Synthesis, Characterization, and Application of Superparamagnetic Iron Oxide Nanoprobes for Extrapulmonary Tuberculosis Detection
Summary
To improve serological diagnostic tests for Mycobacterium tuberculosis antigens, we developed superparamagnetic iron oxide nanoprobes to detect extrapulmonary tuberculosis.
Abstract
A molecular imaging probe comprising superparamagnetic iron oxide (SPIO) nanoparticles and Mycobacterium tuberculosis surface antibody (MtbsAb) was synthesized to enhance imaging sensitivity for extrapulmonary tuberculosis (ETB). An SPIO nanoprobe was synthesized and conjugated with MtbsAb. The purified SPIO-MtbsAb nanoprobe was characterized using TEM and NMR. To determine the targeting ability of the probe, SPIO-MtbsAb nanoprobes were incubated with Mtb for in vitro imaging assays and injected into Mtb-inoculated mice for in vivo investigation with magnetic resonance (MR). The contrast enhancement reduction on magnetic resonance imaging (MRI) of Mtb and THP1 cells showed proportional to the SPIO-MtbsAb nanoprobe concentration. After 30 min of intravenous SPIO-MtbsAb nanoprobe injection into Mtb-infected mice, the signal intensity of the granulomatous site was enhanced by 14-fold in the T2-weighted MR images compared with that in mice receiving PBS injection. The MtbsAb nanoprobes can be used as a novel modality for ETB detection.
Introduction
Globally, extrapulmonary tuberculosis (ETB) represents a significant proportion of tuberculosis (TB) cases. Nevertheless, ETB diagnosis is often missed or delayed because of its insidious clinical presentation and poor performance on diagnostic tests; false results include sputum smears negative for acid-fast bacilli, lack of granulomatous tissue on histopathology, or failure to culture Mycobacterium tuberculosis (Mtb). Relative to typical cases, ETB occurs less frequently and involves little liberation of the Mtb bacilli. In addition, it is usually localized at difficult-to-access sites, such as lymph nodes, pleura, and osteoarticular areas1. Thus, invasive procedures for obtaining adequate clinical specimens, which makes bacteriological confirmation risky and difficult, are essential2,3,4.
Commercially available antibody detection tests for ETB are unreliable for clinical detection because of their wide range of sensitivity (0.00-1.00) and specificity (0.59-1.00) for all extrapulmonary sites combined5. Enzyme-linked immunospot (ELISPOT) assays for interferon-γ, culture filtrate protein (CFP), and early secretory antigenic target (ESAT) have been used for diagnosing latent and active TB. However, the results vary between different disease sites for diagnosing ETB6,7,8. In addition, skin PPD (purified protein derivative) and QuantiFERON-TB frequently provided false negative results9. QuantiFERON-TB-2G is a whole blood immune reactivity assay, which does not require a specimen from the affected organ and this may be an alternative diagnostic tool6,10,11. Other diagnostic methods typically used for TB meningitis, such as polymerase chain reaction, are still too insensitive to confidently exclude clinical diagnosis12,13. These conventional tests demonstrate insufficient diagnostic information to discover the extrapulmonary infection site. Thus, novel diagnostic modalities are clinically required.
Molecular imaging aims at designing novel tools that can directly screen specific molecular targets of disease processes in vivo14,15. Superparamagnetic iron oxide (SPIO), a T2-weighted NMR contrast agent, can significantly enhance the specificity and sensitivity of magnetic resonance (MR) imaging (MRI)16,17. This new functional imaging modality can precisely sketch tissue changes at the molecular level through ligand-receptor interactions. In this study, a new molecular imaging probe, comprising SPIO nanoparticles, was synthesized to conjugate with Mtb surface antibody (MtbsAb) for ETB diagnosis. SPIO nanoprobes are minimally invasive to tissues and bodies under examination18,19. Furthermore, these nanoprobes can demonstrate precise MR images at low concentrations due to their paramagnetic properties. In addition, SPIO nanoprobes appear elicit least allergic reactions because the presence of iron ions is part of normal physiology. Here, the sensitivity and specificity of the SPIO-MtbsAb nanoprobes targeting ETB were evaluated in both cell and animal models. The outcomes demonstrated that the nanoprobes were applicable as ultrasensitive imaging agents for ETB diagnosis.
Protocol
All protocol regarding animal experiment follows the standard operating procedures for laboratory animal breeding in accordance with the National Institutes of Health Guidelines for the Care and Use of Laboratory Animals (8th Edition, 2011) and is approved by the institutional animal care and use committee.
1. SPIO nanoparticle synthesis
- Prepare dextran-coated iron oxide magnetic nanoparticles by vigorously stirring a mixture of dextran T-40 (5 mL; 50% w/w) and aqueous FeCl3×6H2O (0.45 g; 2.77 mmol) and FeCl2×4H2O (0.32 g; 2.52 mmol) solutions at room temperature.
- Add NH4OH (10 mL; 7.5% v/v) rapidly.
- Further stir the black suspension for 1 h; subsequently, centrifuge at 17,300 x g for 10 min and then remove the aggregates.
- Separate the final SPIO products from unbound dextran T-40 by gel filtration chromatography20.
- Load the reaction mixture (total volume = 5 mL) into a 2.5 cm × 33 cm column and elute with a buffer solution containing 0.1 M Na acetate and 0.15 M NaCl at pH 7.0.
- Collect the purified dextran-coated iron oxide magnetic nanoparticles in the void volume and assay the column eluates for iron and dextran at 330 and 490 nm by using hydrochloric acid and the phenol/sulfuric acid methods20, respectively.
2. SPIO-MtbsAb synthesis
- Synthesize SPIO-conjugated EDBE using previously reported methods21,22.
- Synthesize SPIO-EDBE-succinic anhydride (SA).
- Stir an alkaline solution (5 M NaOH; 10 mL)) of SPIO-EDBE and SA (1 g; 10 µmol) at room temperature for 24 h.
- Dialyze the solution with 20 changes of 2 L of distilled water using molecular porous membrane tubing (12,000-14,000 MW cutoff). 6 h for each change.
- Finally, add 100 μL of SPIO-EDBE-SA (4 mg/mL of Fe) to 400 μL of 4.5 mg/mL MtbsAb to synthesize SPIO-MtbsAb by using 1-hydroxybenzotriazole and (benzotriazol-1-yloxy) tripyrrolidinophosphonium hexafluorophosphate as catalysts and stir the solution at room temperature for 24 h.
- Finally, separate the solutions from the unbound antibody through gel filtration chromatography.
- Load the reaction mixture (5 mL) on 2.5 cm × 33 cm column and elute using a PBS buffer. Confirm Ab–nanoparticle complex (i.e., nanoprobe) using a bicinchoninic acid protein assay kit23.
3. Particle morphology observation and relaxation tier measurement
- Examine average particle size, morphology, and size distribution using transmission electron microscope at a voltage of 100 kV.
- Drop-cast the composite dispersion onto a 200-mesh copper grid and air dry at room temperature before loading it onto the microscope.
- Measure the relaxation time values (T1 and T2) of the nanoprobes using the NMR relaxometer at 20 MHz and 37.0 °C ± 0.1 °C.
- Calibrate the relaxometer before each measurement.
- Record the r1 and r2 values from the eight data points generated through inversion-recovery and the Carr-Purcell-Meiboom-Gill pulse sequence, respectively, to determine r1 and r2 relaxivities20.
4. Cell imaging
- Cultivate human monocytes THP-1 in RPMI 1640 with 10% fetal bovine serum, 50 µg/mL gentamycin sulfate, 100 units/mL penicillin G sodium, 100 µg of streptomycin sulfate, and 0.25 µg/mL fungizone in a 5% CO2 incubator at 37 °C.
- Incubate SPIO-MtbsAb nanoprobes (2 mM) with 106 colony forming units (CFU) of Mycobacterium bovis BCG preincubated with 1 × 107 activated monocytes in microcentrifuge tubes (1 mL) in a 5% CO2 incubator at 37 °C for 1 h.
- Centrifuge tubes at 200 x g and discard the supernatant. Redissolve pellets in the medium (200 µL).
- Scan the samples using a fast gradient echo pulse sequence (Repetition time (TR) = 500; Echo time(TE) = 20; Flip angle = 10°) through 3.0-T MRI to determine the nanoprobe's specificity and sensitivity21,22.
5. BCG (Bacillus Calmette–Guérin) inoculation
- Reconstitute the lyophilized vaccine or bacterial stock in Sauton's medium and then dilute the stock with saline until properly dispersed as previously described24.
- Inoculate a live attenuated strain of M. bovis BCG, obtained from ADIMMUNE (Taipei, Taiwan) (Connaught strain; ImmuCyst Aventis, Pasteur Mérieux) at a volume of 0.1 mL/mouse (i.e., 107 CFU) intradermally into the left or right dorsal scapular skin of mice, as described previously23. Inject saline into mice as negative control. Monitor animals daily after BCG inoculation.
- Sacrifice animals 1 month after bacteria inoculation using carbon dioxide euthanasia. Harvest the tissue from the intradermal inoculation site. Fix the tissue in 10% formalin and embed in paraffin for serial sections at 5-10 µm. Stain tissue sections with the hematoxylin/eosin and Ziehl-Neelsen stains for acid-fast bacteria24 and with Berlin blue for ferric iron25.
6. In vivo MRI
- Inject ketamine (80 mg/kg of body weight) and xylazine (12 mg/kg body weight) subcutaneously into mice for animal anesthesia.
- Inject SPIO-TbsAb probes (2 nmol/200 µL) into tail veins of mice. MR image mice before and immediately after probe injection and then every 5 min for 30 min to acquire T2-weighted fast spin-echo images (TR = 3000; TE = 90; field of view = 8).
- Quantitatively analyze all MR images using signal intensity (SI), a measurement of defined regions of interest in comparable locations of an Mtb granuloma center and the back muscle adjacent to a granulomatous area.
- Calculate relative signal enhancements using the SI measurement before (SIpre; control) and 0-3 h after (SIpost) injection of the contrast agents using the formula
[(SIpost – SIpre)/SIpre] × 100
where SIpre is the SI of the lesion on the pre-enhanced scan and SIpost is the SI of the lesion on the post-enhanced scan21,22.
Representative Results
SPIO-MtbsAb nanoprobe synthesis and characterization
SPIO nanoparticles were designed to conjugate with MtbsAb. The dextran stabilized on the surface of SPIO nanoparticles was crosslinked by epichlorohydrin. SPIO nanoparticles were subsequently incorporated with EDBE to activate primary amine functional groups at the dextran ends. SA was then conjugated to form SPIO-EDBE-SA. SPIO-MtbsAb nanoprobes formed in the final step through the conjugation of MtbsAb with SPIO-EDBE-SA in the presence of the coupling agents. The TEM image of SPIO-MtbsAb nanoprobes (Figure 1) demonstrates that the SPIO-MtbsAb nanoprobes had a well-dispersed appearance. The average size of the SPIO-MtbsAb nanoprobe core was 3.8 ± 0.4 nm (200 particle calculation).
In aqueous solution, the relaxivity values, r1 and r2, of the nanoprobes were 23 ± 3 and 151 ± 8 mM-1s-1, respectively, at 20 MHz and 37.0 °C ± 0.1 °C. The r1/r2 ratio of SPIO-MtbsAb nanoprobes was similar to that of Resovist; however, r1 and r2 of Resovist (26 and 164 mM-1s-1, respectively) were somewhat higher than those of SPIO-MtbsAb nanoprobes.
In vitro SPIO-MtbsAb nanoprobe characterization and imaging
First, we detected M. bovis BCG, an acid-fast bacteria, through Ziehl–Neelsen staining (Figure 2A). The bacteria were isolated and then cultured with probes containing ferric iron, identifiable through Berlin blue staining (Figure 2B). The Mtb-targeting degree of SPIO-MtbsAb nanoprobe was determined through T2-weighted MRI; negative enhancement was proportioned to the amount of probes attached to the bacterial cell. The decrease in the SI in the presence of the nanoprobes occurred in a concentration-dependent manner (Figure 2C). At 2, 1, and 0.5 mM, the nanoprobes conjugated with Mtb exhibited SIs of 97.67 ± 3.05, 131.67 ± 4.51, and 257.33 ± 5.03, respectively, all higher the SI of 90.75 ± 2.47 for 1 mM nonconjugated nanoprobe. Compared with PBS (SI = 1073.43 ± 13.62), almost no signal reduction was noted in the TB only group (SI = 957.33 ± 12.53). Thus, SPIO probes specifically targeted Mtb bacilli; moreover, on the enhanced MR images, the SI decreased with increase in the amount of SPIO nanoparticles.
Similarly, the reductions in SI on enhanced MR images were noted 1 h after the culturing of THP-1 monocytes with the nanoprobes. A significant reduction in the SI of the TB group was noted when 1 mM (SI = 225.33 ± 8.58) and 2 mM (SI = 104 ± 2.16) concentrations of the nanoprobes were employed compared with the groups administered with PBS only (SI = 1005.33 ± 16.74) or not administered with the nanoprobe (SI = 991 ± 8.98). MRI SI reduction in the Mtb groups for 1 and 2 mM nanoprobes was comparable to that in the positive 1 mM nanoprobe alone group (SI = 112.33 ± 3.68). According to the above results, the SPIO-MtbsAb nanoprobes could aid in monitoring the nanoprobe-activated THP-1 monocyte trafficking.
In vivo SPIO-MtbsAb nanoprobe imaging
After cell imaging, we determined the efficacy of in vivo MRI for ETB. SPIO-MtbsAb nanoprobes were intravenously injected to Mtb-infected mice. A clearly detectable MR signal was noted in the Mtb granulomatous area 0.5 h after injection; however, the highest SI to background was observed after 1 h of injection. A significant reduction in MR signaling was noted in the Mtb granulomatous area (Figure 3). SI was measured before (SIpre) and after (SIpost) contrast agent injection. One hour after probe injection, the T2-weighted enhancement of signal reduction at the Mtb granulamatous areas (Figure 3B) was approximately 14-fold higher than that at the control sites (Figure 3A; -1.68% ± 1.32% and -23.43% ± 7.24%; p < 0.001).
Histological and immunohistochemical evaluation of SPIO-MtbsAb nanoprobes
A subcutaneous granuloma was developed 1 month after infection in C57BL/6 mice. New blood vascularization was noted within these lesions along with lymphocyte and epithelioid-macrophage aggregates. The organized granuloma had grown progressively (Figure 4A). The correlation of TB lesions with SPIO-MtbsAb MR signals was further determined through the immunohistochemical reaction of Mtb surface antigen with anti-MtbsAb. Positive MtbsAb expression was revealed in the granulomatous areas (Figure 4B), with acid-fast bacilli staining positive at the lesion site (Figure 4C). Berlin blue, a ferric iron-positive stain, was used to determine the sensitivity of the probes to Mtb. Berlin blue-positive SPIO probe was found in the same location as MtbsAb (Figure 4D). All colocalized pairs were shown in Figure 4A-D.
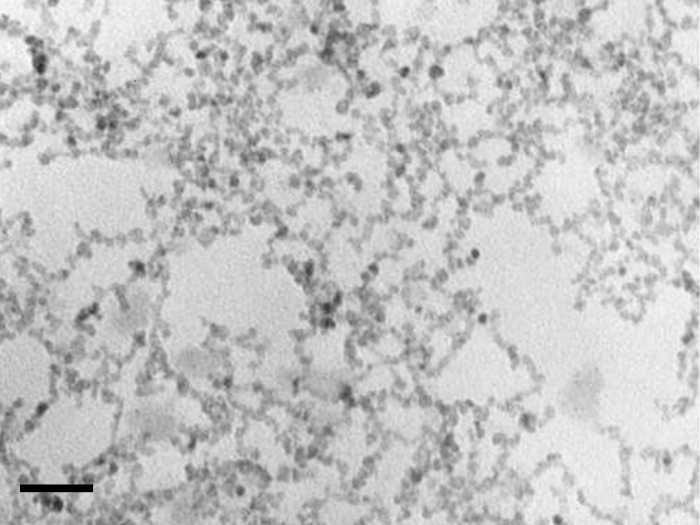
Figure 1: Mean core size of SPIO-MtbsAb nanoprobes in TEM. The average size of the SPIO-MtbsAb nanoprobe core was 3.8 ± 0.4 nm, measured using TEM image analysis (200 particle calculation). Scale bar = 15 nm. This figure has been modified from our previous study26. Please click here to view a larger version of this figure.
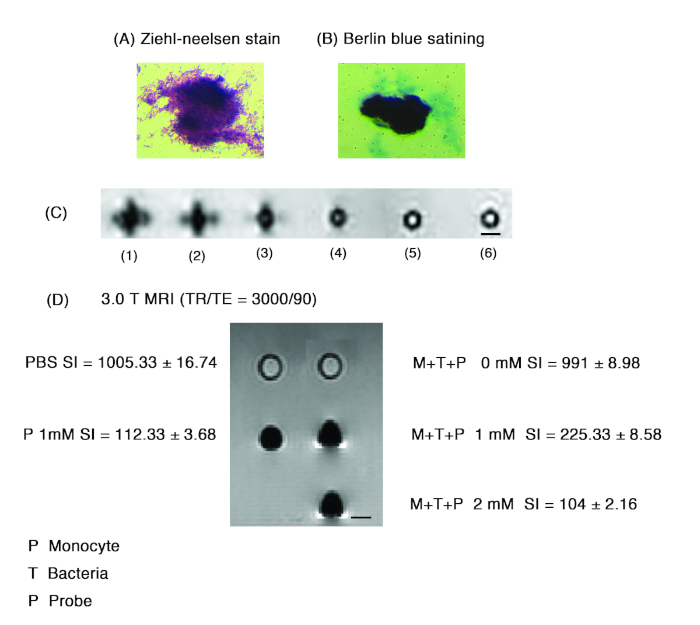
Figure 2: In vitro characterization of SPIO-MtbsAb nanoprobe. The acid-fast bacilli are identified through (A) Ziehl-Neelsen staining and (B) the conjugation of the ferric iron of the nanoprobe to bacteria identified through Berlin blue staining. (C) T2-weighted MRI displaying negative enhancement after the SPIO-MtbsAb nanoprobes are incubated with Mtb. Elimination of SI occurring dose-dependently after the incorporation of the nanoprobes with Mtb: (1) 90.75 ± 2.47 (1.0 mM Probe); (2) 97.67 ± 3.05 (Mtb + 2.0 mM Probe); (3) 131.67 ± 4.51 (Mtb +1.0 mM Probe); (4) 257.33 ± 5.03 (Mtb + 0.5 mM Probe); (5) 957.33 ± 12.53 (Mtb +0 mM Probe); (6) 1073.43 ± 13.62 (PBS). No detectable signal reduction noted in the PBS control group. (D) Dose-dependent negative enhancement in THP-1 monocytes 1 h after incubation with the nanoprobes. Scale bars in (C) and (D) are 5 mm. This figure has been modified from our previous study26. Please click here to view a larger version of this figure.
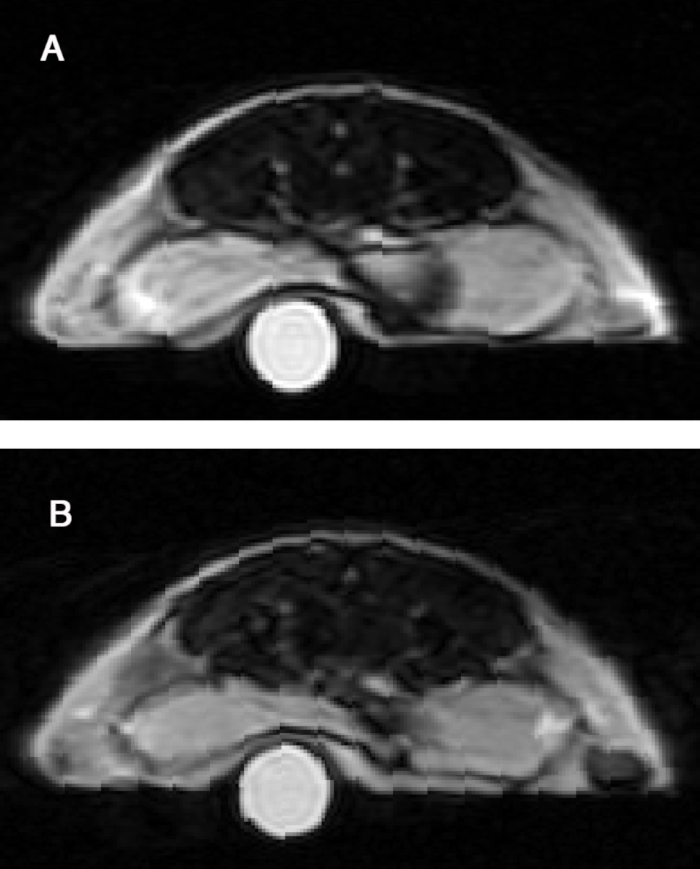
Figure 3: In vivo SPIO-MtbsAb nanoprobes in subcutaneous ETB lesions of C57BL/6 mouse. (A) Control and (B) Mtb granulomatous areas. A significant 14-fold reduction in MR signaling is found in the Mtb granulomatous areas compared with the control areas 1 h after probe administration (-1.68% ± 1.32% vs. -23.43% ± 7.24%, p < 0.001). Results are given as means ± SDs. Statistical comparisons used two-tailed Student's t-tests. p < 0.05 was considered to be significant. This figure has been modified from our previous study26. Please click here to view a larger version of this figure.
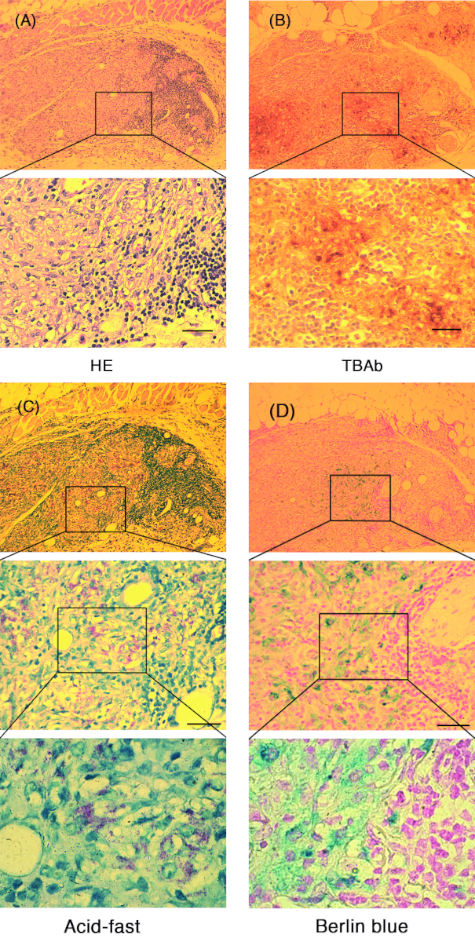
Figure 4: Correlations of histology, immunohistochemistry, acid-fast, and Berlin blue staining. Histology of Mtb granulomatous areas predominantly demonstrating lymphocytes and epithelioid macrophages. Neovascularization and abundant aggregation of lymphocytes and epithelioid macrophages observed in these lesions. (A) Organized granulomas appearing to develop progressively. (B) Immunohistochemical staining demonstrating MtbsAb expression in the granulomatous lesions, whereas (C) acid-fast bacilli are scattered within the same areas. (D) Berlin blue staining SPIO probes are found in the colocalized MtbsAb areas. Berlin blue staining for ferric iron demonstrates probe conjugation to Mtb. Scale bars are 100 µm. This figure has been modified from our previous study26. Please click here to view a larger version of this figure.
Discussion
Similar to relevant studies, our findings regarding SPIO-MtbsAb nanoprobes demonstrated a significant specificity for Mtb27,28. The subcutaneous Mtb granuloma was found 1 month after TB injection in the mouse models. The typical TB granulomatous histology findings included lymphocyte infiltration, presence of epithelioid macrophages, and neovascularization. Acid-fast bacilli were scattered in the TB lesions, corroborating the MtbsAb immunohistochemistry findings. This indicated an immunological reaction between Mtb surface antigen and MtbsAb. Berlin blue highlighted the same areas with MtbsAb, corroborating the probes' specificity for conjugation with acid-fast Mtb.
Notably, the extent of negative contrast enhancement on MRI for Mtb and monocytic THP1 cells was proportional to the SPIO-MtbsAb nanoprobe concentration. When mice bearing Mtb granulomas were administered SPIO-MtbsAb nanoprobes, a 14-fold signal reduction at the granulomatous site was noted on T2-weighted MR images compared to an opposing site with PBS injection. This indicates a significant accumulation of the contrast agent. The results demonstrate a possibility for obtaining specific targeting of contrast agent, which could reduce the dose requirement for clinical diagnosis.
Our findings indicate that these nanoprobes accumulate a detectable volume in Mtb granulomatous lesions. These results can be confirmed by developing an SPIO nanoprobe using anti-hMtbsAb. As the SPIO's magnetic iron oxide core has been applied to induce T2 shortening in MRI contrast agents, the findings suggest a practical and noninvasive approach to detect similar cell behaviors for clinical diagnosis applications.
Here, we provide the protocol comprising of 2 parts: sections 4 to 6 are cell and animal imaging. The techniques cover the cell cultivation, animal experiments, and optical imaging. Sections 1 to 3 are probe syntheses. Some critical steps will help to replicate the experiment. The critical step of SPIO nanoparticle synthesis is to prepare a dextran-coated iron oxide magnetic nanoparticles; it is crucial to vigorously stir and completely mix the dextran T-40, aqueous FeCl3-6H2O, and FeCl2-4H2O solutions at a room temperature. The critical step for section 2, SPIO-MtbsAb synthesis, is conjugating MtbsAb to SPIO-EDBE-SA to synthesize SPIO-MtbsAb. To select the appropriate catalysts and adequately stir the solution at room temperature are critical as well. And the critical step for section 3, Particle morphology observation and relaxation tier measurement, is to calibrate the relaxometer before each measurement. In order to precisely calculate the size of probes, a calibration of the relaxometer is crucial as well.
In this study, M. bovis BCG and rabbit anti-Mtb were used. The crossreactivity of bovine and rabbit sources was considered mild, although the data proved that MtbsAb-conjugated SPIO revealed strong interactions with M. bovis BCG. Our finding suggested that SPIO nanoprobes target TB specifically. The incubation of nanoprobe and Mtb bacteria showed a negative enhancement manner dose-dependently, while the decrease in the enhancement observed for SPIO nanoprobes on MRI was correlated with the existence of SPIO particles. Based on our data, further research to explore possible antibody-conjugation approaches to enhance the specificity of the nanoprobe would be welcome.
Prior studies demonstrate that SPIO shows minimal cytotoxicity without altering cell activity at a concentration used in this study29,30. In agreement with prior research, our results demonstrated minimal effect of SPIO nanoprobes to THP-1 cells. THP-1 cells were incubated with SPIO nanoprobes with bacteria conjugation for 1 hour. SI presented a significant decline in the Mtb groups with concentration of 1 mM or 2 mM nanoprobes, comparing to control group without nanoprobe treatment or PBS alone. The outcome supports the safety of the SPIO nanoprobe, and more studies applying other bacterial loads to validate the sensitivity of the nanoprobe is welcome.
One limitation of our study was that we did not quantify the biodistribution of the SPIO-MtbsAb nanoprobe in mice. Moreover, we did not investigate the intravascular halflife and liver deposition of the nanoprobe, which might alter the exposing time of the probes to THP-1 cells located at the Mtb lesions. Further research on biodegradation is warranted. Moreover, MRI could not differentiate whether SPIO nanoprobes could specifically bind to bacteria or monocytes or whether these probes were endocytosed.
In conclusion, we have developed a clear and feasible protocol to prepare and characterize biocompatible SPIO-MtbsAb nanoprobes. These nanoprobes are hydrophilic and disperse well under physiological conditions; they are minimally cytotoxic at low concentrations. Also, these SPIO-MtbsAb nanoprobes enable targeting and detection of Mtb infection, as demonstrated by our in vitro and in vivo studies. Thus, SPIO-MtbsAb nanoprobes can be applied as MRI contrast agents for ETB detection.
Disclosures
The authors have nothing to disclose.
Acknowledgements
The authors are thankful for the financial support from the Ministry of Economy Taiwan (grants NSC-101-2120-M-038-001, MOST 104-2622-B-038 -007, MOST 105-2622-B-038-004) to perform this research work. This manuscript was edited by Wallace Academic Editing.
Materials
| (benzotriazol-1-yloxy) tripyrrolidinophosphonium hexafluorophosphate | Sigma-Aldrich | ||
| 1-hydroxybenzotriazole | Sigma-Aldrich | ||
| dextran(T-40) | GE Healthcare Bio-sciences AB | ||
| epichlorohydrin, 2,2'-(ethylenedioxy)bis(ethylamine) | Sigma-Aldrich | ||
| ferric chloride hexahydrate | Fluka | ||
| ferrous chloride tetrahydrate | Fluka | ||
| Human monocytic THP-1 | |||
| M. bovis BCG | Pasteur Mérieux | Connaught strain; ImmuCyst Aventis | |
| MRI | GE medical Systems | 3.0-T, Signa | |
| NH4OH | Fluka | ||
| NMR relaxometer | Bruker | NMS-120 Minispec | |
| Sephacryl S-300 | GE Healthcare Bio-sciences AB | ||
| Sephadex G-25 | GE Healthcare Bio-sciences AB | ||
| SPECTRUM molecular porous membrane tubing, 12,000 -14,000 MW cut off | Spectrum Laboratories Inc | ||
| TB surface antibody- Polyclonal Antibody to Mtb | Acris Antibodies GmbH | BP2027 | |
| transmission electron microscope | JEOL | JEM-2000 EX II |
References
- Small, P. M., et al. Treatment of tuberculosis in patients with advanced human immunodeficiency virus infection. New England Journal of Medicine. 324, 289-294 (1991).
- Alvarez, S., McCabe, W. R. Extrapulmonary tuberculosis revisited: a review of experience at Boston City and other hospitals. Medicine. 63, 25-55 (1984).
- Ozbay, B., Uzun, K. Extrapulmonary tuberculosis in high prevalence of tuberculosis and low prevalence of HIV. Clinics in Chest Medicine. 23, 351-354 (2002).
- Ebdrup, L., Storgaard, M., Jensen-Fangel, S., Obel, N. Ten years of extrapulmonary tuberculosis in a Danish university clinic. Scandinavian Journal of Infectious Diseases. 35, 244-246 (2003).
- Steingart, K. R., et al. A systematic review of commercial serological antibody detection tests for the diagnosis of extrapulmonary tuberculosis. Postgraduate Medical Journal. 83, 705-712 (2007).
- Liao, C. H., et al. Diagnostic performance of an enzyme-linked immunospot assay for interferon-gamma in extrapulmonary tuberculosis varies between different sites of disease. Journal of Infection. 59, 402-408 (2009).
- Kim, S. H., et al. Diagnostic usefulness of a T-cell based assay for extrapulmonary tuberculosis. Archives of Internal Medicine. 167, 2255-2259 (2007).
- Kim, S. H., et al. Diagnostic usefulness of a T-cell-based assay for extrapulmonary tuberculosis in immunocompromised patients. The American Journal of Medicine. 122, 189-195 (2009).
- Pai, M., Zwerling, A., Menzies, D. Systematic review: T-cell-based assays for the diagnosis of latent tuberculosis infection: an update. Annals of Internal Medicine. 149, 177-184 (2008).
- Kobashi, Y., et al. Clinical utility of a T cell-based assay in the diagnosis of extrapulmonary tuberculosis. Respirology. 14, 276-281 (2009).
- Paluch-Oles, J., Magrys, A., Kot, E., Koziol-Montewka, M. Rapid identification of tuberculosis epididymo-orchitis by INNO-LiPA Rif TB and QuantiFERON-TB Gold In Tube tests: case report. Diagnostic Microbiology and Infectious Disease. 66, 314-317 (2010).
- Kaneko, K., Onodera, O., Miyatake, T., Tsuji, S. Rapid diagnosis of tuberculous meningitis by polymerase chain reaction (PCR). Neurology. 40, 1617 (1990).
- Bhigjee, A. I., et al. Diagnosis of tuberculous meningitis: clinical and laboratory parameters. International Journal of Infectious Diseases. 11, 348-354 (2007).
- Miyawaki, A., Sawano, A., Kogure, T. Lighting up cells: labelling proteins with fluorophores. Nature Cell Biology. , 1-7 (2003).
- Weissleder, R., Mahmood, U. Molecular imaging. Radiology. 219, 316-333 (2001).
- Gupta, A. K., Gupta, M. Synthesis and surface engineering of iron oxide nanoparticles for biomedical applications. Biomaterials. 26, 3995-4021 (2005).
- Talelli, M., et al. Superparamagnetic iron oxide nanoparticles encapsulated in biodegradable thermosensitive polymeric micelles: toward a targeted nanomedicine suitable for image-guided drug delivery. Langmuir. 25, 2060-2067 (2009).
- Cho, W. S., et al. Pulmonary toxicity and kinetic study of Cy5.5-conjugated superparamagnetic iron oxide nanoparticles by optical imaging. Toxicology and Applied Pharmacology. , 106-115 (2009).
- Mahmoudi, M., Simchi, A., Milani, A. S., Stroeve, P. Cell toxicity of superparamagnetic iron oxide nanoparticles. Journal of Colloid and Interface Science. 336, 510-518 (2009).
- Chen, T. J., et al. Targeted folic acid-PEG nanoparticles for noninvasive imaging of folate receptor by MRI. Journal of Biomedical Materials Research Part A. 87, 165-175 (2008).
- Chen, T. J., et al. Targeted Herceptin-dextran iron oxide nanoparticles for noninvasive imaging of HER2/neu receptors using MRI. Journal of Biological Inorganic Chemistry. 14, 253-260 (2009).
- Weissleder, R., et al. Ultrasmall superparamagnetic iron oxide: an intravenous contrast agent for assessing lymph nodes with MR imaging. Radiology. 175, 494-498 (1990).
- Wang, J., Wakeham, J., Harkness, R., Xing, Z. Macrophages are a significant source of type 1 cytokines during mycobacterial infection. Journal of Clinical Investigation. 103, 1023-1029 (1999).
- Angra, P., Ridderhof, J., Smithwick, R. Comparison of two different strengths of carbol fuchsin in Ziehl-Neelsen staining for detecting acid-fast bacilli. Journal of Clinical Microbiology. 41, 3459 (2003).
- Woods, A. E., Ellis, R. . Laboratory Histopathology- A Complete Reference. 1st edn. , 6-11 (1994).
- Lee, C. N., et al. Super-paramagnetic iron oxide nanoparticles for use in extrapulmonary tuberculosis diagnosis. Clinical Microbiology and Infection. 18, 149-157 (2012).
- Lee, H., Yoon, T. J., Weissleder, R. Ultrasensitive detection of bacteria using core-shell nanoparticles and an NMR-filter system. Angewandte Chemie International Edition. 48, 5657-5660 (2009).
- Fan, Z., et al. Popcorn-shaped magnetic core-plasmonic shell multifunctional nanoparticles for the targeted magnetic separation and enrichment, label-free SERS imaging, and photothermal destruction of multidrug-resistant bacteria. Chemistry. 19, 2839-2847 (2013).
- Nishie, A., et al. In vitro imaging of human monocytic cellular activity using superparamagnetic iron oxide. Computerized Medical Imaging and Graphics. 31, 638-642 (2007).
- von Zur Muhlen, C., et al. Superparamagnetic iron oxide binding and uptake as imaged by magnetic resonance is mediated by the integrin receptor Mac-1 (CD11b/CD18): implications on imaging of atherosclerotic plaques. Atherosclerosis. 193, 102-111 (2007).

