High-Speed Human Temporal Bone Sectioning for the Assessment of COVID-19-Associated Middle Ear Pathology
Summary
This article describes a technique for rapid human temporal bone sectioning that utilizes a microsaw with twin diamond blades to generate thin slices for rapid decalcification and analysis of temporal bone immunohistochemistry.
Abstract
Histopathologic analysis of human temporal bone sections is a fundamental technique for studying inner and middle ear pathology. Temporal bone sections are prepared by postmortem temporal bone harvest, fixation, decalcification, embedding, and staining. Due to the density of the temporal bone, decalcification is a time-consuming and resource-intensive process; complete tissue preparation may take 9-10 months on average. This slows otopathology research and hinders time-sensitive studies, such as those relevant to the COVID-19 pandemic. This paper describes a technique for the rapid preparation and decalcification of temporal bone sections to speed tissue processing.
Temporal bones were harvested postmortem using standard techniques and fixed in 10% formalin. A precision microsaw with twin diamond blades was used to cut each section into three thick sections. Thick temporal bone sections were then decalcified in decalcifying solution for 7-10 days before being embedded in paraffin, sectioned into thin (10 µm) sections using a cryotome, and mounted on uncharged slides. Tissue samples were then deparaffinized and rehydrated for antibody staining (ACE2, TMPRSS2, Furin) and imaged. This technique reduced the time from harvest to tissue analysis from 9-10 months to 10-14 days. High-speed temporal bone sectioning may increase the speed of otopathology research and reduce the resources necessary for tissue preparation, while also facilitating time-sensitive studies such as those related to COVID-19.
Introduction
Human temporal bone research provides an invaluable resource to study the pathology and pathophysiology of the inner and middle ear. Before the 19th century, little was known regarding otologic disease1,2,3. To better understand otologic disease and "rescue aural surgery from the hands of quacks," Joseph Toynbee (1815-1866) developed methods to study histologic sections of the human temporal bone3. This work was furthered by Adam Politzer (1835-1920) in Vienna and others across Europe during the remainder of the 19th century, who used temporal bone sections to describe the histopathology of many common conditions affecting the ear2,3,4.
The first human temporal bone laboratory in the United States was opened in 1927 at Johns Hopkins Hospital, where Stacy Guild (1890-1966) developed methods for temporal bone sectioning5,6. The methods developed by Guild consisted of a 9-10 month process that included postmortem harvest, fixation, decalcification in nitric acid, dehydration in ethanol, celloidin embedding, sectioning, staining, and mounting. Modifications to this technique were later made by Harold Schuknecht (1917-1996)7; however, the basic components of this process remain essentially unchanged.
The significant resources required to maintain a temporal bone laboratory have presented a challenge for temporal bone research and likely contributed to its declining popularity over the past 30 years4,8. A significant portion of temporal bone laboratory resources must be devoted to the 9-10 month process of temporal bone preparation. One of the most time-consuming steps in preparation is the decalcification of the temporal bone, which is the densest bone in the human body. Decalcification is typically performed in nitric acid or ethylenediaminetetraacetic acid (EDTA) and takes weeks to months while requiring the frequent changing of solutions7,9. Further, time-sensitive studies of the human ear, such as those related to the COVID-19 pandemic, may be hindered by this slow preparation process. This paper describes a technique for high-speed temporal bone sectioning that uses a diamond microsaw to generate thick sections that allow for rapid decalcification and tissue analysis within 10-14 days of temporal bone harvest.
Protocol
This protocol was developed with IRB (IRB00250002) approval and in accordance with institutional policies for the use of human tissue and infectious material. Each temporal bone donor provided written consent before death, or consent was obtained posthumously from the donor's family. See the Table of Materials for details about all materials, equipment, and software used in this protocol.
1. Temporal bone harvest
- Obtain local institutional review board (IRB) board approval, review institutional policies for the use of human and infectious material, and obtain consent for tissue donation before utilizing this protocol.
- Put on proper personal protective equipment (PPE) before working with tissue from COVID-19-positive temporal bone donors. Ensure that the PPE consists of an N-95 respirator and face shield (or alternatively a positive pressure air purification system), gown, and two pairs of gloves. Review techniques for properly donning and doffing PPE before beginning this protocol10.
- Harvest temporal bone tissue within 12-24 h of donor death. If the body is not refrigerated, ensure that the harvest occurs within 8 h of death.
- Harvest temporal bones during autopsy using the four-incision, block method by osteotome7.
- Following craniotomy, remove the brain and divide the cranial nerves to the internal auditory canal sharply.
- Make the first bony incision with the osteotome parallel to and just medial to the squamous portion of the temporal bone.
- Perform the second bony incision parallel to the first at the medial border of the temporal bone.
- Then, make the third incision 3-4 cm anterior and parallel to the petrous ridge.
- Make the fourth incision roughly parallel to the third, 2 cm posterior to the petrous ridge.
NOTE: Ensure that all incisions extend through the skull base. - Then, remove the temporal bone using sharp dissection to free the soft tissue attachment along the inferior edge of the specimen. If embalming is to be performed following temporal bone harvest, tie off the stump of the carotid artery.
- Harvest temporal bones during autopsy using the four-incision, block method by osteotome7.
2. Tissue fixation, decalcification, and sectioning
- Immediately place the tissue in 200-300 mL of 10% buffered formalin (formaldehyde) so that the tissue is fully submerged. Leave the tissue in formaldehyde for a minimum of 72 h at room temperature, changing the solutions daily. Store the tissue in an air-tight container and perform solution changes under a fume hood while wearing appropriate PPE to prevent virus spread.
NOTE: Following the 72 h fixation period, the specimens no longer need to be considered infectious. - Use a precision microsaw with twin diamond blades to cut each specimen into three "thick" sections to allow for more rapid tissue decalcification. Set the twin diamond blades to a distance of 5 mm, so that the central section of temporal bone is 5 mm thick. Ensure that the sections of tissue on either end are 3-5 mm thick.
- Place the thick sections in 200-300 mL of 23% w/w formic acid decalcifying solution for 7-10 days at room temperature, until the tissue is soft enough for paraffin embedding. Change the solutions daily. Check for adequate tissue decalcification by palpating the specimen, which should feel soft.
NOTE: Decalcification may also be verified by x-ray. - Rinse the specimens in running tap water for 24 h by placing them in a large beaker underneath a running faucet.
- Dehydrate the tissue in a series of alcohols of increasing concentration7. Submerge the tissue in 100-200 mL of 70% ethanol for 1.5 h, followed by three washes in 95% and 100% ethanol for 1.5 h each, respectively. Next, wash the tissue 3 x 1.5 h in Xylene.
- Embed the thick sections in paraffin, with four treatments of 45 min each.
- Use a cryotome to cut thin (10 µm) sections. Position the tissue so that the tissue is cut in the axial plane. Cut thicker (20 µm) sections if desired.
3. Immunohistochemistry and imaging
- If traditional hematoxylin and eosin staining is desired (not described here), perform staining before mounting the sections on glass slides7.
- Mount the sections on positively charged glass slides.
- Bake the slides on a hot plate at 60 °C for 20 min.
- Place the slides in a holder and submerge them in a commercial pretreatment solution containing an organic solvent (diethanolamine in this case) and ethanol to deparaffinize, rehydrate, and unmask the tissue.
NOTE: This step is necessary to achieve satisfactory results with immunohistochemistry for formalin-fixed and paraffin-embedded tissue. - Heat the slides in a pressure cooker on high pressure for 20 min.
- Place the slides in a humidified chamber and block the tissue with a commercial blocking solution.
- Probe the tissue sections with the primary antibody against angiotensin-converting enzyme 2 (ACE2; 1:50), transmembrane protease serine 2 (TMPRSS2, 1:1,000), and the Furin protease (1:250).
NOTE: The ACE2, TMPRSS2, and Furin antibodies are used because these proteins are believed to play a role in SARS-CoV-2 infectivity11,12, and this protocol sought to investigate the possible mechanisms by which SARS-CoV-2 may infect the middle ear13. - Treat with HRP-conjugated anti-rabbit secondary antibody (ACE2, Furin; 1:100 dilution) or anti-goat (TMPRSS2, 1:100 dilution) secondary antibody.
- Counterstain the slides with 70% hematoxylin in water.
- Acquire images on a light microscope with a mounted digital camera. Obtain images of the middle ear mucosa and Eustachian tube at 20x and 10x magnification, respectively.
Representative Results
Hematoxylin and eosin staining of the middle ear mucosa and Eustachian tube showed preservation of the middle ear mucosa and submucosal middle ear tissue following processing (Figure 1). Immunohistochemical images showed expression of the ACE2, TMPRSS2, and Furin proteins within the middle ear mucosa and Eustachian tube (Figure 1). The presence of these proteins within the middle ear provides a possible route by which SARS-CoV-2 may infect the respiratory epithelium within the middle ear11,12,13. Further, the expression of these proteins within the Eustachian tube may explain a route by which the virus enters the middle ear, traveling to the middle ear from the nasopharynx via the Eustachian tube.
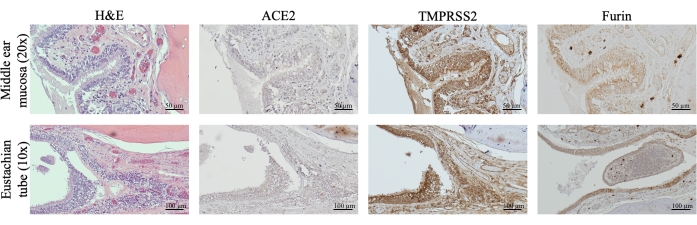
Figure 1: Example of stained middle ear tissue. The figure shows hematoxylin and eosin, ACE2, TMPRSS2, and Furin staining of the middle ear mucosa (top row, 20x magnification) and Eustachian tube (bottom row, 10x magnification). Scale bars = 50 µm (top row); 100 µm (bottom row). Abbreviations: H&E = hematoxylin and eosin; angiotensin-converting enzyme 2; TMPRSS2 = transmembrane protease, serine 2. Please click here to view a larger version of this figure.
Discussion
Human temporal bone research is critical for studying inner and middle ear pathology but remains a time- and resource-intensive endeavor. This paper describes a technique that uses a diamond microsaw to generate thick temporal bone sections that can be rapidly decalcified before further sectioning so that the time from tissue harvest to study can be reduced from 9-10 months to 10-14 days. This technique may reduce the resources required for temporal bone processing and facilitate time-sensitive studies, such as those related to COVID-19 middle and inner ear pathology13, which was the motivation for developing this protocol. This protocol allowed for the visualization of ACE2, TMPRS22, and Furin expression within the middle ear and Eustachian tube, providing a likely mechanism by which SARS-CoV-2 may infect the middle ear by spreading from the nasopharynx through the Eustachian tube.
The primary innovation of this protocol is the use of a diamond saw that cuts the tissue before decalcification, which generates "thick" sections of temporal bone that may be rapidly decalcified by increasing the surface area of the tissue exposed to the decalcifying agent. This step allows for tissue decalcification to occur within 7-10 days instead of the 1-2 months that traditional protocols may require for decalcification. The "thick" sections of tissue created with the diamond saw may also be dehydrated more quickly than a standard block of temporal bone tissue, thereby reducing the time between decalcification and embedding. Further, this protocol utilizes paraffin as an embedding agent rather than celloidin, which takes approximately 3 months to harden7. While celloidin provides superior preservation of cochlear structures, paraffin hardens much quicker and facilitates immunostaining. With these modifications, temporal bone tissue can be processed in 10-14 days as opposed to the 9-10 months required in more traditional processing strategies7,9.
This protocol has several limitations. Cutting the tissue with the diamond saw before embedding risks damaging the organ of Corti (OOC). The OOC was severely damaged in most specimens during the development of this technique, which may limit the value of this technique for studying pathologies such as age-related hearing loss, where it is vital that the delicate structures of the inner ear are preserved. It may be possible to position the specimen so that the diamond saw does not directly cut through the otic capsule bone and preserves inner ear structures, but this remains an area of active investigation. Animal models may provide a valuable tool to further refine this protocol and increase the chance of preserving inner ear structures in these valuable human specimens. Tissue quality in this protocol is additionally limited by the use of the paraffin-embedding agent, which was selected due to time constraints. Celloidin embedding better maintains cellular integrity in otopathologic specimens but takes months to harden7. Last, this protocol still requires significant time and resource investment. The use of a diamond microsaw is an additional cost to the materials required for traditional temporal bone preparation, and the 7-10 days required for decalcification is still lengthy. In the future, it may be possible to combine these methods with microwave-assisted decalcification14 to further shorten the time required for processing.
Despite its limitations, the protocol for high-speed temporal bone processing described here offers another tool for studying middle ear, and potentially inner ear, pathology. This technique has been useful during the COVID-19 pandemic and may also reduce the costs associated with maintaining an active temporal bone laboratory by reducing the time and labor necessary for tissue processing. Temporal bone research has decreased in popularity within the United States, decreasing from 28 active laboratories in the 1980s to only 4 active laboratories at present4. This decline in the number of operating temporal bone laboratories may be related to the significant costs associated with harvesting and processing temporal bones4,8. Consequently, it is important that we aim to develop techniques that reduce the resources necessary for temporal bone processing and also those that allow for the study of temporal bone pathology in new contexts, such as the COVID-19 pandemic. Further, high-speed tissue processing, such as that outlined in this protocol, may aid the use of new biologic techniques (e.g., immunohistochemistry, transcriptomics) that allow for the assessment of middle and inner ear pathology at the molecular level15,16,17,18,19. We have barely scratched the surface in terms of utilizing molecular techniques to study human tissue in otologic disease, and they may provide important insights that cannot be provided by animal models.
Disclosures
The authors have nothing to disclose.
Acknowledgements
We thank Mohamed Lehar for his assistance with this project. This work was partially supported by the National Institutes of Health (T32DC000027, NSA).
Materials
| Anti-ACE-2 Antibody (1:50 applied dilution) | Novus Biologicals | SN0754 | |
| Anti-Furin Antibody (1:250 dilution) | Abcam | EPR 14674 | |
| Anti-TMPRSS2 Antibody (1:1,000 dilution) | Novus Biologicals | NBP1-20984 | |
| BX43 Manual System Microscope | Olympus Life Science Solutions | ||
| CBN/Diamond Hybrid Wafering Blade | Pace Technologies | WB-007GP | |
| Collin Mallet – 8'' | Surgical Mart | SM1517 | |
| DS-Fi3 Microscope Camera | Nikon | ||
| Dual Endogenous Enzyme Block (commercial blocking solution) | Dako | S2003 | |
| Eaosin Stain | Sigma-Aldrich | 548-24-3 | |
| Formalin solution, neutral buffered 10% | Sigma-Aldrich | HT501128 | |
| Formical-4 Decalcifier (formic acid decalcifying solution) | StatLab | 1214-1 GAL | |
| Hematoxylin Stain | Sigma-Aldrich | H9627 | |
| HRP-Conjugated Anti-Rabbit Secondary Antibody (1:100 dilution) | Leica Biosystems | PV6119 | |
| ImmPRESS HRP Horse Anti-Goat igG Detection Kit, Peroxidase (1:100 dilution) | Vector Laboratories | MP-7405 | |
| Lambotte Osteotome | Surgical Mart | SM1553 | |
| Metallographic PICO 155P Precision Saw | Pace Technologies | PICO 155P | microsaw |
| NIS Elements Software Version 4.6 | Nikon | ||
| Paraplast Plus | Sigma-Aldrich | P3683 | paraffin |
| Positive Charged Microscope Slides with White Frosted End | Walter Products | 1140B15 | |
| Thermo Shandon Crytome FSE Cryostat Microtome | New Life Scientific Inc. | A78900104 | cryotome |
| Triology Pretreatment Solution (commercial pretreatment solution) | Sigma-Aldrich | 920P-05 | |
| Xylene | Sigma-Aldrich | 920P-05 |
References
- Nogueira, J. F., et al. A brief history of otorhinolaryngology: Otology, laryngology and rhinology. Brazilian Journal of Otorhinolaryngology. 73 (5), 693-703 (2007).
- Pappas, D. G. Otology through the ages. Otolaryngology-Head and Neck Surgery. 114 (2), 173-196 (1996).
- Schuknecht, H. F. Otopathology: The past, present, and future. Auris Nasus Larynx. 23, 43-45 (1996).
- Monsanto, R. D. C., Pauna, H. F., Paparella, M. M., Cureoglu, S. Otopathology in the United States: History, current situation, and future perspectives. Otology & Neurotology. 39 (9), 1210-1214 (2018).
- Crowe, S. J., Guild, S. R., Polvogt, L. M. Observations on the pathology of high-tone deafness. Journal of Nervous and Mental Disease. 80, 480 (1934).
- Andresen, N. S., et al. Insights into presbycusis from the first temporal bone laboratory within the United States. Otology & Neurotology. 43 (3), 400-408 (2022).
- Schuknecht, H. . Pathology of the Ear. , (1993).
- Chole, R. A. Labs in crisis: Protecting the science–and art–of otopathology. Otology & Neurotology. 31 (4), 554-556 (2010).
- Nager, G. T. . Pathology of the Ear and Temporal Bone. , (1993).
- . COVID-19 Personal Protective Equipment (PPE) Available from: https://www.cdc.gov/niosh/emres/2019_ncov_ppe.html (2022)
- Essalmani, R., et al. Distinctive roles of Furin and TMPRSS2 in SARS-CoV-2 infectivity. Journal of Virology. 96 (8), 0012822 (2022).
- Ueha, R., Kondo, K., Kagoya, R., Shichino, S., Yamasoba, T. ACE2, TMPRSS2, and Furin expression in the nose and olfactory bulb in mice and humans. Rhinology. 59 (1), 105-109 (2021).
- Frazier, K. M., Hooper, J. E., Mostafa, H. H., Stewart, C. M. SARS-CoV-2 virus isolated from the mastoid and middle ear: Implications for COVID-19 precautions during ear surgery. JAMA Otolaryngology – Head & Neck Surgery. 146 (10), 964-966 (2020).
- Cunningham, C. D., Schulte, B. A., Bianchi, L. M., Weber, P. C., Schmiedt, B. N. Microwave decalcification of human temporal bones. Laryngoscope. 111 (2), 278-282 (2001).
- Stephenson, R., et al. Immunohistochemical location of Na+, K+-ATPase α1 subunit in the human inner ear. Hearing Research. 400, 108113 (2021).
- McCall, A. A., et al. Extralabyrinthine manifestations of DFNA9. Journal of the Association for Research in Otolaryngology. 12 (2), 141-149 (2011).
- Wu, P. Z., O’Malley, J. T., de Gruttola, V., Liberman, M. C. Age-related hearing loss is dominated by damage to inner ear sensory cells, not the cellular battery that powers them. The Journal of Neuroscience. 40 (33), 6357-6366 (2020).
- Miller, M. E., Lopez, I. A., Linthicum, F. H., Ishiyama, A. Connexin 26 immunohistochemistry in temporal bones with cochlear otosclerosis. Annals of Otology, Rhinology & Laryngology. 127 (8), 536-542 (2018).
- Lopez, I. A., et al. Immunohistochemical techniques for the human inner ear. Histochemistry and Cell Biology. 146 (4), 367-387 (2016).

