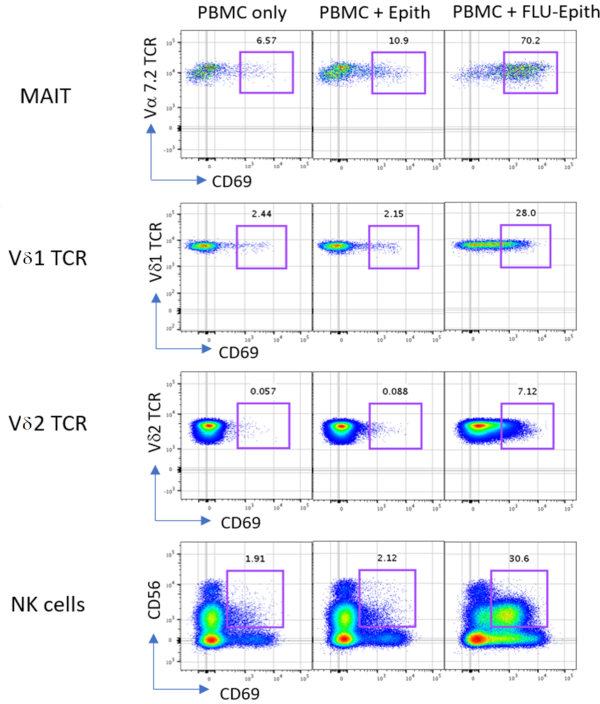
Figure 5: Representative results of PBMCs incubated with or without nasal epithelium or influenza-infected epithelium for 24 h. Activation of MAIT, Vδ1 T cells, Vδ2 T cells, and NK cells was determined by cell-type-specific markers including Vα 7.2 TCR, Vδ1 TCR, Vδ2 TCR, CD56, and CD69 staining. The values above the gates indicate the percentage of CD69-positive cells. Abbreviations: PBMCs = peripheral blood mononuclear cells; Epith = nasal epithelium; FLU-Epith = influenza-infected epithelium; MAIT = mucosal-associated invariant T cells; NK = natural killer; TCR = T-cell receptor; CD = cluster of differentiation. Please click here to view a larger version of this figure.
| Medium | Recipe | Composition | Comments |
| Medium 3 | DMEM/Nutrient Mixture F-12 | 500 mL | |
| Human Epithelial Growth Factor | 5 ng/mL | ||
| Insulin | 2.5 µg/mL | ||
| Cholera Toxin | 0.1 nM | ||
| Hydrocortisone | 0.5 µg/mL | ||
| 3,3',5-triiodo-l-thyronine | 2 nM | ||
| N-2 supplement | 5 mL | 10 µL/mL | |
| Antibiotic-Antimycotic | 5 mL | ||
| Differentiation Media | PneumaCult-ALI Basal Medium | 441 mL | |
| PneumaCult-ALI 10x Supplement | 50 mL | ||
| Hydrocortisone Solution (200x) | 2.5 mL | ||
| 0.2% (2 mg/mL; 1000 IU/mL) Heparin Sodium Salt in Phosphate-Buffered Saline | 1 mL | ||
| Antibiotic-Antimycotic (100x) | 5 mL | ||
| PneumaCult-ALI Maintenance Supplement (100x) | 500 µL | Only to be added right before use | |
| Complete Dulbecco's Minimal Essential Medium (DMEM) | DMEM/High Glucose | 450 mL | |
| Heat-inactivated Fetal Bovine Serum | 50 mL | ||
| Antibiotic-Antimycotic (100x) | 5 mL | ||
| Complete Roswell Park Memorial Institute (RPMI) Medium | RPMI 1640 (w L-Glutamine) | 445 mL | |
| Heat-inactivated Fetal Bovine Serum | 50 mL | ||
| Antibiotic-Antimycotic (100x) | 5 mL | ||
| Complete Eagle's Minimal Essential Medium (EMEM) | EMEM (w L-Glutamine) | 450 mL | |
| Heat-inactivated Fetal Bovine Serum | 50 mL | ||
| Infection Medium | EMEM (w L-Glutamine) | 4 mL | |
| TPCK Trypsin (500 µg/mL) | 8 µL | Final TPCK Trypsin Concentration of 1 µg/mL | |
| Magnetic-Activated Cell Sorting Buffer | 1x PBS | 498 mL | |
| 0.5 M EDTA | 2 mL | ||
| BSA (Tissue Culture Grade) | 2.5 g | ||
| Mitomycin C-Supplemented Complete DMEM | Complete DMEM | 10 mL | |
| Mitomycin C | 500 μL | Mitomycin C (10 µg/mL) |
Table 1: Recipe for media used.
| Cell surface marker | Fluorophore |
| Vδ1 T-cell receptor (TCR) | Fluorescein isothiocyanate (FITC) |
| Vδ2 TCR | Peridinin-cholorphyll-protein (PerCP) |
| CD3 | V500 |
| CD8 | Allophycocyanin-Cyanine 7 dye (APC-Cy7) |
| CD14 | Phycoerythrin (PE)-CF594 |
| CD56 | Phycoerythrin (PE)-Cyanine 7 (Cy7) |
| CD69 | Brilliant Violet 421 (BV421) |
| CD83 | Allophycocyanin (APC) |
| CD161 | Brilliant Violet 605 (BV605) |
| Vα 7.2 | Phycoerythrin (PE) |
| CD38 | Brilliant UltraViolet 395 (BUV395) |
Table 2: Sample surface staining markers.
| qPCR Reaction Mix | qPCR Master Mix | 5 µL |
| Nuclease-free Water | 3 µL | |
| Forward Primer (1 mM) | 0.5 µL | |
| Reverse Primer (1 mM) | 0.5 µL | |
| cDNA (12.5 ng/µL) | 1 µL | |
| Total Reaction Volume | 10 µL | |
| RT-PCR Reaction Mix | RT-PCR 5x Buffer | 2.5 µL |
| Random Primers (500 ng/µL) | 0.2 µL | |
| RNase Inhibitor | 0.625 µL | |
| dNTP Mix | 2.5 µL | |
| Reverse Transcriptase | 0.5 µL | |
| RNA (200 ng/µL) | 1 µL | |
| Nuclease-Free Water | 12.675 µL | |
| Total Reaction Volume | 20 µL |
Table 3: Recipe for reaction mixes of reverse-transcription polymerase chain reaction (RT-PCR) and quantitative PCR (qPCR).
Discussion
Innate immune responses against viruses are an under-investigated field of study in antiviral management. The airway epithelial cells and innate immune cells work in concert to suppress viral replication during an infection, besides serving as a determinant of overactive adaptive response if the viral load is not kept in check12,13,17. However, the development of a relevant human model for the study of epithelial-innate immune crosstalk to investigate the activation of innate immune cells to confer an appropriate antiviral response remains a challenge. Hence, this ALI co-culture model represents a versatile technique that can be used to assess a whole host of interactions between the nasal epithelial layer and the immune cells. As this model combines in-vitro-differentiated hNECs, PBMC activation analysis via flow cytometry, and viral infection, many of the crucial steps have been clearly demarcated to ensure the success of this protocol. In addition, further modification can also be done to the part of the airway involved where in-vitro–differentiated cells from both the upper and lower airways can be used, adding another layer of versatility to the protocol.
However, when working with epithelial-immune cell crosstalk in viral infection, it is critical that the viruses do not interact directly with the PBMCs to identify early local epithelial-derived soluble factors released by the hNECs. Therefore, this model is more suitable for examining viruses with polarized viral release, wherein viruses only bud out from the apical surface into the apical chamber, e.g., influenza viruses12 and SARS-CoV-2 virus19. In addition, to prevent leakage of apical-release viruses into the basal chamber compromising the experiment, an intact epithelial layer of sufficient thickness is vital. Therefore, it is important that TEER measurement and viral RNA quantification be performed to ensure that the results are free of viral leakages into the basal chamber13,16,20. A TEER reading of >1000 implies an intact multilayer of cells suitable for viruses with polarized release; the basal media should be free of any viral RNA contamination13,15,16. However, the utility of the model for bidirectional release viruses, such as rhinoviruses, remains to be explored16. Such viruses are not limited to releasing their progeny in a polarized manner and may bidirectionally release new viruses into both apical and basal regions of the epithelium. Further optimization is required before this model can be applied to viruses with non-polarized release.
As this protocol involves working with human samples from different individuals, no two samples of hNECs will exhibit the same properties and responses12,16. For example, the viscosity of the mucus produced by the terminally differentiated hNEC layer could differ greatly. The speed of cilia development may also be different. It is important, therefore, to exercise some level of flexibility when adhering to the guidelines laid out in this protocol. While it is certainly possible to utilize epithelial cell lines, this would remove the complexity (mucus, interactions between different cell types) of the interactions between the different cell types of the epithelial layer, which would be ideal for investigation of how epithelial crosstalk influences the responses of the PBMCs. A primary cell line is necessary to mimic the physiology of the nasal tissues, where the cells are multilayered, and the different cell types are localized to their own individual niche, although variability might be an issue. Variability in this respect can be overcome by utilizing single-cell RNA sequencing to differentiate and separate the heterogenous population of cells.
The types of interactions that can be assessed are indeed limited by the origin of the PBMCs and the hNECs. When the PBMCs and hNECs are obtained from different donors, ensuring epithelial integrity and separation is crucial. When PBMCs come into contact with hNECs, allogenic immune reactions could occur. Hence, the only interactions that are relevant are interactions mediated by soluble factors that can pass through the membrane inserts, as has been described in the protocol above. However, when both populations of cells originate from the same individual, this model has an added layer of utility as conventional immune cell reactions between the hNECs and the PBMC population can now be assessed, including T-cell-mediated cytotoxicity and antibody-mediated responses. In addition, epigenetic studies can also be performed to examine how modifications to the genome may affect cytokine gene/protein expression/secretion.
Furthermore, different cell populations can be added to the basal chamber to further investigate a specific population. This can be performed by isolating the cell populations of interest (T cells, NK cells, monocytes) and introducing them to the basal chamber instead of the PBMCs. However, this model cannot be used to investigate cellular interactions that require direct contact owing to the separation of the two cell populations by the membrane. As such, the investigation of adaptive immune responses may be limited by this detail. In conclusion, this ALI co-culture model offers a versatile starting point for the in vitro investigation of the crosstalk between nasal tissues and immune cells. The protocol described in this manuscript attempts to provide a guideline that will be helpful even if the populations/conditions are altered.
Disclosures
The authors have nothing to disclose.
Acknowledgements
We would like to thank the research staff in NUS Department of Otolaryngology and Department of Microbiology and Immunology for their help with the hNEC culture- and viral-culture-related work. We would also like to thank the surgeons and surgical team in National University Hospital, Department of Otolaryngology, for their assistance in providing the cell and blood samples required for the study.
This study was funded by National Medical Research Council, Singapore No. NMRC/CIRG/1458/2016 (to De Yun Wang) and MOH-OFYIRG19may-0007 (to Kai Sen Tan). Kai Sen Tan is a recipient of fellowship support from European Allergy and Clinical Immunology (EAACI) Research Fellowship 2019.
Materials
| 0.5% Trypsin-EDTA | Gibco | 15400-054 | |
| 0.5 M Ethylenediaminetetraacetic acid (EDTA), pH 8.0, RNase-free | Thermofisher | AM9260G | 0.5M EDTA |
| 1.5 mL SafeLock Tubes | Eppendorf | 0030120086 | 1.5mL Centrifuge Tube |
| 10 mL K3EDTA Vacutainer Tubes | BD | 366643 | 10mL Blood Collection Tubes |
| 10x dPBS | Gibco | 14200-075 | |
| 10x PBS | Vivantis | PC0711 | |
| 12-well Plate | Corning | 3513 | |
| 12-well Transwell Insert | Corning | 3460 | membrane insert |
| 1x FACS Lysing Solution | BD | 349202 | |
| 2.0 mL SafeLock Tubes | Eppendorf | 0030120094 | 2 mL centrifuge tube |
| 24-well Plate | Corning | 3524 | |
| 24-well Transwell Insert | Corning | 3470 | |
| 3% Acetic Acid with Methylene Blue | STEMCELL Technologies | 07060 | |
| 3,3',5-triiodo-l-thyronine | Sigma | T-074 | |
| 37% Formaldehyde Solution w 15% Methanol as Stabilizer in H2O | Sigma | 533998 | |
| 5810R Centrifuge | Eppendorf | 5811000320 | |
| 5 mL polypropylene tubes (flow tubes) | BD | 352058 | |
| 70 µm Cell Strainer | Corning | 431751 | |
| A-4-62 Rotor | Eppendorf | 5810709008 | |
| Accutase | Gibco | A1110501 | Cell Dissociation Reagent |
| Antibiotic-Antimycotic | Gibco | 15240-062 | |
| Avicel CL-611 | FMC Biopolymer | NA | Liquid Overlay |
| Bio-Plex Manager 6.2 Standard Software | Bio-Rad Laboratories, Inc | 171STND01 | Multiplex Manager Software |
| Butterfly Needle 21 G | BD | 367287 | |
| Cholera Toxin | Sigma | C8052 | |
| Crystal Violet | Merck | C6158 | |
| Cytofix/Cytoperm Solution | BD | 554722 | Fixation and Permeabilization Solution |
| Dispase II | Sigma | D4693 | Neutral Protease |
| DMEM/High Glucose | GE Healthcare Life Sciences | SH30243.01 | |
| DMEM/Nutrient Mixture F-12 | Gibco-Invitrogen | 11320033 | |
| dNTP Mix | Promega | U1515 | dNTP Mix |
| EMEM (w L-Glutamine) | ATCC | 30-2003 | |
| EVOM voltohmmeter device | WPI, Sarasota, FL, USA | 300523 | |
| FACS Lysing Solution | BD | 349202 | 1x Lysing Solution |
| Falcon tube 15 mL | CellStar | 188271 | 15 mL tube |
| Falcon tube 50 mL | CellStar | 227261 | 50 mL Tube |
| Fast Start Essential DNA Probes Master | Roche | 6402682001 | qPCR Master Mix |
| Ficoll Paque Premium | Research Instruments | 17544203 | Density Gradient Media |
| H3N2 (A/Aichi/2/1968) | ATCC | VR547 | |
| H3N2 M1 Forward Primer Sequence | Sigma | 5'- ATGGTTCTGGCCAGCACTAC-3' | |
| H3N2 M1 Reverse Primer Sequence | Sigma | 5'- ATCTGCACCCCCATTCGTTT-3' | |
| H3N2 NS1 Forward Primer Sequence | Sigma | 5'- ACCCGTGTTGGAAAGCAGAT-3' | |
| H3N2 NS1 Reverse Primer Sequence | Sigma | 5'- CCTCTTCGGTGAAAGCCCTT-3' | |
| Heat Inactivated Fetal Bovine Serum | Gibco | 10500-064 | |
| hNESPCs | Human Donors | NA | |
| Human Epithelial Growth Factor | Gibco-Invitrogen | PHG0314 | |
| Hydrocortisone | STEMCELL Techonologies | 7925 | Collected from nasal biopsies during septal deviation surgeries |
| Insulin | Sigma | I3536 | |
| Lightcycler 96 | Roche | 5815916001 | qPCR Instrument |
| Live/DEAD Blue Cell Stain Kit *for UV Excitation | Thermofisher | L23105 | Viability Stain |
| MILLIPLEX MAP Human Cytokine/Chemokine Magnetic Bead Panel II – Premixed 23 Plex | Merck Pte Ltd | HCP2MAG-62K-PX23 | Immunology Multiplex Assay |
| Mitomycin C | Sigma | M4287 | |
| M-MLV 5x Buffer | Promega | M1705 | RT-PCR 5x Buffer |
| M-MLV Reverse Transcriptase | Promega | M1706 | Reverse Transcriptase |
| N-2 supplement | Gibco-Invitrogen | 17502-048 | |
| NIH/3T3 | ATCC | CRL1658 | |
| Perm/Wash Buffer | BD | 554723 | Permeabilization Wash Buffer |
| PneumaCult-ALI 10x Supplement | STEMCELL Techonologies | 5001 | |
| PneumaCult-ALI Basal Medium | STEMCELL Techonologies | 5001 | |
| PneumaCult-ALI Maintenance Supplement (100x) | STEMCELL Techonologies | 5001 | |
| Random Primers | Promega | C1181 | Random Primers |
| Recombinant Rnasin Rnase Inhibitor | Promega | N2511 | RNase Inhibitor |
| RNA Lysis Buffer | Qiagen | Part of 52904 | |
| RPMI 1640 (w L-Glutamine) | ATCC | 30-2001 | |
| STX2 electrodes | WPI, Sarasota, FL, USA | STX2 | Electrode |
| T25 Flask | Corning | 430639 | |
| T75 Flask | Corning | 430641U | |
| TPCK Trypsin | Sigma | T1426 | |
| Trypan Blue | Hyclone | SV30084.01 | |
| Viral RNA Extraction Kit | Qiagen | 52904 | Viral RNA Extraction Kit |
| V-Shaped 96-well Plate | Corning | 3894 | |
References
- Monto, A. S. Vaccines and antiviral drugs in pandemic preparedness. Emerging Infectious Diseases. 12 (1), 55-60 (2006).
- Lightfoot, N., Rweyemamu, M., Heymann, D. L. Preparing for the next pandemic. The British Medical Journal. 346, 364 (2013).
- Gerdil, C. The annual production cycle for influenza vaccine. Vaccine. 21 (16), 1776-1779 (2003).
- Putri, W., Muscatello, D. J., Stockwell, M. S., Newall, A. T. Economic burden of seasonal influenza in the United States. Vaccine. 36 (27), 3960-3966 (2018).
- Mas-Coma, S., Jones, M. K., Marty, A. M. COVID-19 and globalization. One Health. 9, 100132 (2020).
- Guo, Y. R., et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status. Military Medical Research. 7 (1), 11 (2020).
- Guan, W. J., et al. Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine. 382, 1708-1720 (2020).
- van Wilgenburg, B., et al. MAIT cells are activated during human viral infections. Nature Communications. 7, 11653 (2016).
- Chien, Y. H., Meyer, C., Bonneville, M. Gammadelta T cells: first line of defense and beyond. Annual Review of Immunology. 32, 121-155 (2014).
- van Wilgenburg, B., et al. MAIT cells contribute to protection against lethal influenza infection in vivo. Nature Communications. 9 (1), 4706 (2018).
- Dias, J., Leeansyah, E., Sandberg, J. K. Multiple layers of heterogeneity and subset diversity in human MAIT cell responses to distinct microorganisms and to innate cytokines. Proceedings of the National Academy of Sciences of the United States of America. 114 (27), 5434-5443 (2017).
- Yan, Y., et al. Human nasal epithelial cells derived from multiple individuals exhibit differential responses to H3N2 influenza virus infection in vitro. Journal of Allergy and Clinical Immunology. 138 (1), 276-281 (2016).
- Luukkainen, A., et al. A co-culture model of PBMC and stem cell derived human nasal epithelium reveals rapid activation of NK and innate T cells upon Influenza A virus infection of the nasal epithelium. Frontiers in Immunology. 9, 2514 (2018).
- Tan, K. S., et al. RNA sequencing of H3N2 influenza virus-infected human nasal epithelial cells from multiple subjects reveals molecular pathways associated with tissue injury and complications. Cells. 8 (9), 986 (2019).
- Kim, N., et al. Effect of lipopolysaccharide on diesel exhaust particle-induced junctional dysfunction in primary human nasal epithelial cells. Environmental Pollution. 248, 736-742 (2019).
- Tan, K., et al. In vitro model of fully differentiated human nasal epithelial cells infected with rhinovirus reveals epithelium-initiated immune responses. Journal of Infectious Diseases. 217 (6), 906-915 (2018).
- Tan, K. S., et al. Comparative transcriptomic and metagenomic analyses of influenza virus-infected nasal epithelial cells from multiple individuals reveal specific nasal-initiated signatures. Frontiers in Microbiology. 9, 2685 (2018).
- Cytokine /Chemokine Panel II 96 Well Plate Assay. Millipore Corporation Available from: https://www.merckmillipore.com/SG/en/product/MILLIPLEX-MAP-Human-Cytokine-Chemokine-Magnetic-Bead-Panel-II-Premixed-23-Plex-Immunology-Multiplex-Assay (2020)
- Gamage, A. M., et al. Infection of human nasal epithelial cells with SARS-CoV-2 and a 382-nt deletion isolate lacking ORF8 reveals similar viral kinetics and host transcriptional profiles. PLoS Pathogens. 16 (12), 1009130 (2020).
- Zhao, X. N., et al. The use of nasal epithelial stem/progenitor cells to produce functioning ciliated cells in vitro. American Journal of Rhinology & Allergy. 26 (5), 345-350 (2012).

